Rhino-Orbital Mucormycosis in Diabetes Mellitus
Ravindra V. Shinde1, Geeta S. Karande2, S.T. Mohite3, S.R. Patil4
1 Assistant Professor, Department of Microbiology, Krishna Institute of Medical Sciences, Karad-415110, India.
2 Associate Professor, Department of Microbiology, Krishna Institute of Medical Sciences, Karad-415110, India.
3 Professor & Head, Department of Microbiology, Krishna Institute of Medical Sciences, Karad-415110, India.
4 Associate Professor, Department of Microbiology, Krishna Institute of Medical Sciences, Karad-415110, India.
NAME, ADRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravindra V. Shinde, Department of Microbiology, Krishna Institute of Medical Sciences, Karad-415110, India.
Phone: 09423005997
E-mail: dr.ravi910@gmail.com
Rhino-orbital mucormycosis is a rare but life threatening infection that generally occurs in patients with diabetes mellitus and other immune deficiency conditions. Rhino-orbital and Rhino-cerebral are two form of the disease. As such the condition is a medical emergency. Early recognition and treatment are essential because it may lead to death in few days. Fungal infection of nasal cavity is uncommon but is being seen with increasing frequency in patients with immune deficiency.
Diabetes mellitus, Mucormycosis, Rhizopus spp
CASE REPORT
A 55 years old male patient presented with a history of pain in the nose since eight days and inability in opening the right eye since one day. The pain was not relived. He was apparently all right 8 days prior. He was a known diabetic. On admission, he was found to be afebrile, conscious and well oriented to the time and place, with a BP of 160/90mmHg, a pulse of 82/min and with a swelling on the right side of the face. His other systems were normal. His fasting blood sugar was 164mg/dl, sodium was 12mEq/L, potassium was 2.5mEq/L., urea was 19mg/dl creatinine was 1.4mg/dl and haemoglobin was 11.7gm%. His total count was 23900/cumm, differential count was Neutrophils-88, Lymphocytes-10, monocytes-00, eosinophils-02, basophils-00/cumm and his platelet count was 4.65lacs/cumm. His urine specimen negative for acetone on admission. After 3 days, acetone was detected in his urine specimen. His nasal swab and maxillary and ethmoid sinus curettages were received in the microbiology laboratory for KOH mounts and fungal cultures to check for mucormycosis. An informed consent was obtained from the patient. The microscopic examination of the biopsy material and the nasal discharge was done in 10% KOH wet mounts. It showed the characteristic broad, aseptate, branched hyphae. The fungus was grown on Sabouraud’s dextrose agar at 370C with antibiotics but without actidione. The colonies were dense and had a white hairy appearance. A microscopic examination of the growth which was done in a lactophenol cotton blue mount, revealed that it was Rhizopus. The patient was started on an intravenous insulin infusion and amphotericin B at 0.3 mg/kg/day and this was gradually increased to 1mg/kg/day with the monitoring of the serum electrolytes and the renal functions. An ophthalmologic examination confirmed endophthalmitis and a right eye evisceration surgery was done. The left eye was normal, with a 6/6 vision. The patient took discharge against medical advice and died after two months.
DISCUSSION
Mucormycosis are a group of invasive infections which are caused by filamentous fungi of the order, Mucorales of the Mucoraceae Family. Rhino-orbital mucormycosis is an aggressive, angioinvasive fungal infection which is seen inimmunocompromised hosts. The risk factors are poorly controlled Diabetes mellitus, haematological malignancies and a prolonged corticosteroid treatment. The infections which are caused by members of the order mucorales are primarily opportunistic infections and they represent the third leading cause of invasive fungal infections following Aspergillus and Candida species. The most frequently isolated species is Rhizopusoryzae, followed by Rhizopus microsporeus and Absidia corymbifera [1].
Rhino-Orbital Mucormycosis (ROM) is a rare disease with an overall prevalence in 0.15% of the diabetics. However, rhino-orbital-cerebral mucormycosis, as a presenting manifestation, is rare [2]. Despite the advances in the diagnosis and treatment, a high mortality rate of 30-70% still exists for this disease. Death may occur within two weeks in untreated or unsuccessfully treated patients. It is an acute opportunistic infection which is caused by a broad, nonseptate, saprophytic fungus which is found in soil, air, bread mould, rotten fruit and vegetables.It can be cultured from the mouth, nasal tract, throat and the faeces of healthy persons. The fungus belongs to the Phycomycetes class, whose most common genera are Mucor, Rhizopus, Absidia and Basidiobolus. Contact with the micro organism occurs through spore inhalation. The infection spreads along the vascular and neuronal structures and it infiltrates the walls of the blood vessels. It causes erosion of the bony walls of the ethmoid sinuses and it may spread into the orbit and the retro-orbital area and in the brain (cerebro-rhino-orbital mucormycosis). Death may occur due to the cerebral abscesses. The infection with this organism usually complicates any underlying chronic disease, as in our patient. Commonly, mucormycosis attacks people with compromised immune systems. The reduced ability of serum to bind iron at a low pH may be the basic defect in the body’s defense systems. The high iron, glucose-rich acid milieu facilitates fungal growth. The human resistance to fungal infections rests on the body’s ability to restrict the availability of iron to the invading fungus, by binding it to proteins such as apotransferrin. The fungal hyphae produce a substance called rhizoferrin, which binds iron avidly. This iron-rhizoferrin complex is then taken up by the fungus and it becomes available for the vital intracellular processes. Diabetic patients are predisposed to mucormycosis because of the decreased ability of their neutrophils to phagocytose and adhere to the endothelial walls. Furthermore, the acidosis and hyperglycaemia provide an excellent environment for the fungus to grow [3]. In this case, the patient was a known diabetic and later on, he had developed ketosis. Initially, he had presented with pain in his right nose which was there since eight days, which had progressed to Rhino-Orbital Mucormycosis (ROM) within the next five days. It was followed by a periorbital swelling and an inability to open the mouth (facial weakness). The prognosis of mucormycosis has markedly improved over the past 30 years, with a 90% survival rate [2]. The factors which are related to a poor survival are delays in the diagnosis and treatment. The patient had foetal wastage within two months after taking discharge against medical advice from the hospital, which could be related to hyperglycaemia and his concomitant illness. Mucormycosis, also known as Zygomycosis or Phycomycosis, was first described by Paultauf in 1885, who coined the term ‘mycosis mucorina’. In 1943, three cases of rhinocerebral mucormycosis were reported in diabetic patients. The most pathogenic species of the family, Mucoraceae is Rhizopus. Rhizopus oryzae is the predominant pathogen which accounts for 60% of all the forms and 90% of the rhinocerebral cases [4]. In this case also, we isolated the Rhizopus oryzae species. Roden et al., [5] who reviewed 929 reports of zygomycosis in the English-language literature since 1885, found co-existing diabetes in 36% of the patients. Zygomycosis had caused death in 44% of them. However, Chakrabarti et al., [6] who analyzed 178 cases of Zygomycosis in hospitalized patients in northern India, found co-existing, uncontrolled diabetes in 73.6% of the patients. Moreover, Schwartz et al., [7] noticed that Cerebro-Rhino-Orbital Phycomycosis (CROP) which was mainly caused by Rhizopus spp, occurred predominantly in the individuals with diabetic ketoacidosis. CROP leads to proptosis, loss of vision, ophthalmoplegia and death which results from a cerebral involvement [Table/Fig-1,2,3&4].
Showing orbital swelling (deidentification done)

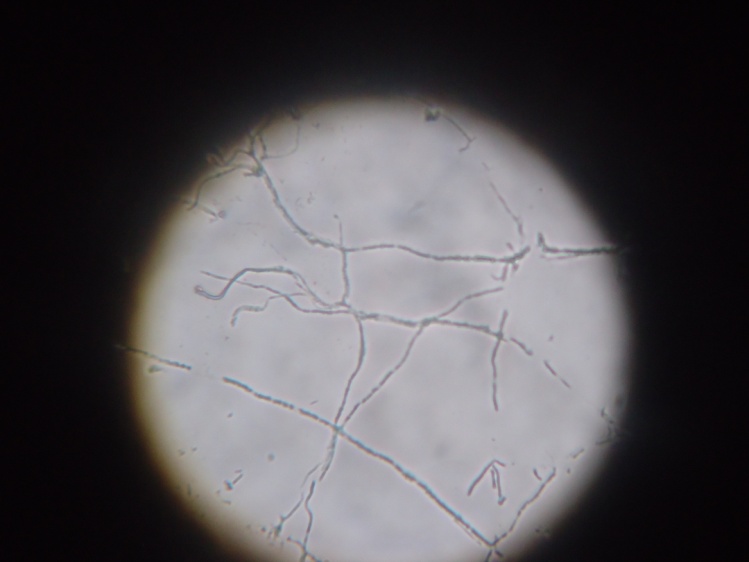
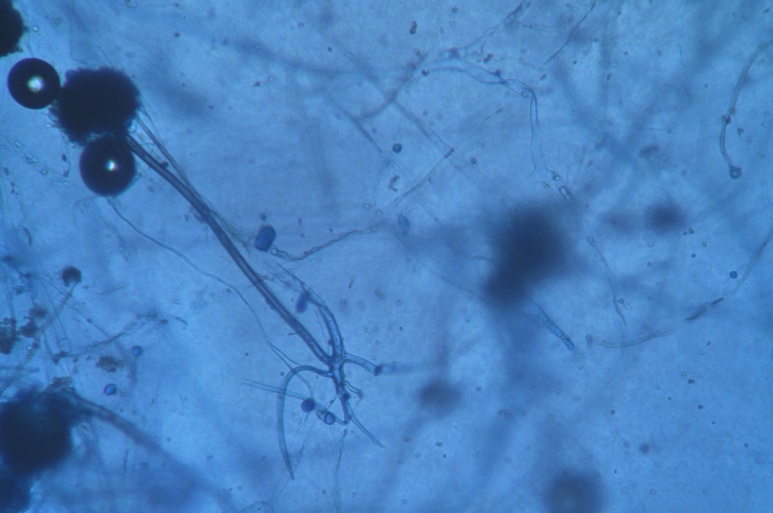
KOH Mount- Showing fungal element
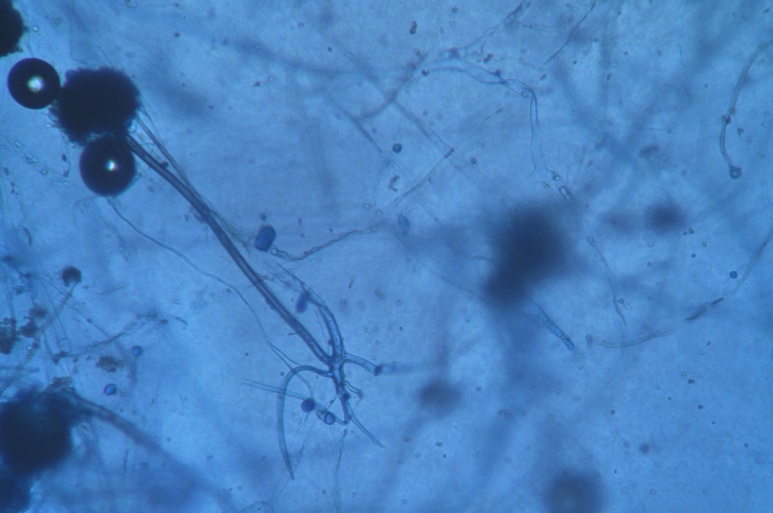
Showing growth on SDAJCDR
CONCLUSION
Mucormycosis remains a severe infectious disease in diabetic patients and it is characterized by a high mortality rate. The clinical diagnosis is often difficult and it gets delayed. It should be underlined that in diabetics, physicians should always pay special attention to the infections within the facial skeleton, especially which do not respond to antibiotic therapy. Aggressive diagnostic procedures are required for histo-microbiological studies to confirm this disease. An early diagnosis, combined with medical and surgical treatments, is necessary to improve the outcome.
[1]. Mallis A, Mastronikolis SN, Naxakis SS, Papadas AT, Rhinocerebral mucormycosis: an updateEuropean Review for Medical and Pharmacological Sciences 2010 14:987-92. [Google Scholar]
[2]. Hayat Mohd, Mushtak Syed, Saba Sameena, Saif Riyaz, Rhino-orbital-mucormycosis as presenting manifestation of gestational diabetes mellitusIndian journal of Endocrinology and Metabolism 2011 15(supplement 1):65-66. [Google Scholar]
[3]. Mathebula SD, Case report: Rhino-orbital mucormycosisThe South African optometrist 2006 65(2):78-81. [Google Scholar]
[4]. Ammari Lamia, Kilani Badreddine, Tiouiri Hanene, Mucormycose: Apropos de quatre observationsLa Tunisie Medicale 2008 86(2):165-68. [Google Scholar]
[5]. Roden MM, Zaoutis TE, Buchanan WE, Epidemiology and outcome of Zygomycosis : a review of 929 reported casesClin Infe Dis 2005 41:634-53. [Google Scholar]
[6]. Chakrabarti A, Das A, Mandal J, The rising trend of invasive Zygomycosis in patient with uncontrolled diabetes mellitusMed Mycol 2006 44:335-42. [Google Scholar]
[7]. Schwart JN, Donnelly EH, Kintworth GK, Ocular and orbital phycomycosisSurv Ophthalmol 1977 22:3-28. [Google Scholar]