An Interesting Case of Hypertriglyceridaemic Pancreatitis
Anupama K. Pujar1, Anil Kumar V. R.2, Sridhar M.3, Kulkarni S. V.4
1 Assistant Professor, MSRMC,
2 Associate Professor, MSRMC,
3 Assistant Professor, MSRMC,
4 Professor, M.S. Ramaiah Medical College, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anupama Pujar K, Assistant Professor, No 1165, 5th main, 4th block, Hbr Layout, Bangalore-560043, India.
Phone: 09740190687
E-mail: anupamapujar@rediffmail.com
Hypertriglyceridaemia is a well-known but uncommon cause of acute pancreatitis. A serum triglyceride level of more than 1000mg/dl is needed to precipitate the pancreatitis. A 35 year male patient, who was a known diabetic who was on oral hypoglycaemics, presented to us with pain in the abdomen and vomiting of one day’s duration. His serum amylase was normal. The serum was highly lactescent. The triglycerides were 1901mg/dl. CECT of the abdomen showed features which were suggestive of pancreatitis. The patient was managed just as the pancreatitis of any other eitiology. He was started on fibrates, atorvastatin, and antioxidants to prevent a relapse. His diabetes was controlled by insulin. He recovered well.
Hypertriglyceridaemia, Pancreatitis, Hyperlipidaemia
INTRODUCTION
Hypertriglyceridaemia is a rare cause of acute pancreatitis and it accounts for 1-4% of acute pancreatitis cases [1]. Serum triglyceride levels of more than 1000mg/dl are usually required to establish the diagnosis of hypertriglyceridaemic pancreatitis [1, 2]. The hypertriglyceridaemia may be primary or Secondary to alcohol, diabetes, pregnancy and drugs. The sera of these patients may be lactescent (4-20%) [3]. Types I, IV and V hyperlipidaemia (Fredrickson’s classification) is an identifiable risk factor [3]. The clinical course and the initial management are the same as that for pancreatitis which occurs due to other causes. Lifestyle modifications in terms of restricted fat in the diet and the use of fibrates effectively prevent a relapse. Insulin and heparin can be used to lower the hypertriglyceridaemia. The plasma triglycerides can also be lowered by plasmapheresis. Here, we are reporting a male patient who presented to us with the features of an acute abdomen, who was later diagnosed to have pancreatitis which was induced by hypertriglyceridaemia.
CASE REPORT
A 35 year old male patient presented to us with history of pain abdomen of one day’s duration. The pain was sudden in onset and it was more in the upper abdomen. There were no aggravating and relieving factors. The pain was associated with 3 episodes of vomiting, which contained food particles. He was a known diabetic who was on oral hypoglycaemic drugs.
On examination-the patient’s pulse rate was found to be 100/min, his blood pressure was 134/90mm of Hg, his respiratory rate was 18/min, the Spo2 was 96% in the room air and he was afebrile and mild dehydration was present. There was no eruptive xanthoma or lipaemia retinalis. On examination of his abdomen, tenderness and guarding were found to be present in the epigastrium. The rest of the abdomen was normal. There was no free fluid. His bowel sounds were normal. We made a working diagnosis of acute gastritis/acute pancreatitis on the basis of the above history and the clinical findings.
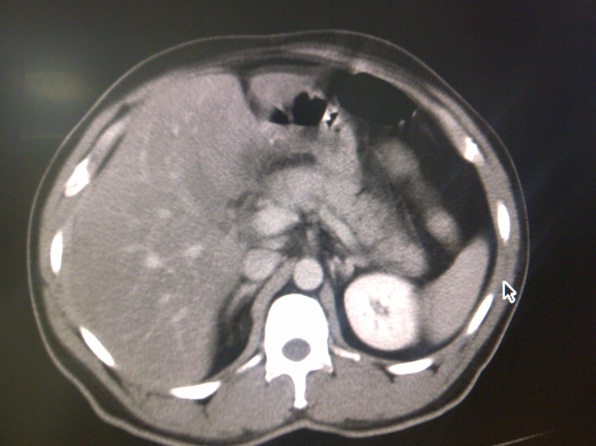
The patient was managed conservatively. His routine investigations were normal. An ultrasound of his abdomen showed fatty hepatomegaly. The serum amylase (61U/L) was within normal limits. Serum lipase was slightly elevated (77U/L). The LFT was normal. The patient’s serum was highly lipaemic. On estimation of his lipid profile, the serum triglyceride was found to be high (1901mg/dl) [Table/Fig-1]. LDL and VLDL couldn’t be calculated due to the high triglyceride levels. CECT showed a bulky pancreas with peripancreatic fat stranding and peripancreatic inflammatory fluid, especially around the head and the uncinate process of the pancreas. No pancreatic necrosis or calcification was seen. There was no dilatation of the pancreatic duct. Minimal thickening of the right perinephric fascia was noted [Table/Fig-2 & 3].
Lipid profile of patient on admission
| Test | Result | Reference range |
|---|
| Serum total Cholesterol(mg/dl) | 457 | <200-no risk 201-239 moderate risk >240 high risk |
| Serum Triglycerides(mg/dl) | 1901 | 0-200 |
| Serum HDL Cholesterol(mg/dl) | 18 | No risk female>65 male>55 Moderate risk- female 45-65, male 35-55 High risk female <45,male<35 |
| Total Cholesterol/HDL Cholestrerol Ratio | 25.4 | No risk : <5 |
Bulky pancreatic head with peripancreatic fat stranding

The patient was still on conservative management. His diabetes was controlled with insulin. The patient was put on fenofibrate, atorvastatin and anti-oxidants, since he was in the hypertriglyceri-daemia group. Once the patient recovered, he was counselled by a nutritionist regarding his fat restricted and sugar free diet. He was discharged with fenofibrate, atorvastatin, and oral hypoglycaemic drugs.
DISCUSSION
Hypertriglyceridaemia is a risk factor for acute pancreatitis, both as a precipitant and as an epiphenomenon. The risk is more so, when the triglyceride levels are more than 1000mg/dl. Our patient had a triglyceride level of 1901mg/dl. Hypertriglyceridaemia can be primary or secondary. Primary hypertriglyceridaemia is the result of various genetic defects which lead to a disordered triglyceride mechanism. The secondary causes are acquired causes such as a high fat diet, diabetes, obesity, hypothyroidism chronic renal disease and certain drugs like oestrogen, tamoxifen, thiazides, etc. [4]. In our patient, the family history of hyperlipidaemia was unknown and he was a diabetic who was on oral hypoglycaemic drugs.
Mild hyperlipidaemia is frequent in the early phase of acute pancreatitis of any aetiology (alcohol, gallbladder stone, etc.) in up to 47% of the cases [1]. To consider hypertriglyceridaemia as the cause of acute pancreatitis, the serum level should be more than 1000mg/dl [2, 5]. Our patient had hypertriglyceridaemia of more than 1000mg/dl.
The clinical presentation of acute hypertriglycerediaemic pancreatitis is similar to those of other causes of pancreatitis [6]. The clinical course doesn’t differ greatly from that of acute pancreatitis which occurs due to other causes. Our patient presented with acute pain abdomen and vomiting.
The severity and complication rates with hypertiglyceridaemic pancreatitis have been reported to be higher as compared to those of acute pancreatitis which occurs due to other aetiologies [7, 8]. The mortality rate does not differ [7]. The serum amylase levels may be spuriously low or they may be normal in 50% of the hypertriglyceridaemic pancreatitis patients at the time of their admissions or during their hospital courses, which is in contrast to those of hypertriglyceridaemia which occurs due to other causes [3]. This is because the hypertriglyceridaemia interferes with the calorimetric reading of the assay [2]. If the serum is diluted, then an increase in the amylase levels can be demonstrated. In our patient too, the serum amylase level was normal (61U/L). Lipase was insignificantly raised (77U/dl).
There are several mechanisms which have been described to explain hypertriglyceridaemic pancreatitis. The first one is direct damage of the pancreatic tissue by high levels of free fatty acids. High concentrations of the free fatty acids reduce the pH, which may activate trypsinogen. Secondly, the chylomicrons may damage the distal pancreatic blood circulation, thus inducing ischaemia. This change alters the acinar function and exposes the pancreatic tissue to the triglycerides. This activates the pancreatic lipase, which in turn induces inflammation and a sustained pancreatic enzyme activity. The third is a genetic decrease in the lipoprotein lipase activity. A study which was done by Chang et al., [9] has identified the specific genes which are associated with hypertriglyceridaemic pancreatitis. A cystic fibrosis transmembrane conductance regulator mutation/variant/haplotype and the tumour necrosis factor promotor polymorphism were both found to be independent risk factors for hyperlipaedimic pancreatitis in the Chinese population.
The initial management for this, remains the same as that for pancreatitis which occurs due to other causes. For a long term control and to prevent recurrent pancreatitis the secondary factors like the avoidance of alcohol, weight reduction, the control of diabetes and dietary restrictions with a low fat, low carbohydrate diet should be adopted. Fibrates form the mainstay of the hypertriglyceridaemia treatment [4, 10]. These fibrates can reduce the plasma triglyceride levels by up to 50% and raise the plasma HDL-C concentration to as much as 20% [4]. A fish oil supplementation may be added to augment the fibrate treatment. Statins are not a suitable monotherapy. However, when they are combined with fibrates, they may have a synergetic benefit [6]. Hypertriglyceredaemic pancreatitis has been treated with infusions of insulin, heparin or both [2]. Plasmapheresis is an effective method for a rapid lowering of the triglyceride levels in cases of severe hypertriglyceridaemia [11].
CONCLUSION
Hypertriglyceridaemia increases the risk of acute pancreatitis. The mechanism for hypertriglyceridaemic pancreatitis is postulated to involve the hydrolysis of Triglycerides by pancreatic lipase, which can induce a radical damage. The serum amylase levels are less contributory for the diagnosis. A high index of suspicion is necessary, particularly when risk factors are present. CECT is very important modality of imaging which can help in making a diagnosis. Life style modifications in terms of weight reduction, a fat restricted diet and a good control of diabetes are helpful for reducing the triglyceride levels. Fibrates prevents the relapse of hypertriglyceridaemic pancreatitis.
[1]. Khan A S, Latif S U, Eloubeidi M A, Controversies in Etiologies of Acute PancreatitisJOP. J Pancreas(online) 2010 Nov 9 11(6):545-52. [Google Scholar]
[2]. Tsuang W, Navaneethan U, Ruiz L, Palascak JB, Gelrud A, Hypertriglyceridemic pancreatitis Presentation and managementAm J Gastroenterol 2009 April 104:984-91. [Google Scholar]
[3]. Yadav D, Pitchumoni C S, Issues in hyperlipidemic pancreatitisJ. Clin. Gastroenterol 2003 Jan 36(1):54-62. [Google Scholar]
[4]. Yuan G, Al-Shali KZ, Hegele RA, Hypertriglyceridemia:its etiology, effects and treatmentCMAJ 2007 Aprill 176(8):1113-20. [Google Scholar]
[5]. Berglund L, Brunzell JD, Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guidelineJ Clin Endocrinol Metab 2012 sep 97(9):2969-89. [Google Scholar]
[6]. Lebenson J, Oliver T, Hypertriglyceride Induced Acute Pancreatitis, Prof. Luis Rod-rigo(ED), ISBN:978-953-307-984-84, In Tech [Google Scholar]
[7]. Navarro S, Cubiella J, Feu F, Zambon D, Hypertriglyceredemic Acute pancreatitis. Is its clinical course different from lithiatic acute pancreatitisMedicina Clinica 2004 123(15):567-70. [Google Scholar]
[8]. Ewald N, Hardt P D, Kloer H U, Severe hypertriglyceridemia and pancreatitis: presentation and managementCurr. Opin. Lipidol 2009 Dec 20(6):497-504. [Google Scholar]
[9]. Chang YT, Chang MC, Su TC, Association of cystic fibrosis transmembrane conduct ance regulator(CFTR) mutation/variant/haplotype and tumor necrosis factor(TFR) promotor polymorphism in hyperlipidemic pancreatitisClin Chem 2008 Jan 54:131-38. [Google Scholar]
[10]. Sandhu S, Al-Sarraf A, Incidence of pancreatitis, secondary causes, and treatment of patients referred to a specialty lipid clinic with severe hypertriglycedemia: a retrospective cohort studyLipids in Health and Disease 2011 Sept 10:157 [Google Scholar]
[11]. Ewald N, Kloer HU, Treatment options for severe hypertriglyceridemia (SHTG):the role of apheresisClin Res Cardiol Supp 2012 Feb 7:31-35. [Google Scholar]