An Ocular Prosthesis For A Geriatric Patient: A Case Report
Vikas B. Kamble1, Mukesh Kumar2, Debashis Panigrahi3
1 Professor and Head, Department of Prosthodontics, Crown and Bridge, P.M.N.M Dental College & Hospital, Bagalkot-587101, Karnataka, India.
2 Prosthodontist, Speciality Dental Clinic, Sitamarhi, Bihar, India.
3 Senior Lecturer, Department of Prosthodontics, Mansarovar Dental College and Hospital, Bhopal, India.
NAME, ADDRES, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vikas B. Kamble, Department of Prosthodontics, Crown and Bridge, P.M.N.M Dental College & Hospital, Bagalkot-587101, Karnataka, India.
Phone: +919970155404
E-mail: drvikaskamble2002@yahoo.co.in
When geriatric patients with maxillofacial defects are handled, the clinician must be confident of addressing and managing the psychology of these patients. It is also required that the clinician must understand and be sensitive to the medical and financial states of geriatric patients. The loss of an eye has a far-reaching impact on an individual’s psychology and an immediate replacement is necessary to promote the physical and psychological healing of the patient and to improve his/her social acceptance. Special approaches and treatment goals are considered while treating geriatric patients with ocular defects and special consideration is given to the appointment length, the number of appointments and their medical and financial statuses. This article presents the prosthetic rehabilitation of a geriatric patient with an ocular defect, with a customized stock ocular prosthesis, by using a minimal intervention geriatric approach.
Ocular prosthesis, Geriatric patient, Stock ocular prosthesis
CASE REPORT
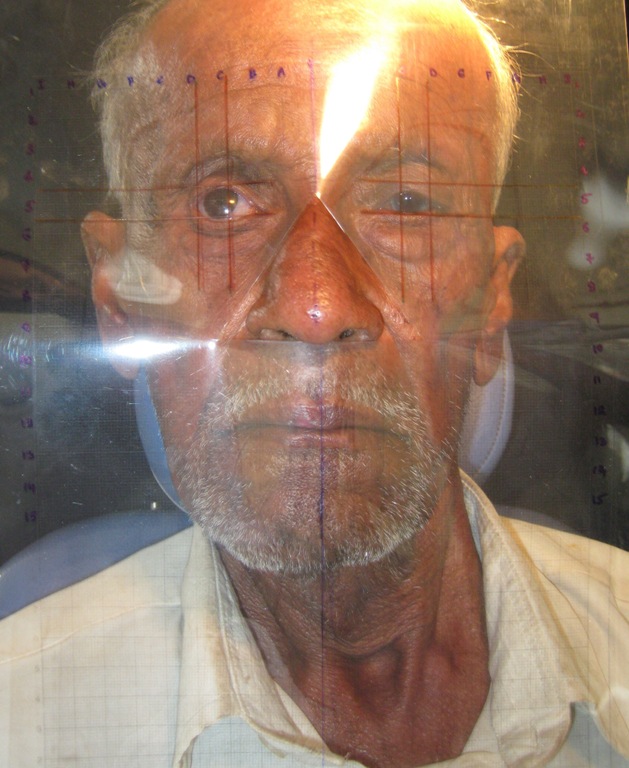
An 80 year old male patient reported to the Department of Prosthodontics, P.M.N.M Dental College, Bagalkot, Karnataka, India, for the prosthetic replacement of a missing right eye. His history revealed that his right eye was enucleated 2 years ago, following an infection, pain and discomfort after he underwent a cataract operation in a local village medical camp [Table/Fig-1]. On general examination, it was noticed that the conjunctiva which covered the posterior wall of the anophthalmic socket was healthy and that it elicited synchronous movements. There was adequate depth between the upper and lower fornices for the retention of the ocular prosthesis.
Geriatric patient with missing right eye

TREATMENT PLAN
The patient was unable to attend the prosthodontic clinic for a larger number of visits because of his age, financial status and general health condition and therefore, a customized stock ocular prosthesis was used to restore the ocular defect. The treatment plan was discussed with the patient and an informed consent was signed.
TECHNIQUE
The impression procedure
A medium body polyvinyl siloxane impression material (Aquasil, Dentsply Caulk, lot no-100901) was injected into the eye socket through a syringe, to which an acrylic tray was attached. The patient was asked to move his eye to the right and then to the left, then up and down and finally, in a circular motion, to obtain a functional impression of the defect. After the material was set, the impression was retrieved from the socket and it was examined for completeness or any voids [Table/Fig-2]. Boxing of the impression was done and the cast was poured in two layers to get a split cast by using a type III dental stone. (Gold stone, Asian chemicals, Gujarat, lot no-1959/200) [Table/Fig-3].
Impression of ocular defect


The wax pattern fabrication and positioning of the iris
A wax pattern was fabricated by allowing molten modeling wax to flow (Maarc,shiva product ,Mumbai, lot no-711) into the mold. A stock eye shell which matched the patient’s natural iris in colour and size was selected. The eye shell’s borders were trimmed so that it would be confined within the borders of the cast. A transparent graph grid was used to position the iris in the exact symmetrical placement on the defect side [Table/Fig-4].
Graph template used to orient the iris
The wax pattern try in
The wax pattern was tried in the patient’s ocular defect for comfort, stability, a proper orientation, motility and iris and sclera colours. The position, gaze and aesthetics of the prosthesis were shown to the patient and it got approved.
Flasking and curing
The wax pattern was invested in a type III dental stone in a crown flask to create a split mold. After dewaxing, 0.5–1mm of the surface layer of the scleral portion of the stock eye shell was trimmed. The characterization of the iris and shade matching of the sclera were done by using acrylic resin based pigments to match with the contralateral normal eye [Table/Fig-5]. Once the artwork was completed, heat cured clear acrylic resin (DPI, batch no-7102, 2010) was mixed and packed into the mold and a thin layer of it was also placed on the characterized sclera and the iris. The stock eye shell was put back into the mold and the flask was closed. The curing was done as per the manufacturer’s instructions. After the processing, the prosthesis was recovered and finishing and polishing were done to get a high shine. The prosthesis was disinfected and stored in water for 24 hours before its insertion.
Customized pre-fabricated eye shell

Insertion
The prosthesis was inserted into the eye socket and it was evaluated for aesthetics and the comfort of the patient. The patient was educated to insert and remove the prosthesis. Regular follow up appointments were given, along with instructions regarding the maintenance of the prosthesis [Table/Fig-6].
Geriatric patient with ocular prosthesis

DISCUSSION
Several techniques have been used for fitting and fabricating artificial eyes, like empirically fitting a stock eye (ocular shell prosthesis), [1] modifying a stock eye by making an impression of the ocular defect, [2] and the custom eye technique [3].
The disadvantages of the empirical fitting of an ocular shell is that, it leaves the vaulted spaces in the cavity and leads to accumulation of tears and mucous secretion, creating heaviness in the cavity and resulting in the dislodgement of the prosthesis from the cavity. Moreover, the aesthetics is also compromised, as the shades of the sclera and the iris do not exactly match those of the contralateral eye.
When the impression of the ocular defect is made and a custom made prosthesis is fabricated, then an intimate contact is achieved between the prosthesis and the tissue bed. The close adaptation of the custom-made prosthesis tends to distribute pressure more equally than does a stock eye prosthesis, thus helping in reducing the incidence of the conjunctival abrasion and ulceration. It also enhances the tissue health by reducing the potential fluid stagnation spaces at the prosthetic-tissue interface [4]. The custom made ocular prosthesis provides more aesthetic results because the iris and the sclera are custom fabricated and painted. The iris painting is one of the important steps in the fabrication of a custom-made ocular prosthesis. This technique is complex, it increases the treatment time, and it requires artistic skills, which are necessary in the iris painting. Moreover, the age, systemic conditions and financial constraints may limit their use.
If the stock prefabricated eye prosthesis is customized according to the patient’s contra lateral eye by using the acrylic resin pigments and if it is fabricated appropriately by making an impression of the ocular defect, then it can provide a satisfactory fit and aesthetic appearance for the patient. In the case of geriatric patients, such prostheses would be of immense use because of their relatively simple fabrication technique and as fewer appointments are required, thus aiding a minimal intervention approach for geriatric patients. The geriatric patient who is being presented here was rehabilitated by using the same technique, as this patient was unable to attend the prosthodontic clinic for a larger number of visits because of his age and general health condition. The easiest and the most effective way of rehabilitating geriatric patients with ocular defects, is mixing the professional treatment with a humane touch.
CONCLUSION
The clinicians who restore geriatric patients with ocular defects should provide professional services that are sensitive and caring. The use of a customized stock ocular prosthesis can provide an acceptable aesthetic result and it can also aid a minimal intervention geriatric approach in the rehabilitation of geriatric patients. It can also help their reintegration into the society by improving their psychology and quality of life.
[1]. Raizada Kuldeep, Rani Deepa, Ocular prosthesisContact Lens and Anterior Eye 2007 30:152-162. [Google Scholar]
[2]. Taicher S, Steinberg HM, Tubiana I, Sela M, Modified stock-eye ocular prosthesisJ Prosthet Dent 1985 54:95-8. [Google Scholar]
[3]. Benson P, The fitting and fabrication of a custom resin artificial eyeJ Prosthet Dent 1977 38:532-8. [Google Scholar]
[4]. Ow R.K.K., Amrith S, Ocular Prosthetics: Use of tissue conditioner material to modify a stock ocular prosthesisJ Prosthet Dent 1997 78:218-22. [Google Scholar]