Dilated Cardiomyopathy: An Anaesthetic Challenge
Haramritpal Kaur1, Ranjana Khetarpal2, Shobha Aggarwal3
1 Assistant Professor, Department of Anaesthesia, GGS Medical College and Hospital, Faridkot, India.
2 Assistant Professor, Department of Anaesthesia, GMC Medical College and Hospital, Amritsar, India.
3 Professor & Head, Department of Anaesthesia, GGS Medical College and Hospital, Faridkot, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Haramritpal Kaur, Department of Anaesthesia, GGS Medical College and Hospital, Faridkot, India.
Phone: 0091-9878088013
E-mail: amritk_dr@yahoo.co.in
Idiopathic dilated cardiomyopathy is a primary myocardial disease of unknown etiology characterized by left ventricular or biventricular dilation and impaired contractility. Depending upon diagnostic criteria used, the reported annual incidence varies between 5 and 8 cases per 100,000 populations. Dilated cardiomyopathy is defined by presence of: a) fractional myocardial shortening less than 25% (>2SD) and/or ejection fraction less than 45% (>2SD) and b) Left Ventricular End Diastolic Diameter (LVEDD) greater than 117% excluding any known cause of myocardial disease. Such cases are always a challenge to the anesthesiologist as they are most commonly complicated by progressive cardiac failure. We report the anesthetic management of a patient with dilated cardiomyopathy undergoing surgery for carcinoma breast.
Idiopathic, Dilated cardiomyopathy, Anaesthetic management
CASE HISTORY
A 54 years old female ,weighing 68kg having carcinoma left breast is scheduled for surgery. She was a known case of idiopathic dilated cardiomyopathy and had history of previous admissions to the hospital for episodes of congestive cardiac failure.
On preanaesthetic examination her heart rate was 72/min and regular. The systolic and diastolic blood pressures were 118mmHg and 68mmHg respectively. The respiratory rate was 16/min .There were no ronchi or rales on auscultation and heart sounds were normal. Jugular venous pressure was not raised and there was no hepatomegaly.
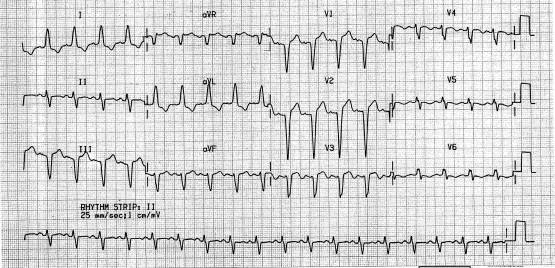
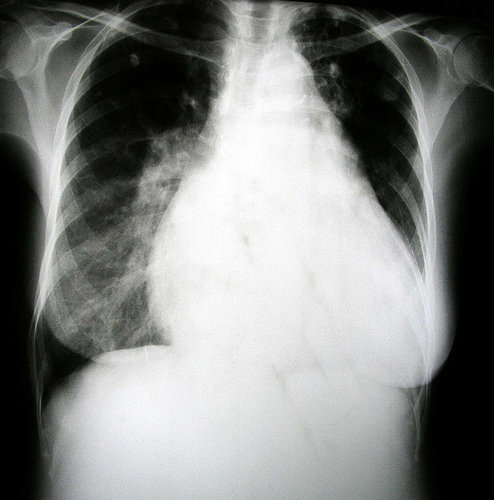
Preoperative 12 lead electrocardiograph (ECG) [Table/Fig-1] showed Left Bundle Branch Block (LBBB) and poor progression of R wave in leads V1-V5. X-Ray chest [Table/Fig-2] revealed cardiomegaly. The lung fields were clear.
ECG showing left bundle branch block and poor progression of R wave in lead V1-V5
Chest X-ray Showing dilated cardiomyopathy
Echocardiography reports demonstrated global hypokinesia of left ventricle, poor systolic function, ejection fraction of 25%, mitral regurgitation and left ventricular end diastolic dilatation.
She was on Losartan 25 mg OD, Spirinolactone 50 mg OD and Digoxin 0.125 mg OD for the last 2 years. All investigations including serum sodium, potassium, calcium and magnesium were with in normal limits.
A high risk consent was obtained and general anaesthesia was planned .No premedication was advised.
On the day of surgery, patient Blood Pressure (BP) was 118/80 mm Hg, Heart Rate (HR) was 70/min and oxygen saturation (SaO2) was 95% on room air. A right arterial line and right internal jugular central catheter was placed under local anaesthesia prior to the induction of anaesthesia. Other parameters monitored were ECG, end tidal carbon dioxide and oxygen saturation. Preloading with 250 ml of ringer lactate was done and anaesthesia was induced slowly with iv fentanyl 50ug, iv etomidate 30 mg and iv rocuronium 6mg. Lignocaine 60mg was given to blunt the hemodynamic response to intubation. The patient was intubated with cuffed endotracheal tube 7.5 mm ID (Internal Diameter). Anaesthesia was maintained with O2/N2O, isoflurane (MAC 1-1.5%) and intermitted rocuronium. Surgery was completed in 45 minutes. There was minimal response to intubation, her preintubation BP was 122/80 mmHg and HR was 72/min while post intubation BP was 130/84 mm Hg and HR was 80/min. Otherwise intraoperatively her mean arterial pressure was 65-75 mm Hg, heart rate 60-71 /min, SaO2 was 99-100%, CVP was 7-10 cm H2O, end tidal carbon dioxide was 33-37 mm Hg and airway pressure was 15-18 cm H2O. Intraoperatively patient had a fall of blood pressure to 72/45 and CVP was 5. Dopamine drip was started at the rate of 5ug/kg/min to maintain systolic blood pressure of 90. ECG tracing showed sinus rhythm with infrequent PVC (< 6/min) without ischemic changes. Injection paracetamol 1 gm intraoperatively was given for postoperative pain management. Total IV fluids included 500 ml of crystalloids and 500 ml colloid and her total urine output was 200 ml. Estimated blood loss was 250 ml. At the end of surgery, patient was kept electively intubated and shifted to intensive care unit to put on ventilator. By the next evening the dopamine drip was tapered off and patient was successfully weaned off from ventilatory support. The following day patient was discharged to surgical ward with stable hemodynamics.
DISCUSSION
Dilated Cardiomyopathy (DCM) is a syndrome characterized by cardiac enlargement and impaired systolic function of one or both ventricles. A large number of cases are idiopathic. The known causes are ischemic, valve dysfunction and post viral infection. DCM can also be found in association with sickle cell disease, muscular dystrophy, excess alcohol, hypothyroidism and some chemotherapy agents or during peripartum period.
Clinical picture of dilated cardiomyopathy may vary from only cardiomegaly to severe CHF [1]. Apart from CHF, dysarrhythmias and embolism are (systemic or pulmonary) also common [2]. Recent management include medical therapy with drugs for example vasodilator, diuretics or beta blockers and atrio-ventricular pacemakers for patients with incoordinate movements of heart chambers [3]. It is difficult to decide the optimal time for surgery but the medical control of heart failure for >1 week is desirable .
Goals of anaesthetic management consist of 1) Myocardial depression should be avoided 2) normovolemia should be maintained 3) Avoid overdose of drugs during induction as circulation time is slow. 4) Ventricular after load is avoided 5) avoid sudden hypotension when regional anaesthesia is a choice [2].
Anaesthetic management needs to be customized for those with left ventricular ejection fraction below 45%. Drugs like ketamine, etomidate and narcotics have minimal depressing effect on cardiac function and are used frequently [4]. Oxygen carrying capacity should be adequate. The main determinants of oxygen carrying capacity are cardiac output and hemoglobin. Therefore, hemoglobin should be maintained at higher level and 13-14gm/100ml has been recommended [5]. To improve cardiac output inotropes, biventricular synchronized pacing or an intra arotic balloon pump may be required. Skeletal muscle paralysis is to be provided by nondepolarizing muscle relaxant that lack significant cardiovascular effects.
Use of vasoactive or inotropic drugs may be required frequently to counteract the negative effects of the anaesthetics on cardiac function. Dopamine in appropriate dose range has positive inotropic, chronotropic and vasoconstrictive effects making it an ideal agent to negate adverse cardiovascular effects of anaesthetics. Anaesthesiologist should also be prepared to use lidocaine, Amidarone or defibrillation to treat the arrhythmias [6]. Arrhythmias occur when potassium and magnesium levels are decreased (as these patients are usually on diuretic therapy). These electrolytes should be assessed preoperatively and corrected as necessary [7].
If the patient is having pacemaker then inhibition of pacemaker function may occur in presence of Electromechanical Interference (EMI) as produced by myogenic electrical activity associated with Muscle fasciculation induced by suuccinylcholine. Continuous invasive hemodynamic monitoring is essential as electrocardiography is not reliable in presence of EMI [8]. Cautery may lead to EMI. Bipolar cautery is less hazardous than unipolar, although EMI can still occur.
The acceptable limit of decrease in blood pressure and heart rate for a patient depends upon underlying medical condition [9]. It is recommended that fluid therapy and pharmacological management be guided by the use of pulmonary artery catheterization and the determination of cardiac filling pressure [9]. Continuous monitoring of preload by Transesophageal Echocardiography (TEE) and of myocardial performance by cardiac output measurement (CCO) is also useful [10] but this was not available in our hospital so, we relied on central venous pressure.
Nerve blocks are a rational approach for appropriate surgery as they have minimal hemodynamic abrasion [6]. Epidural anaesthesia produces changes in the preload and after load that mimic pharmacological goals in the treatment of this disease [2]. Regional anaesthesia was not used in the present case as extensive sensory level of block was required.
CONCLUSION
Patients with dilated cardiomyopathy are a challenge to the attending anesthesiologist. These patients can be well managed by thorough preoperative assessment and medical management, formulating the good anesthetic plans and prompt diagnosis and management of complications.
[1]. Stevenson LW, Perloff JK, The Dilated cardiomyopathy: clinical aspectsCardiol Clin 1988 6:187-218. [Google Scholar]
[2]. Stoelting RK, Dierdorf SF, Cardiomyopathy. In: Stoelting RK (Ed)Anaesthesia and Coexisting Disease 1993 (3rd ed)New YorkChurchill Livingstone:97-102. [Google Scholar]
[3]. Molhoek SG, Bax JJ, Erven RV, Effectiveness of resynchronization therapy in patients with end stage heart failureAm J Cardiol 2002 90:379-83. [Google Scholar]
[4]. Schechter WS, Kim C, Martinez M, Anesthetic induction in a child with end-stage cardiomyopathyCan J Anaesth 1995 42:404-08. [Google Scholar]
[5]. Sharma R, Francis DP, Pitt B, Hemoglobin perdicts survival in patients with chronic heart failure: a sub study of the ELITE II trialEur Heart J 2004 25(12):1021-28. [Google Scholar]
[6]. Thiagrarajah PH, Thiagarajah S, Frost E, Anaesthetic considerations in patients with cardiomyopathiesMiddle East J Anesth 2009 20(3) [Google Scholar]
[7]. Cermuzynski L, Gebalska J, Wolk R, Hypomagnesemia in heart failure with ventricular Arrhythmias, beneficial effects of magnesium supplementationJ Intern Med 2000 247(1):78-86. [Google Scholar]
[8]. Senthuran S, Toff WD, Vuylsteke A, Solesburry PM, Menon DK, Implantable cardiac pacemaker and defibrillators in anaesthetic practice- Editorial IIIBr J Anaesth 2002 88:627-31. [Google Scholar]
[9]. Bernards Christopher M, Epidural and Spinal Anaesthesia. In:Clinical Anaesthesia 1996 3rd EditionLippincot Raven:665 [Google Scholar]
[10]. Oda T, Otani S, Yoshimura N, Preanaesthetic evaluation of cardiovascular reserve in a patient with dilated cardiomyopathyMasui 1996 45(4):491-95. [Google Scholar]