Bowel Block in Pancreatitis
Biggs Saravanan Ramachandran1, Mohammed Ali2, Sivakumar Palaniswamy3, Thangadurai Chinnaswamy4
1 Third Year DM Resident, Department of Medical Gastroenterology, Madras Medical College, Chennai, India.
2 Professor and HOD, Department of Medical Gastroenterology, Madras Medical College, Chennai, India.
3 Consultant Surgical Gastroenterology, Kumaran Hospital, Chennai, India.
4 Primary Care Physician, Kumaran Hospital, Chennai, India.
NAME, ADRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Biggs Saravanan Ramachandran, Department of Medical Gastroenterology, Madras Medical College, Park Town, Chennai-600003, India.
Phone: 9159666778
E-mail: rbiggs21@yahoo.com
Acute pancreatitis is a multisystem disorder which can result in a variety of complications. Vascular complications can occur commonly in acute pancreatitis. Splenic artery rupture, aneurysms; gastro duodenal artery aneurysms; splenic venous thrombosis; portal venous thrombosis and rarely, superior mesenteric venous thrombosis, are the vascular complications of pancreatitis. Ischaemic stricture of the small bowel can occur secondary to pancreatitis, but it is extremely rare. Hence, we are reporting this case of a proximal jejunal stricture which occurred secondary to the pancreatitis which was caused by a superior mesenteric thrombosis.
Pancreatitis, Small intestinal stricture, Mesenteric venous thrombosis
INTRODUCTION
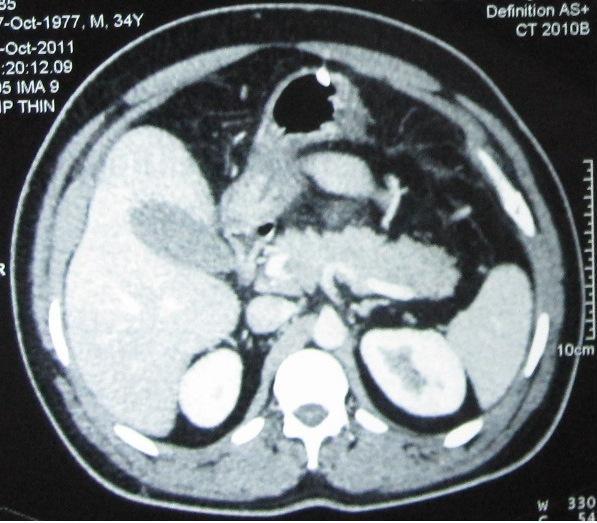
A 34 years old male who had a past history of acute pancreatitis 5 months ago, which required hospitalization and treatment, presented to our facility with abdominal pain in the epigastric region, which radiated to the back and recurrent vomiting of 2 days duration. He was a known heavy alcohol consumer since 10 years. There was no melena or hematochezia. The serum amylase was 540 U/L (reference range: 23-80 U/L) and lipase was 348 U/L (reference range: 0-60 U/L). The imaging findings of the pancreas were suggestive of pancreatitis [Table/Fig-1]. Additionally, they showed thrombosis of the superior mesenteric vein, which extended to the portal vein, with thickened oedematous proximal jejunal loops with a target pattern and convergence of the mesenteric vessels, which were suggestive of a mesenteric ischaemia [Table/Fig-2A and B]. His Protein C, S and anti thrombin III levels were normal. He was started on intravenous heparin for one week and was discharged on oral anticoagulants, as he became asymptomatic after seven days of hospitalization.
Thrombosis of superior mesenteric vein (lower arrow ) and portal vein (upper arrow)
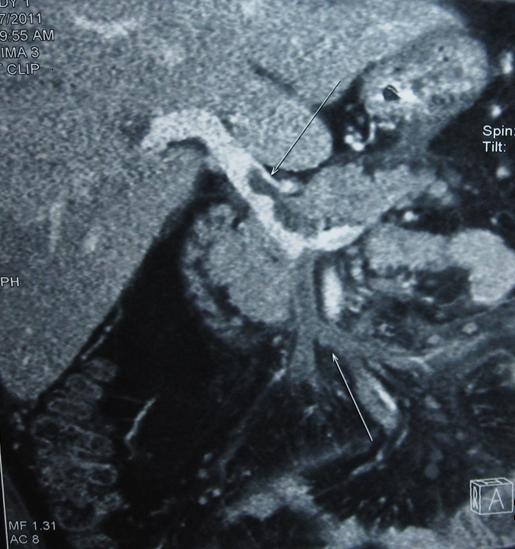
Showing target pattern (black arrow) and thickened jejunal loop with converging mesenteric vessels (white arrows)
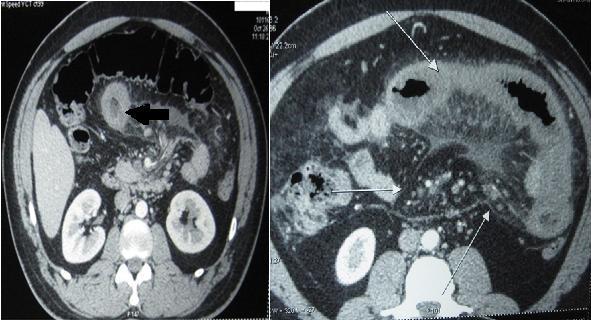
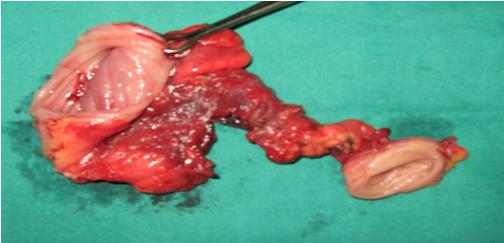
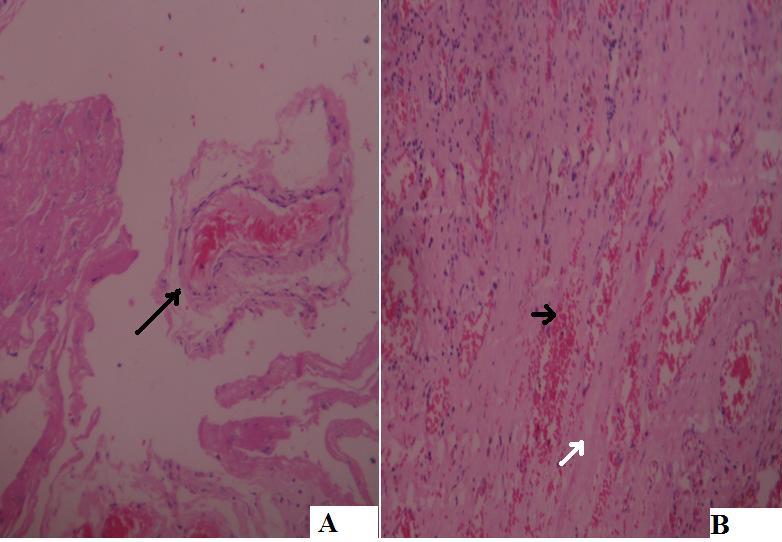
After 3 months, the patient again presented with recurrent vomiting and upper GI endoscopy, which showed excessive fluid in the second and third parts of the duodenum, which were suggestive of a distal obstruction. A Barium small bowel study showed a 5 cm stricture and a proximal dilatation in the proximal jejunum [Table/Fig-3]. Resection and primary end to end anastomosis were done. [Table/Fig-4] shows the resected specimen of the stricture, with a proximal dilatation. The histopathological examination of the resected specimen showed a thrombus inside a vein and fibrous tissue with congestion, which may be seen in venous ischaemia [Table/Fig-5A and B]. The patient is being followed up for the past six months and he is doing fine.
Barium study of small bowel showing 5 cm stricture in proximal jejunum (black arrow)

Surgical specimen showing stricture with proximal dilatation
(A) Histopathological examination of the stricture showing a thrombus inside a vein (black arrow) and (B) showing fibrous tissue (white arrow) with congestion (black arrow) which may be seen in venous ischemia.( Eosin hematoxylin stain with magnification X 40)
DISCUSSION
Acute pancreatitis is a multisystem disorder which is associated with a variety of complications. They can be roughly divided in to local and systemic complications. The local complications include pseudo cysts, pancreatic necrosis, pancreatic abscesses, gastro intestinal bleeding, splenic infarction and splenic rupture and various vascular complications like splenic artery aneurysms, aneurysm ruptures and splenic vein thrombosis, which lead to a variceal bleeding. The systemic complications include respiratory failure, renal failure, shock, hyperglycaemia, hypocalaemia, DIC, fat necrosis and retinopathy. Rarely, the patients may have psychiatric symptoms as well.Among the thrombotic complications of pancreatitis, isolated splenic vein thrombosis is fairly common and it is present in 10 to 40% [1] of the pancreatitis cases. Pseudoaneurysms are seen in 3.5-10% of the patients with pancreatitis [2]. A portal and a superior mesenteric venous thrombosis are less common [3]. The thrombosis which occurs due to intraabdominal causes like pancreatitis, starts in the larger vessels at the site of compression, which are caused by localized inflammatory processes or by pseudocysts and then progress peripherally to involve the smaller venous arcades and the arcuate channels. In contrast, the thrombosis which is caused by the underlying prothrombotic states, begins in the small vessels and it progresses to involve the larger vessels [4]. Pancreatitis per se, is also a prothrombotic condition. So, the venous thrombosis in pancreatitis is either caused by the localized inflammatory processes which affect the vein or by hypercoagulable states. Our case had 2 episodes of acute pancreatitis and during the second episode, he presented with mesenteric and partial portal venous thrombosis. After few months, he developed a proximal jejunal stricture which was secondary to the venous thrombosis, since the other common prothrombotic disorders were ruled out. The small intestinal strictures which occur secondary to pancreatitis are a rare occurrence. Only few case reports are available as of now [5]. We are reporting this case since it is rare and because the treating physicians should have an idea about this complication when they encounter recurrent vomiting after episodes of pancreatitis.
CONCLUSION
Small intestinal strictures can occur secondary to pancreatitis, either due to the hypercoagulable states which are associated with pancreatitis, which lead to ischaemic strictures or which are caused by a local inflammation. The ischaemic strictures which are secondary to pancreatitis may be included in the differential diagnosis of the cases with recurrent vomiting following pancreatitis.
[1]. Bernades P, Baetz A, Levy P, Splenic and portal venous obstruction in chronic pancreatitis. A prospective longitudinal study of a medical-surgical series of 266 patientsDig Dis Sci 1992 37:340-46.[PMID 1735356] [Google Scholar]
[2]. White AF, Baum S, Buranasiri S, Aneurysms secondary to pancreatitisAm J Roentgenol 1976 127:393-96.[PMID 183522] [Google Scholar]
[3]. Rattner DW, Warshaw AL, Venous, biliary, and duodenal obstruction in chronic pancreatitisHepatogastroenterology 1990 37:301-06.[PMID 2197206] [Google Scholar]
[4]. Kumar S, Sarr MG, Kamath PS, Mesenteric venous thrombosisN Engl J Med 2001 345:1683-88.(PMID:11759648) [Google Scholar]
[5]. Kato T, Morita T, Fujita M, Ischemic stricture of the small intestine associated with acute pancreatitisInt J Pancreatol 1998 24:237-42.(PMID: 9873959) [Google Scholar]