Management of an Endodontic Infection with an Extra Oral Sinus Tract in a Single Visit: A Case Report
Krishnamurthy Satish Kumar1, Arunajatesan Subbiya2, Paramasivam Vivekanandhan3, Venkatachalam Prakash4, Ramachandran Tamilselvi5
1 PG student, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India.
2 Professor, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India.
3 Professor, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India.
4 Professor, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India.
5 Senior Lecturer, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arunajatesan Subbiya, 35, 3rd Avenue, Indra Nagar Adyar, Chennai, India.
Phone: +919840197437
E-mail: drsubbiy@gmail.com
Chronic apical periodontitis can drain through a sinus tract, which may be intra-oral or extra-oral, though an intra-oral drainage is more common. Though such cases can be treated in a single visit, there is no report on a single visit endodontic treatment for a chronic apical periodontitis with a draining sinus. This case report demonstrates that the apical periodontitis with a cutaneous sinus tract can be successfully treated endodontically as a single visit procedure, if the patient is in good systemic health.
Extra oral sinus tract, Single visit endodontic treatment
INTRODUCTION
Single visit endodontics is gaining popularity over the traditional multi-visit endodontics because of various advantages. The advantages include a reduction in patient’s appointments per tooth, which would avoid an interappointment leakage, the immediate use of a canal for the retention of the posts, particularly in the anterior region (aesthetic consideration) and reduced procedural costs.
A chronic inflammation of pulpal origin is one of the reasons for an extra oral sinus of odontogenic origin [1]. Though, a draining sinus tract of odontogenic origin is one of the indications for single visit endodontics, the published case reports of such cases were of endodontics of two or more visits. An extra oral sinus tract from a lesion of endodontic origin is rare as compared to an intra oral sinus. An extraoral sinus tract of odontogenic origin is often diagnosed late, as the patient suspects it to be a skin lesion. If this is followed by a misdiagnosis from the general physician, it often takes weeks to months before it is referred to a dentist.
Conventionally, the root canal treatment was performed as a multiple visit procedure, as it was thought that the elimination of bacteria, and therefore its success, was possible only with a prolonged period of intra canal antimicrobial medicaments. But the healing potential for the teeth that are treated in one or two visits with the placement of an intra canal medicament appears to be similar [2–3]. The healing rate of single-visit and multiple-visit root canal treatments is also similar, even for infected teeth [4].Moreover, it has been found that the positive culture which is obtained just before the obturation, does not suggest the success of the endodontic treatment [5].
It has been suggested that the teeth with chronic apical periodontitis and a draining sinus tract can be endodontically treated by a single visit procedure [6]. This sinus tract may act as a safety valve for the residual inflammatory exudate. But a Cochrane systemic review showed that there was no study which had investigated fistulas or sinus tract formations with respect to a single-visit versus multiple-visit endodontic treatment [7]. The case which has been presented here is of a persistent extra oral sinus tract which originated from a necrotic pulp, which showed complete resolution following a single visit procedure.
CASE REPORT
A 33 years old female patient reported to our department with the chief complaint of a lesion on the face, in the zygomatic region [Table/Fig-1]. The patient gave a history of recurrence and remission of the fever for one month, for which she was treated by a general physician. Since there was a recurrence of the lesion and fever over and over again, she was referred to our dental institute for our opinion. On the day of the examination, the patient was afebrile. She was devoid of systemic diseases. On extraoral examination, an erythematous nodule was found, with continuous drainage on the right side of the cheek. The nodule was soft on palpation and it elicited a purulent discharge from it. Its history revealed that the lesion was present for the past 3 months, which was alternatively appearing and disappearing.

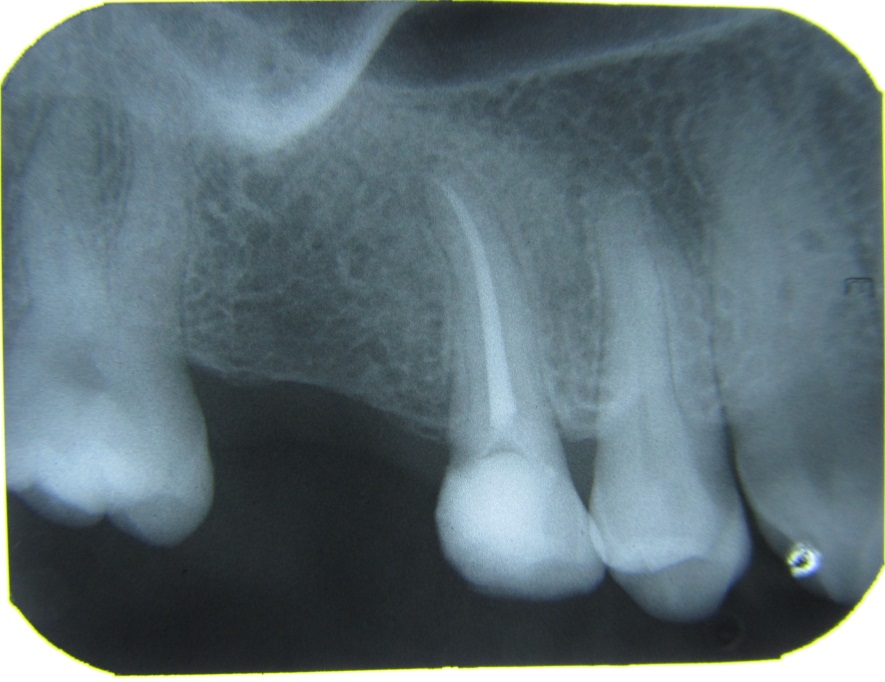
Intraorally, there was a carious lesion in the disto-occlusal aspect of the maxillary right second premolar with caries, which extended sub-gingivally in the distal aspect. The tooth was not tender on percussion and it did not respond to heat and electric pulp testing. On radiographic examination, it was found that there was an evidence of dental caries which involved the pulp in the disto-occlusal aspect of the crown and the periodontal ligament space, which widened in the apical third of the maxillary right second premolar [Table/Fig-2]. There was no definitive periapical radiolucency in that tooth. It was provisionally diagnosed as a non-vital maxillary second premolar with apical periodontitis and a draining extraoral sinus.

An endodontic treatment was initiated and the working length was determined by using an apex locator. The canal was cleaned and shaped. Irrigation of the root canal with saline resulted in the irrigant squirting out of the extra oral lesion, which confirmed that the lesion was a sinus tract with an odontogenic origin from the maxillary second premolar. As the saline was coming out through the extraoral lesion, chlorhexidine was preferred as an irrigant during the instrumentation procedure and not sodium hypochlorite, due to the risk of the apical extrusion of the irrigant. After an enlargement upto size 30 K-file, the canal was irrigated with saline and dried. A 30 size paper point was saturated with 5% NaOCl and it was left in the canal for 15mins to prevent the extrusion which could arise due to the irrigation. The canal was irrigated with saline, followed by chlorhexidine as a final irrigant. Chlorhexidine was left in the canal for 10 min to ensure complete disinfection. The canal was dried and obturated by the lateral condensation method [Table/Fig-3].

Follow Up
At the end of 1 week, there was a sign of healing of the extra oral lesion and in 2 weeks, there was a complete resolution of the extra oral lesion [Table/Fig-4]. In the follow up appointment in the sixth month, the patient was found to be asymptomatic and even the evidence of the extra-oral sinus had disappeared [Table/Fig-5 and 6].


6 months post-op radiograph
DISCUSSION
The purulent exudate of the odontogenic infection will move towards the path of the least resistance from the periapical area. Once the cortical plate has been penetrated, the sinus tract exits as an intraoral or extra oral sinus, depending on the location of the muscle attachments and the fascial sheaths. If the apices of the maxillary teeth are above the maxillary muscle attachments, and for the mandibular teeth below the mandibular muscle attachments, the spread of the infection may be extraoral [8–9]. These sinus tracts were originally thought to be lined by epithelium and therefore to require a surgical intervention apart from the endo-dontic treatment [10–11]. But later, studies suggested that it was lined by granulation tissue and not epithelium, which means that it could be intraoral or extraoral and that it could be treated by a non-surgical endodontic treatment [12].
Adequate measures which are used to eliminate the intracanal microorganisms would ensure a complete healing with a single visit endodontic treatment. Various studies have proved that chlorhexidine and sodium hypochlorite were the best among the irrigants, as they could reduce the bacterial counts rapidly [13–14]. Both these irrigants eliminate the gram positive and the gram negative anaerobic bacteria in 15 minutes [15]. Complete healing of the extraoral sinus indicates the adequacy of the disinfection procedure and it confirms the existing opinion of the management of such an endodontic infection as a single visit procedure. Though a single visit endodontic treatment is indicated in situations with draining sinus tracts, the treatment of the cases with extraoral sinuses is not attempted in single visit. This is probably because of the assumption that the intraoral and extraoral sinuses are different entities. But, this case report establishes that an endodontic infection with an extraoral sinus can also heal with a single visit endodontic treatment.
CONCLUSION
In conclusion, the presented case report demonstrates a conservative single visit endodontic management which resulted in the elimination of a cutaneous sinus tract of endodontic origin in a patient with a good host response.
[1]. Bender IB, Seltzer S, The oral fistula: Its diagnosis and treatmentOral Surg Oral Med Oral Pathol 1961 14:1367-76. [Google Scholar]
[2]. Trope M, Delano EO, Orstavik D, Endodontic treatment of teeth with apical periodontitis: single vs. multivisit treatmentJ Endod 1999 25:345-50. [Google Scholar]
[3]. Weiger R, Rosendahl R, Löst C, Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesionsInt Endod J 2000 33:219-26. [Google Scholar]
[4]. Su Y, Wang C, Ye L, Healing rate and post-obturation pain of single- versus multiple-visit endodontic treatment for infected root canals: A systematic reviewJ Endod 2011 37:125-32. [Google Scholar]
[5]. Peters LB, Wesselink PR, Periapical healing of endodontically treated teeth in one and two visits obturated in the presence or absence of detectable microorganismsInt Endod J 2002 35:660-67. [Google Scholar]
[6]. Cohen S, Pathways of the pulp6th ednSt. Louis, MissouriSamuel O. Dorn, Arnold HGartner, 72 [Google Scholar]
[7]. Figini L, Lodi G, Gorni F, Gagliani M, Single versus multiple visits for endodontic treatment of permanent teeth: A Cochrane systematic reviewJ Endod 2008 34:1041-47. [Google Scholar]
[8]. McWalters GM, Alexander JB, del Rio CE, Knott JW, Cutaneous sinus tracts of dental etiologyOral Surg Oral Med Oral pathol 1988 66:608-14. [Google Scholar]
[9]. Kotecha M, Browne MK, Mandibular sinuses of dental originPractitioner 198 225:910-15. [Google Scholar]
[10]. Thoma KH, Oral Surgery 1963 4th ednSt Louis, USAMosby:733 [Google Scholar]
[11]. Harrison JW, Larson WJ, The epithelized oral sinus tractOral Surg Oral Med Oral Pathol 1976 42:511-17. [Google Scholar]
[12]. Grossman LI, Endodontic Practice 1981 10th ednPhiladelphia, PALea and Febiger:84-111. [Google Scholar]
[13]. Siqueira JF Jr, Batista MM, Fraga RC, de Uzeda M, Antibacterial effects of endodontic irrigants on black pigmented Gram-negative anaerobes & facultative bacteriaJ Endod 1998 24:414-16. [Google Scholar]
[14]. Jeansonne MJ, White RR, A comparison of 2.0% chlorhexidine gluconate and 5.25% sodium hypochlorite as antimicrobial endodontic irrigantsJ Endod 1994 20:276-78. [Google Scholar]
[15]. Spratt DA, Pratten J, Wilson M, Gulabivala K, An in vitro evaluation of the antimicrobial efficacy of irrigants on biofilms of root canal isolatesInt Endod J 2001 34:300-07. [Google Scholar]