Chikungunya is an arthropod born arboviral infection. The Chikungunya virus is an RNA virus that belongs to the alpha virus genus of the Togaviridae family. The name 'Chikungunya' has been derived from a root verb in the Kimakonde language, which means, "that which bends up" i.e. which becomes contorted.The name reflects the stooped appearance of the sufferers due to arthralgia [1]. Epidemics of fever, rashes and arthritis which resembled Chikungunya fever were recorded as early as in 1824 in India and elsewhere [2]. However, the virus was first isolated in 1952-53 in Tanzania from both man and mosquitoes during an epidemic of fever [3].
There was an outbreak of this disease in Kolkata in 1963-64. In that outbreak, a total of 38 cases were reported, among which the virus was isolated from 35 patients and the sera of 3 more patients were positive for this virus [4]. A t that time, the outbreak occurred in south India [5] also;10 years later, in 1973, an epidemic of Chikungunya broke out in Barshi, Solapur district [6]. After 32 years, the state of Maharashtra experienced a large number of outbreaks of Chikungunya in the year 2006. A similar rise in the cases was also witnessed by the nearby states, i.e. Karnataka, Andhra Pradesh, and Tamil Nadu [7]. We conducted a cross sectional study in the affected village Kasegaon, District Sangli, with the objectives of studying the magnitude of the outbreak and of identifying the possible socio-environmental factors which are responsible for Chikungunya fever.
MATERIAL AND METHODS
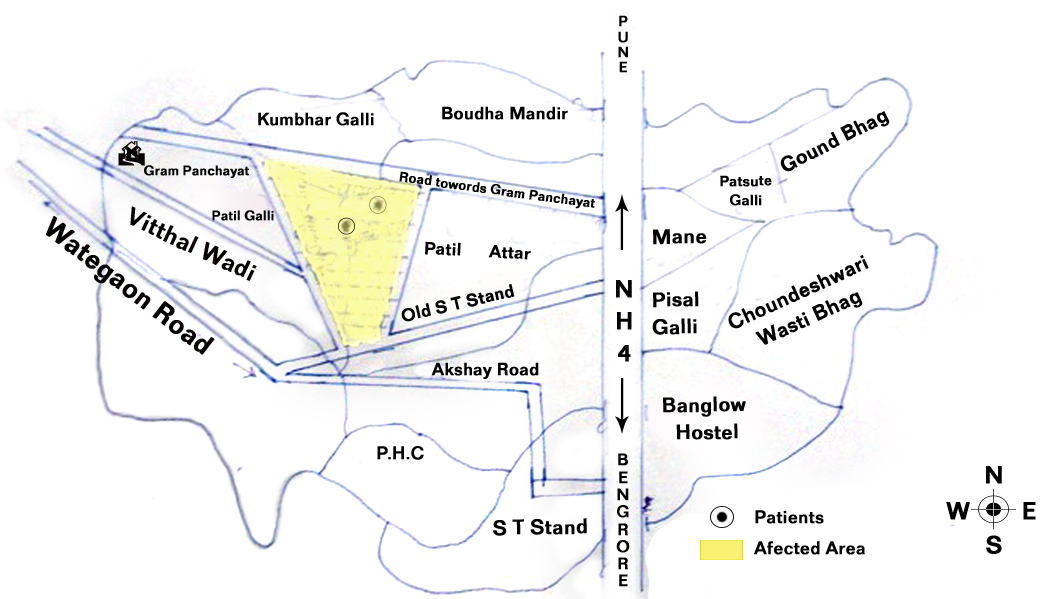
Around 20-25 cases of fever with joint pain were reported from the village Kasegaon, Maharashtra state, in the first week of January 2010. Following this, a team of medical doctors from the Krishna Institute of Medical Sciences, Karad, Maharashtra, in collaboration with the Primary Health Centre Kasegaon, District Sangli, carried out a house to house survey. The informed consents of the study subjects were obtained during the study. A spot map was prepared and the areas with the maximum number of cases were identified, namely, Muslim Samaj, Bhuyachi vagal and Chambhartek [Table/Fig-1].
Spot map showing area with maximum cases
A pretested proforma was prepared, which included the identification data, socioeconomic data, the information regarding the fever, its duration, the associated symptoms, the knowledge regarding the symptoms and the spread of Chikungunya, the health seeking behaviour, etc.
A population of 1599 from 388 households was covered. As per our clinical criterion, all the fever cases with joint pain or arthralgia were considered as cases of Chikungunya fever unless they were proved otherwise. A door to door survey was done to enlist the fever cases. A multipurpose worker from the Primary Health Centre accompanied us, who distributed paracetamol tablets to those who needed them, as per the doses which were prescribed. The people were advised to attend the Primary Health Centre if they wanted, where free treatment was available. We assessed a number of containers in each and every house and instructed the people to follow a "dry day" for vector control, particularly larval control. The concept of "dry day" meant, the weekly emptying of water containers, scrubbing and washing them, drying them, refilling them and covering the containers on the fixed day by all the community members. For the larval surveys, the basic sampling unit was a house or its premise, which were systematically searched for water- holding containers. The containers were examined for the presence of mosquito larvae and pupae by using a flash light. Paramethrin was sprayed in this area. Concurrently, by using pamphlets which were printed in the local Marathi language, we educated the local population regarding the personal, family and community protection against mosquito bites and the mosquito source reduction. Blood samples were taken from 8 out of 154 clinically suspected Chikungunya fever patients who were randomly selected and they were sent to the National Institute of Virology, Pune, India.
RESULTS
Among the total population of 1599 from 388 houses which were surveyed in the village, there were 154 clinically suspected Chikungunya fever cases. Hence, the prevalence was calculated to be 9.6%. Of these, 54.5% were males and 45.5% were females. About 72.7% of the cases were in the age range of 11-50 years, which was the active age group [Table/Fig-2].
Age and Sex wise distribution of the chikungunya fever cases
| Age groups | Sex |
|---|
| Male No. (%) | Female No. (%) | Total No. (%) |
| 0 -10 | 12(7.79) | 8(5.19) | 20(12.98) |
| 11 -20 | 16(10.39) | 10(6.49) | 26(16.88) |
| 21 -30 | 12(7.79) | 12(7.79) | 24(15.58) |
| 31 -40 | 14(9.09) | 22(14.29) | 36(23.38) |
| 41 -50 | 20(12.99) | 6(3.90) | 26(16.89) |
| 51 -60 | 6(3.90) | 4(2.60) | 10(6.49) |
| >60 | 4(2.60) | 8(5.19) | 12(7.79) |
| Total | 84(54.5) | 70(45.5) | 154(100) |
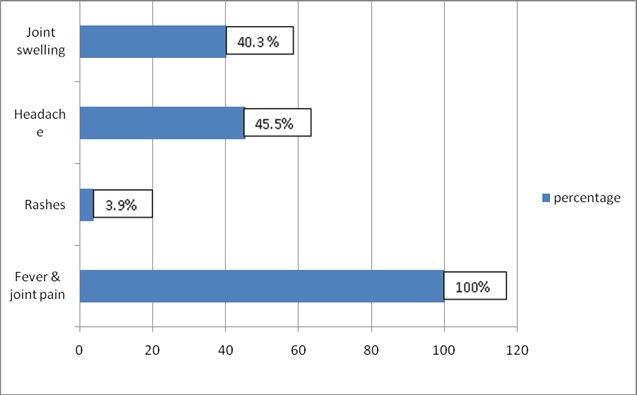
A majority of the cases (64.3%) belonged to the socioeconomic class III and 30.5% belonged to class V of the modified B.G. Prasad's classification [8]. Among the affected cases, 65.5% were educated up to the secondary level and 24.7% were illiterate. The main symptoms were an acute onset of fever with joint pain (100%).Multiple joints were involved in 89.6% cases; joint swelling was present in 40.3% of the cases. The other symptoms were headache (45.5% cases) and rash (3.9% cases). The mean duration of the fever was 3 days (range 1-10 days) [Table/Fig-3].
Symptoms of chikungunya fever percentages of cases
Out of the 8 blood samples which were taken from 154 clinically suspected Chikungunya fever cases, 5(62.5%) were reported as positive from the National Institute of Virology, Pune.
All the 154 patients visited the health care facility and consulted the physicians on the onset of the symptoms. About 40.3% people preferred to consult government health facilities, 30.5% consulted private doctors, 23.4% went to both government and private doctors, and 5.8 % people went to traditional healers to get relief [Table/Fig-4].
Treatment Seeking Behaviour of the chikungunya fever cases
| Health seeking behaviour | No (%) |
|---|
| Government health facility | 62(40.25) |
| Private doctors | 47(30.5) |
| Both government and private doctors | 37(24.02 %) |
| Traditional healers | 8(5.2) |
| Total | 154(100) |
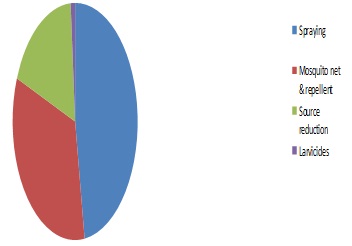
We also studied the knowledge regarding the Chikungunya fever, its prevention and its control in the affected region. In the affected area, 83.1% of the people were aware about Chikungunya fever. About 90.2% knew that Chikungunya fever was transmitted from mosquitoes to humans. Only 1.1% knew the vectors which were responsible for the transmission of Chikungunya. The knowledge regarding the modes of prevention of the Chikungunya infection among the respondents was as follows: [Table/Fig-5].
Knowledge of modes of prevention
Plastic drums, mud pots, flowerpots, cement tanks, overhead tanks, coconut shells and broken vessels were the common sources for the breeding of mosquitoes. Artificial collection of water was reported by 64.3% of the cases. We monitored the impact through various indices like the house index and the container index (House index-10%, Container index-7.5%). There was no case fatality in this outbreak.
DISCUSSION
This study was done in the affected village Kasegaon, District Sangli. In this study, more males were affected than females. Similar observations were reported by other studies [9, 10]. However, in a study which was conducted in an urban field practice area of a private medical college of Chennai and in an outbreak at Vellore, south India more females were affected than males [11, 12]. The maximum number of cases was in the age group of 11-50 years. This was similar to that in the outbreak in Shrirampur town [9]. In our study, 12.9% of the cases were below 10 years of age. In the study which was conducted by Sharma et al., during the outbreak in Madras city in 1964, it was found that the population which belonged to the age group of 5-9 years had the highest percentage of morbidity (23.2%) [10]. In our study, a majority of the cases (64.4%) belonged to the socioeconomic class III and a majority (65.3%) were educated upto the secondary level. In a study which was carried out at a village in the Villuppuram district of Tamil Nadu, 69.8% had secondary level education and 28.8% were graduates and above [13]. In a study which was carried out at Chennai, 44.9% of the persons who were affected, belonged to the socioeconomic class III [11] and another study reported that 30.2% patients were poor, who belonged to the social class IV. 26% patients were illiterate [9].
In the present study, the classical symptoms of fever with joint pain were observed. The disease had manifested after an incubation period of 2-4 days (range 3-12 days). The median duration of the fever was three days and for joint pain, it was four days in the acute phase [11]. The illness was self limiting. In a series of 876 patients who were admitted to a hospital in south India during January-September 2006, an abrupt onset of fever of short duration (100% cases) and severe and crippling arthritis which involved the knee, ankle, wrist and hands and feet (98% cases) were the most significant clinical manifestations. Bleeding (3% cases), fulminant hepatitis (2% cases) and meningoencephalitis (1% cases) were the rarer manifestations of the disease [14]. In most of the series, the fever and joint pain were almost universal at the onset. The fever was of sudden onset and of high grade (> 400C/1040F), which was accompanied by chills and rigors. The fever was biphasic or saddleback. The second phase of the fever was associated with relative bradycardia [15]. The fever tended to last for only 3-4 days. The ankles, knees and the wrist were the usual joints that were affected, but the involvement of the small joints of the hands and feet was also not uncommon [16]. Skin rashes have been reported in about 40-50% of the cases, which usually appear between the second and the fifth day of the onset of the fever. The rashes are mostly of the pruriginous maculopapular type. Maculopapular rashes can sometimes be accompanied by petechiae [1].
In our study, 40.3% of the cases preferred to consult government health facilities. In a Tamil Nadu study, 27% of the cases preferred treatment only from government health facilities. Private health facilities were utilized exclusively by 25% of the patients [13]. In another study, 77.7% of the affected persons sought treatment at private clinics and 18.4% took treatment at government health set ups [11].
Three main laboratory tests are used for diagnosing the Chikungunya fever: virus isolation, serological tests, and the molecular technique of the polymerase chain reaction (PCR). The disease is self limiting. There is no specific treatment for Chikungunya. A symptomatic treatment is recommended after excluding the more serious conditions. The symptomatic or supportive treatment basically comprises rest, the use of acetaminophen or paracetamol to relieve the fever and ibuprofen, naproxen or another non -steroidal anti -inflammatory agent (NSAID) to relieve the arthritic component. Using aspirin is not advised because of the risk of bleeding in a small number of patients and the risk of developing Reye's syndrome in children who are less than 12 years of age.
In our study, a majority of the patients (83%) were aware about the Chikungunya fever, but only 1% knew about the vectors which were responsible for the fever. Nagpal et al., reported that a majority of the respondents (63% in Latur, Maharashtra to 94% in Betul, Madhya Pradesh) were aware of Chikungunya fever, whereas in Delhi and Orissa, a majority (56% in Mahavir Enclave to 85% in Sundergarh, Orissa) were ignorant. A majority of the respondents ( 82% in Dwarka, Delhi to 92% in Kannur, Kerala) knew about the Chikungunya transmission. Only few respondents across the high incidence wards of all the states (3% in Sundergarh, Orissa to 43% in Alappuzha, Kerala) knew about the vectors which were responsible for the Chikungunya transmission. In Madhya Pradesh and Kerala, 48-69% of the patients respectively, preferred treatment with insecticides and source reduction. Among the low incidence wards of all the states, Maharashtra the highest number of respondents (72%) and had not known about it. In the high incidence and low incidence wards of Kerala, a majority (48 and 60% respectively) preferred to keep the surroundings mosquito free to prevent the disease [17].
A clinic-epidemiological study which was done on a Chikungunya outbreak in Maharashtra state, reported that only 8.9% patients knew correctly about the viral origin of the disease, that the transmitting vector species was least remembered (4.2%) and that about 38% people certainly knew as to how to carry out a source reduction which pertained to domestic water containers. The sources of the knowledge on Chikungunya, its transmission and the control measures for it were mainly paramedical workers and government doctors [18].
The preventive measures at the individual level included the use of mosquito repellents like coils, mats, body creams, mosquito nets, etc. At the community level, it is important to ensure that there are no collections of water in household vessels or around dwelling places. The usual recommendation is that on every fifth day, all the vessels which contain water should be emptied; this observance of a dry day breaks the life cycle of the mosquito. In the epidemic affected areas, there was an intermittent water supply; every 4th or 6th day, the water supply was there. So, there was a tendency among the people to store the water for longer periods of time. Hence, we have created awareness regarding the importance of the "dry day." Within six weeks of the implementation of the preventive measures, there was a drastic reduction in the incidence of the cases.
CONCLUSION
Chikungunya fever is self limiting; the morbidity can be very high in major outbreaks, resulting in a heavy social and economic tolls. The prevention of the disease requires a planned approach, besides knowledge and awareness on the early warning signs. An integrated vector management through the elimination of the breeding sites, the use of anti-adult and anti-larval measures and personal protection will contribute to the prevention of outbreaks. A community empowerment and mobilization is crucial for the prevention and control of Chikungunya.