A Huge Primary Ovarian Leiomyoma with Degenerative Changes-An Unusual
Ranjan Agrawal1, Mukta Kumar2, Lata Agrawal3, Keshav Kumar Agrawal4
1 Department of Pathology, Rohilkhand Medical College Hospital, Bareilly, UP, India.
2 Department of Pathology, Rohilkhand Medical College Hospital, Bareilly, UP, India.
3 Department of Obstetrics & Gynaecology, Rohilkhand Medical College Hospital, Bareilly, UP, India.
4 Department of Surgery, Rohilkhand Medical College Hospital, Bareilly, UP, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjan Agrawal, Professor, Department of Pathology, Rohilkhand Medical College Hospital Pilibhit, Byepass Road, Bareilly, UP, India.
Phone: 9412291009
E-mail: drranjan68@gmail.com
Primary ovarian leiomyoma is a rare benign tumour of the ovary, which is seen in women who are aged between 20 years to 65 years. Ovarian leiomyomas can be confused with other spindle cell tumours which display gross anatomical and histological similarities. A case of a primary leiomyoma of the ovary in a pre-menopausal female is being presented here, due to its huge size and unusual presentation.
Ovarian leiomyoma, Primary tumour, Benign, Huge, Secondary changes
INTRODUCTION
Leiomyoma is one of the rarest solid tumours of the ovary that accounts for 0.5-1% of all the benign ovarian tumours. Approximately 60 cases have been reported in the literature [1]. A majority of such tumours are small sized and they are discovered incidentally, with about 80% of the cases occurring in pre-menopausal women [1–5].
We are reporting a case of a huge primary ovarian leiomyoma in a 40 years old lady, which clinically and radiologically mimicked a broad ligament leiomyoma.
CASE REPORT
A 40 years old lady presented with pain in the abdomen and vomiting, of one month duration. On examination, a palpable mass was found in the right lower abdomen. Her blood pressure was 96/58 mmHg and her pulse was 108/min. On per-vaginal examination, it was suspected to be a right sided, broad ligament fibroid. Ultrasound of the abdomen revealed a huge pelvic mass. CT and MRI of the abdomen confirmed that the pelvic mass originated from the right ovary. The mass showed a heterogenous enhancement in a post-contrast study, with multiple necrotic and cystic components being present within, thus suggesting a diagnosis of a large ovarian teratoma.
Her pre-operative investigations revealed Hb of 7.53 g%, TLC of 8200 cells/mm3; differential counts of P-86 and L-14; random blood sugar of 160.2 mg%; blood urea of 23.9 mg%; serum creatinine of 1.0 mg% and serum amylase of 72 IU/dl. The total serum bilirubin was 1.28 mg% and the conjugated bilirubin was 0.97 mg%. The peripheral smear examination showed a microcytic hypochromic picture with no evidence of haemolysis. Her CA-125, CEA, CA 19-9 and AFP values were within normal limits. A laparotomy was performed under epidural anaesthesia. She was transfused with 2 units of a packed cell concentrate. Per-operatively, there was a huge right ovarian mass which measured 20 x 25 cm, with adherent bowel loops and parietal and visceral peritoneum. The uterus, both tubes and left ovary were unremarkable. Since the tumour was adherent to the surrounding adnexa, a debulking surgery was done.
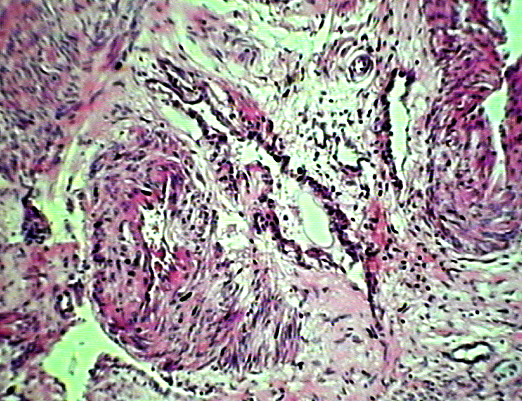
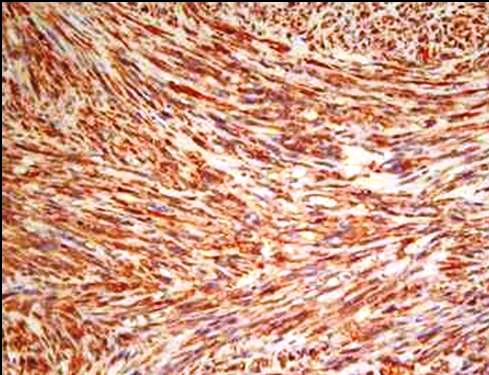
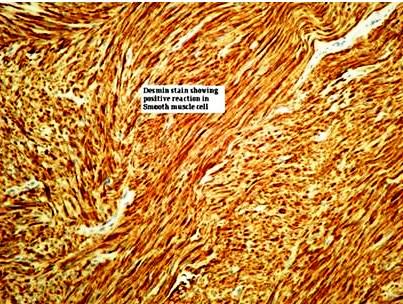
Grossly, the tumour was received in multiple pieces of varying dimensions [Table/Fig-1], with the largest measuring 6.5x3.8 cm. The cut-sections were homogenous, with few showing glistening white whorled areas. The microscopic examination showed irregular bundles and whorling of the spindle-shaped cells with elongated blunt nuclei. There was no atypia or pleomorphism and there were 2-3 mitotic figures per 10 high-power fields. Areas with varying degrees of hyaline degeneration and myxomatous changes were also present [Table/Fig-2]. Foci of haemorrhage and necrosis with no cellular reactions were observed, particularly next to the cystic spaces. There was no trace of normal ovarian tissue. The immunohistochemical staining revealed a diffuse positive staining for α-smooth muscle actin (SMA) [Table/Fig-3] and desmin [Table/Fig-4]. The post-operative period was uneventful.
Gross specimen with multiple irregular pieces obtained after debulking

Leiomyoma with areas of hyaline and myxomatous changes (H&E ×100).
Diffuse positivity of neoplastic cells on Immunohistochemical stain by SMA( smooth muscle actin) (IHC, SMA X100)
Desmin stain showing positive reaction in the neoplastic cells (IHC, Desmin X100)
DISCUSSION
Primary leiomyoma of the ovary is uncommon. It is likely that many cases are not reported, especially when the tumour is small or when it is discovered incidentally [1–3]. Most of the leiomyomas of the ovaries are small, measuring only a few millimetres or centimetres in diameter, which are usually less than 3cm. The tumour which was reported by Herbut had a maximum diameter of approximately 25 cm [2]. In the present case, the tumour was very large.
The incidence age of ovarian leiomyoma varies between 20 and 65 years. About 16% of the cases occur after menopause. They are usually unilateral, with no predilection for the left or the right side. Most of the bilateral cases have been reported in young females aged between 16 and 25 years [1, 4].
Clinically, many patients are asymptomatic, and the tumour is discovered incidentally. When symptoms are present, they are related to the presence of an adnexal mass, which are often accompanied by an abdominal swelling or pain. In pure ovarian leiomyomas, no menstrual irregularities are encountered. Weight loss, ascites and an increase in the abdominal girth may complicate the large and fairly rapidly growing tumours. Rarely, such tumours become twisted around their pedicle, with subsequent haemorrhage and necrosis. Most of the tumours which have been reported were freely mobile, but at times, they can adhere to the omentum, intestine or the uterus. The ovary proper may become almost completely absorbed by the tumour, as in our case, or portions of it may persist [5].
Macroscopically, the tumours are solid, firm, round or oval masses which have smooth surfaces. On cut-section, they have a white or grey-white solid surface. Frequently, a whorl formation can be recognized grossly. Secondary changes such as hyalinization, haemorrhage, calcification and cystic changes are present, especially in the larger tumours [4, 6, 7]. Microscopically, the smooth muscle cells are uniformly spindle shaped or elongated with blunt-ended or cigar shaped nuclei. Palisading of the nuclei may be present and it may be prominent. Mitotic activity is absent or very low, and cellular and nuclear pleomorphisms are not a feature. The correct diagnosis of a ovarian leiomyoma requires recognition of the smooth muscle nature of the tumour. In the present case, an immunohistochemical analysis confirmed our diagnosis.
Ovarian leiomyomas need to be distinguished from ovarian fibroma-thecomas, cellular fibromas, sclerosing stromal tumours, leiomyomas arising in the broad ligaments and uterine leiomyomas becoming parasites on the ovary (wandering leiomyomas). Ideally, a primary ovarian leiomyoma should be entirely within the ovary, with no similar lesions in the uterus or elsewhere. The co-existence of a ovarian leiomyoma with a uterine leiomyoma has been reported by several authors [3, 8].There was no associated uterine leiomyomatosis in our case. The tumour in the present case was of ovarian origin, because it replaced nearly the entire ovary and the normal ovarian tissue could not be discerned. The tube was stretched over the tumour. Primary ovarian leiomyoma must also be differentiated from a pedunculated subserosal (parasitic) uterine leiomyoma, which may have lost its original attachment and has instead become attached to the ovary, thus deriving its blood supply. In the development of ovarian and uterine leiomyomas, hormonal influences are known to play a vital role. A great majority of the leiomyomas of these two organs grow only between puberty and menopause. However, in a number of cases, this rule does not apply. To explain the histogenesis of this tumour, several theories have been proposed. According to the most accepted one, the tumour arises from the smooth muscle of the ovarian ligament, where they enter the ovary from the smooth muscle of the ovarian blood vessels. Endometriotic cysts have also been suggested to trigger metaplasia of the surrounding stroma into the smooth muscle cells.
These tumours are benign and radical surgeries are usually done for their complete removal. However, in the present case, since the tumour was very large and as it was also attached to the adjacent adnexa, a complete removal was not possible and a debulking surgery had to be carried out.
SUMMARY
A case of pure leiomyoma of the ovary has been described because of the features of the secondary changes, which, apart from being extremely rare due to its location, was one of the largest sized which has been reported so far.
[1]. Safaei A, Khanlari M, Azarpira N, Monabati A, Large ovarian leiomyoma in a postmenopausal womanIndian J Pathol Microbiol 2011 54:413-4.PMID: 21623113 [Google Scholar]
[2]. Herbut PA, Ovarian leiomyomaIn Gynaecological and obstetrical pathology 1953 1st editionPhiladelphiaLea and Febiger:501 [Google Scholar]
[3]. Lerwill MF, Sung R, Oliva E, Prat J, Young RH, Smooth muscle tumours of the ovary: A clinicopathologic study of 54 cases emphasizing prognostic criteria, histologic variants, and differential diagnosisAm J Surg Pathol.2 2004 8:1436-51.PMID: 15489647 [Google Scholar]
[4]. Murakami M, Uehara H, Nishimura M, Iwasa T, Ikawa H, A huge ovarian smooth muscle tumour: A case reportJ Med Invest 2010 57:158-62.PMID: 20299756 [Google Scholar]
[5]. Wellmann KF, Leiomyoma of the OvaryCan Med Assoc J.85(8):429-432.1961. PMCID: PMC1848262 [Google Scholar]
[6]. Wei C, Lilic N, Shorter N, Garrow E, Primary ovarian leiomyoma: A rare cause of ovarian tumour in adolescenceJ Pediatr Adolesc Gynecol 2008 21:33-6.PMID: 18312799 [Google Scholar]
[7]. Ramalakshmi Pullela VB, Das S, Chunduru B, Dua S, A case of ovarian leiomyoma with cystic degenerationIndian J Pathol Microbiol 2009 52:592-4.PMID: 19805992 [Google Scholar]
[8]. Matamala MF, Nogales FF, Aneiros J, Herraiz MA, Caracuel MD, Leiomyomas of the ovaryInt J Gynaecol Pathol. 1988 7:190-6.PMID:3397211 [Google Scholar]