A twenty six years old woman presented with visual disturbance, headache and gait disturbance ten weeks postpartum. Imaging studies identified an acute infarction in the left thalamus. This case report discusses her presentation, investigations and management and the aetiology of stroke in pregnancy and the postpartum period.
Stroke, Postpartum, Pregnancy, Neurology
INTRODUCTION
There is an increased risk of stroke during pregnancy and the postpartum period with the risk greatest deemed to be in the immediate post-partum period. Stroke is an important contributor to maternal morbidity and mortality with four women dying of cerebral thrombosis during the period of 2006 to 2008, a rate of 0.17 per 100,000 maternities [1]. The rate of stroke during the postpartum period has increased by 83% from 0.12 in 1994 to 0.22 per 1,000 deliveries in 2006 according to a recent study by Kuklina et al., [2]. During the study period the total number of pregnancy related hospitalisations that involved a stroke also increased by a relative 54% [2] so this may be an increasing presentation in pregnant and recently pregnant women. We are presenting a rare case of stroke in the late postpartum period. The case report discusses her presentation, investigations and management and the aetiology of stroke in pregnancy and the postpartum period.
CASE REPORT
A twenty six years old woman with a past medical history of bilateral congenital blue dot cataracts was seen by her General Practitioner on a home visit with a one day history of nausea and vomiting three times, left-sided headache, dizziness, blurred vision and gait disturbance. She was found to be confused talking about a ‘flying giraffe– and drowsy. She was ten weeks postpartum after delivering a normal baby girl at term plus nine days. The placenta was retained and was manually removed by an obstetric registrar one hour and twenty minutes after delivery. The placenta was examined and deemed complete. She had no further vaginal bleeding. She is not taking any medications. She is an ex-smoker with an eight pack year history. Her Body Mass Index (BMI) is 33kg/m2. She lives with her husband and two children who are three and a half years old and ten weeks old. She was sent to Accident and Emergency (A&E) and discharged with a diagnosis of flu.
The patient returned to A&E two days later with continuing flu-like symptoms, headache and blurred vision and was admitted to the Clinical Decisions Unit (CDU). She was seen by the on-call medical team on her admission and was found to have sinus tachycardia, failure of upwards gaze, internuclear ophthalmoplegia, blurred vision, ataxia and incoherent speech. Some vertical nystagmus was noted. Power, tone, sensation and reflexes were all normal. Plantars were down-going bilaterally. There was no fine tremor. Her blood pressure was 120/75 mmHg. A differential diagnosis of postpartum thyrotoxicosis, multiple sclerosis, cerebral infarction or venous thrombosis was made and investigations were requested.
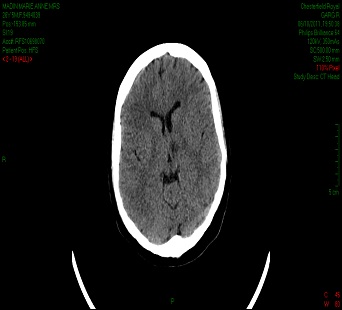
Laboratory tests revealed the following: haemoglobin 11.7 g/dL, white cell count 9.3 x 109/L, platelets 288 x 109/L, erythrocyte sedimentation rate of 47 mm/hr, C-reactive protein level of 20 mg/L, thyroid stimulating hormone 2.0 mIU/L and normal clotting, urea and electrolytes and liver function tests. Her chest X-ray showed clear lung fields. An X-ray Computed Tomography (CT) scan of the head performed on admission revealed an area of low attenuation within the left thalamus extending towards the mid line and close to the third ventricle, representing an acute infarct [Table/Fig-1].
An X-ray computed tomography (CT) scan of the head showing an area of low attenuation within the left thalamus extending towards the mid line and close to the third ventricle, representing an acute infarct
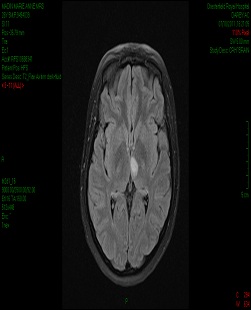
A magnetic resonance image (MRI) of the brain performed on day two of admission showed high signal changes in the left thalamus on T2 weighted and Fluid Attenuated Inversion Recovery (FLAIR) axial images. The region demonstrated restricted diffusion on Diffusion Weighted Imaging (DWI) and low calculated Apparent Diffusion Co-efficients (ADC). The cerebral venous sinuses were patent [Table/Fig-2].
A magnetic resonance image (MRI) of the brain showing high signal changes in the left thalamus on T2-weighted and fluid attenuated inversion recovery (FLAIR) axial images. The region demonstrated restricted diffusion on diffusion-weighted imaging (DWI) and low calculated apparent diffusion coefficients (ADC). The cerebral venous sinuses were patent
The patients– symptoms resolved with only some minor visual disturbance remaining. She went home over the weekend to be with her newborn baby and family and returned for further investigations on Monday morning.
Transthoracic echocardiography was unremarkable with good systolic function, thin and mobile valves and no evidence of patent foramen ovale or an atrial septal defect. Doppler ultrasound of the lower limbs showed no evidence of a deep vein thrombosis bilaterally. No visual field defects were detected on Goldmann perimetry. Ultrasound doppler of the extra-cranial carotid arteries found normal vessels with good flow bilaterally.
Further screening tests for anti-nuclear antibody, rheumatoid arthritis, hepatitis B, Treponemal IgG and IgM, perinuclear and cytoplasmic anti-neutrophil cytoplasmic antibody, double-stranded DNA IgG, glomerular basement membrane antibody, extractable nuclear antigens and complement levels were all negative. A thrombophilia screen was not indicated as per the consultant haematologist as her clotting was normal.
The patient was commenced on and discharged with aspirin 300mg once daily for two weeks with clopidogrel 75mg once daily thereafter, lansoprazole 30mg once daily and simvastatin 40mg nocte. She was advised to stop breast feeding by the obstetrics and gynaecology team. Upon discharge her neurology had resolved and she was followed up in clinic in two weeks, where she was found to have to further problems.
DISCUSSION
This case concerns a rare presentation of late postpartum cerebral infarction involving the left thalamus. The reported incidence of pregnancy-related stroke varies widely but has been reported to lie between eleven and twenty-six deliveries per 100,000 maternities [3] with the highest risk in the postpartum period.
The pathophysiology of cerebral infarction in pregnancy and the postpartum period is thought to be related to significant haemodynamic changes during pregnancy and after delivery. Blood volume increases up until thirty-four weeks gestation predominantly due to the increased capacity of the uterine, breast, renal, striated muscle and cutaneous vascular systems. There is a greater increase of plasma volume relative to that of the red cell mass leading to a state of haemodilution and a decrease in haemoglobin concentration. This serves to facilitate maternal and fetal exchanges and provide adequate blood supplies to manage blood loss at delivery. In addition to increases in red call mass and plasma volume, fibrinogen, factors VII, X and XII as well as the number of platelets rise to the upper limits of normal resulting in a relatively hypercoagulable state. There is a rise in cardiac output during pregnancy and following delivery to compensate for these changes, primarily due to an increase in stroke volume and heart rate and a steady reduction in systemic vascular resistance.
A study by Skidmore et al., [4] evaluated the presentation, timing, aetiology and outcome of women with ischaemic stroke, haemorrhagic stroke and cerebral venous thrombosis during pregnancy and postpartum at three hospitals in Indianapolis. They included events up until 12 weeks postpartum. The majority of events occurred in the third trimester and postpartum period with a cluster of 44% of events occurring in postpartum week one.
In a further single-centre 20 years study by Witlin et al., [5] auditing women diagnosed with postpartum stroke, of the twenty women included, six were diagnosed with arterial cerebral infarction with a mean time of occurrence at eight days post-partum (range: 3-35 days). They, along with a study by Lanska and Kryscio [6], found an association between post partum stroke and caesarean section and hypertensive disorders of pregnancy, neither of which our patient experienced. Other risk factors identified include pre-existing or pregnancy-related hypertension and eclampsia, diabetes, sickle cell disease, thrombophilia, smoking and heart disease [3].
A study conducted by Ducrocq et al., [7] looking at young patients admitted to a French university hospital with cerebral infarction between 1990 and 1997 found a history of pregnancy or postpartum period in 13 cases (9.3%). They also found that patients whose stroke remained unexplained were often younger 33.7 years versus 37.7 years (P=0.002), had less risk factors (P<0.00001) but had a better prognosis (P=0.01).
In terms of secondary prevention, despite limited research and data, some studies have recommended the use of low dose aspirin (75mg once daily) in breast feeding mothers [8]. Our patient was advised not to breast feed.
CONCLUSION
This patient has no other major risk factors for stroke so the aetiology is likely to be related to her recent pregnancy. Although this risk has previously been reported as highest in the immediate post-partum period, this patient case shows us this risk may extend further than previously thought in some individuals. Fortunately in this patient–s case her prognosis is excellent.
[1]. Saving Mothers– Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008.. BJOGAn International Journal of Obstetrics and Gynaecology March 2011 118:1-203. [Google Scholar]
[2]. Kuklina EV, Tong X, Bansil P, George MG, Collaghan WM, Trends in Pregnancy Hospitalizations That Included a Stroke in the United States From 1994 to 2007: Reasons for Concern?Stroke 2011 DOI: 10.1161/STROKEAHA.110.610592 [Google Scholar]
[3]. Davie CA, O–Brien P, Stroke and pregnancyJournal of Neurology, Neurosurgery and Psychiatry November 2008 79:240-45. [Google Scholar]
[4]. Skidmore FM, Williams LS, Fradkin KD, Alonso RJ, Biller J, Etiology, and outcome of stroke in pregnancy and puerperiumJournal of Stroke and Cerebrovascular Diseases January 2001 10(1):1-10. [Google Scholar]
[5]. Witlin AG, Fand Sibai Matter, BM, Postpartum stroke: A twenty years experienceAmerican Journal of Obstetrics & Gynecology July 2000 183(1):83-8. [Google Scholar]
[6]. Lanska DJ, Kryscio RJ, Risk Factors for Peripartum and Postpartum Stroke and Intracranial Venous ThrombosisStroke 2000 31:1274-82. [Google Scholar]
[7]. Ducrocq X, Lacour JC, Debouverie M, Bracard S, Girard F, Weber M, Cerebral ischemic accidents in young subjects. A prospective study of 296 patients aged 16 to 45 yearsRevue Neurologique September 1999 155(8):575-82. [Google Scholar]
[8]. Helms AK, Kittner SJ, Pregnancy and StrokeCNS Spectrums July 2005 10(7):580-87. [Google Scholar]