A Case of Ankylosing Spondylitis and Discussion of the Literature
M.P. Ranjith1, R. Divya2
1 Consultant Physician, Department of General Medicine, Melepurakkal Hospital, Malappuram, Kerala, India.
2 Consultant Physician, Department of General Medicine, Melepurakkal HospitalMalappuram, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjith M.P, Bhavatharini, Pantheerankave P.O. Kozhikode-673019, Kerala, India.
Phone: 9846382001
E-mail: drranjithmp@gmail.com
Ankylosing spondylitis (AS) is a systemic inflammatory disease. Its pathogenesis has not been completely understood, but the HLA-B 27 positive immune cells are thought to be involved. Nonsteroidal anti-inflammatory agents are the first line drugs and they effectively relieve the symptoms. Biological agents such as Infliximab may help in targeting the underlying inflammatory process and have been used recently. Here, we are reporting a case of AS with established classical skeletal deformities.
Ankylosing spondylitis, Sacroilitis, Bamboo spine, Romanus lesion, Enthesitis
INTRODUCTION
The term, ‘ankylosing’ has been derived from the Greek word, ‘ankylos’, which means stiffening of a joint, while ‘spondylos’ means vertebra. The aetiology of ankylosing spondylitis is unknown, and it primarily affects the axial skeleton. Familial incidence is common. Approximately 90-95% of the patients with ankylosing spondylitis are positive for the human leukocyte antigen B27 (HLA-B27) assay, as compared to 7% positivity in the general population [1–4]. The age of onset is second or third decade of life [5] and males are affected two to three times more than females [6].
CASE REPORT
A 42 years old man presented with the complaint of gradually progressive low back pain, which was associated with stiffening and deformity of the spine and hip. He had episodes of back pain which woke him at night and associated with spinal stiffness in the morning. He had no history of fall, diabetes or hypertension. Examination revealed kyphosis, stooping forward position of the neck and flexion deformity of both hip joints [Table/Fig-1]. There was loss of lateral and anterior flexions of lumbar spine, and tenderness over the sacroiliac joint. His chest expansion was 2.4cm and Schober’s test was positive.
Ankylosing spondylitis patient showing kyphosis, stooping forward position of neck and flexion deformity of both hip joints

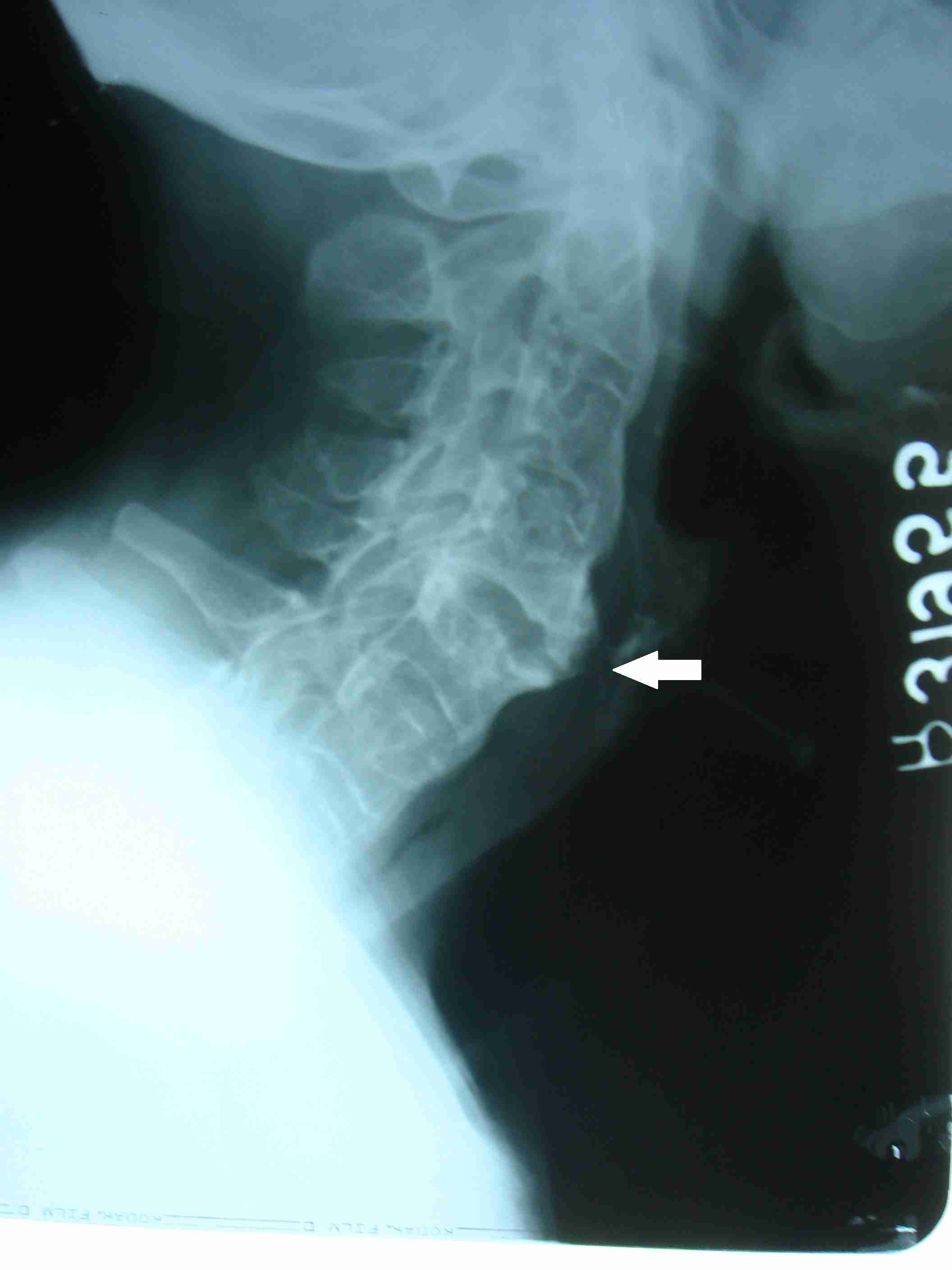
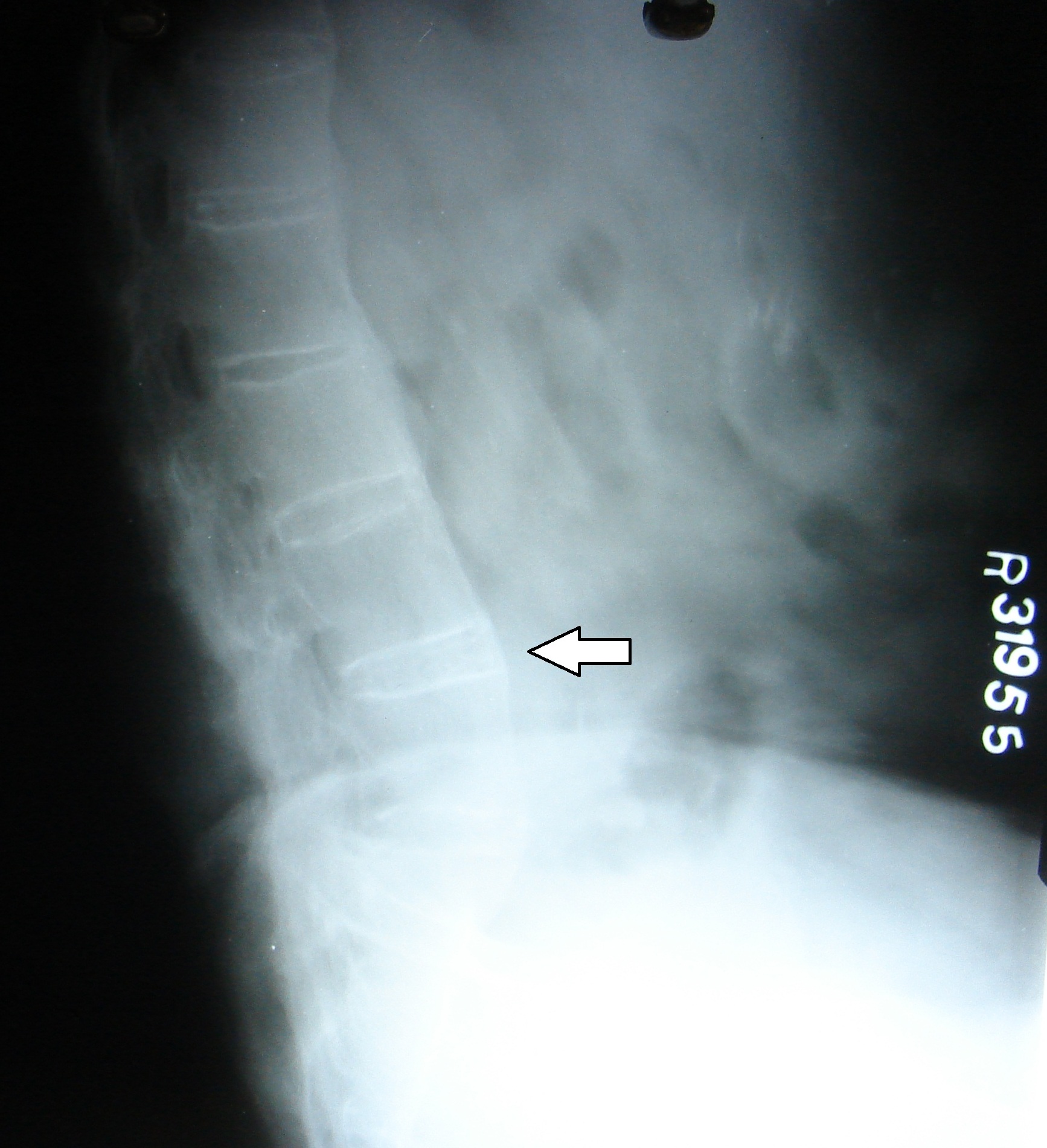
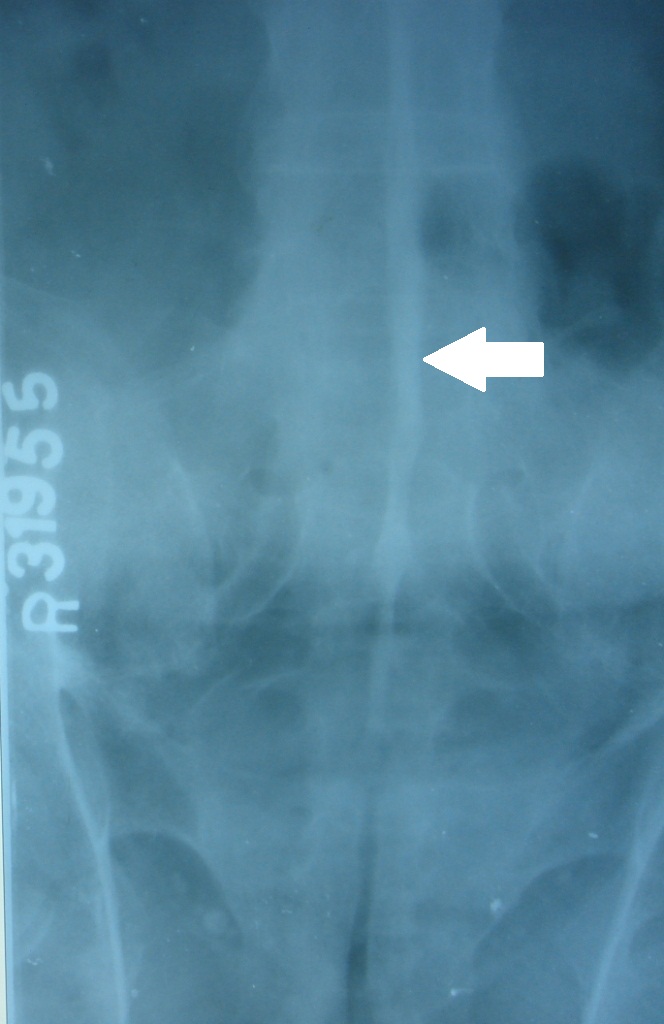
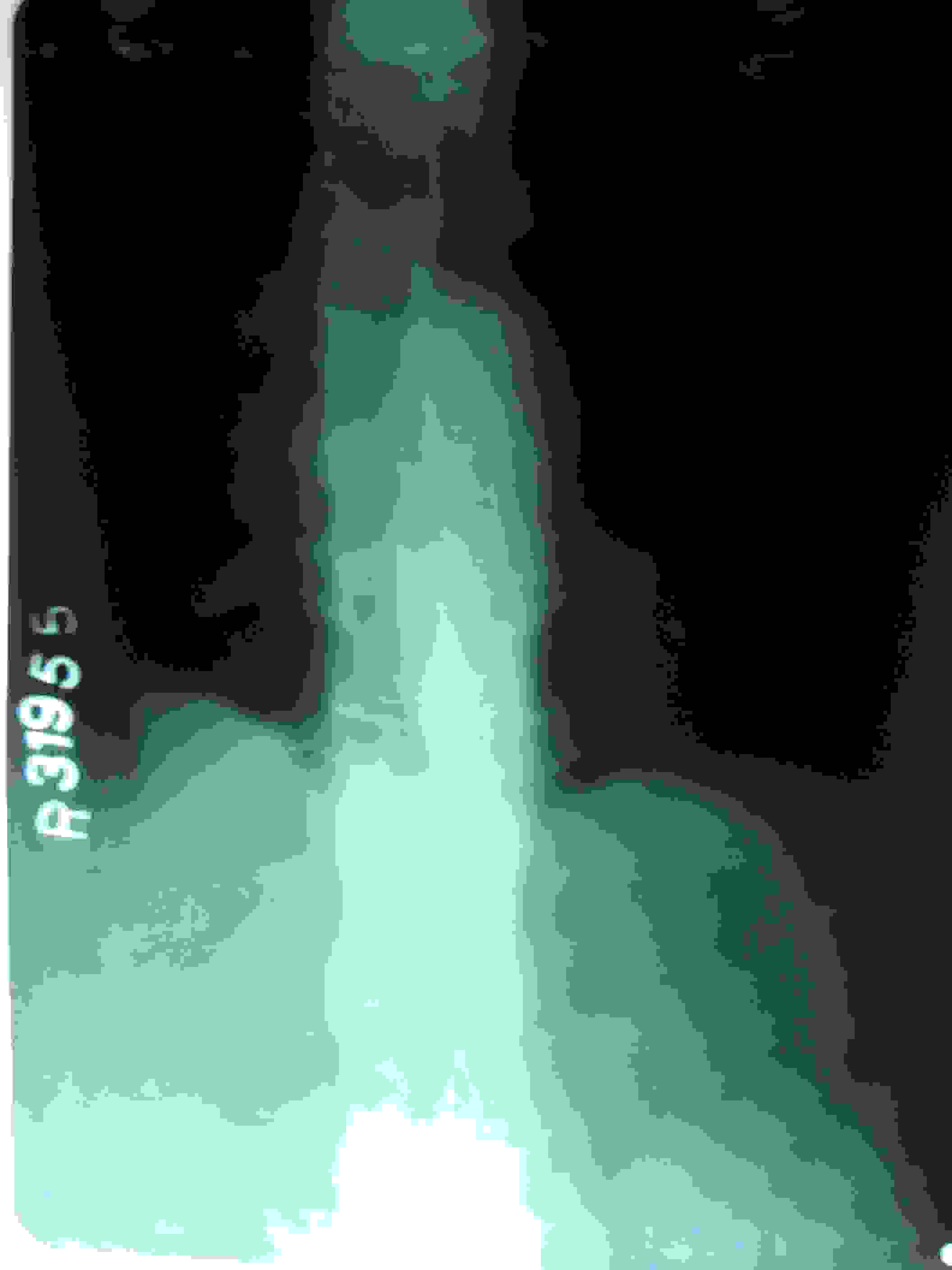
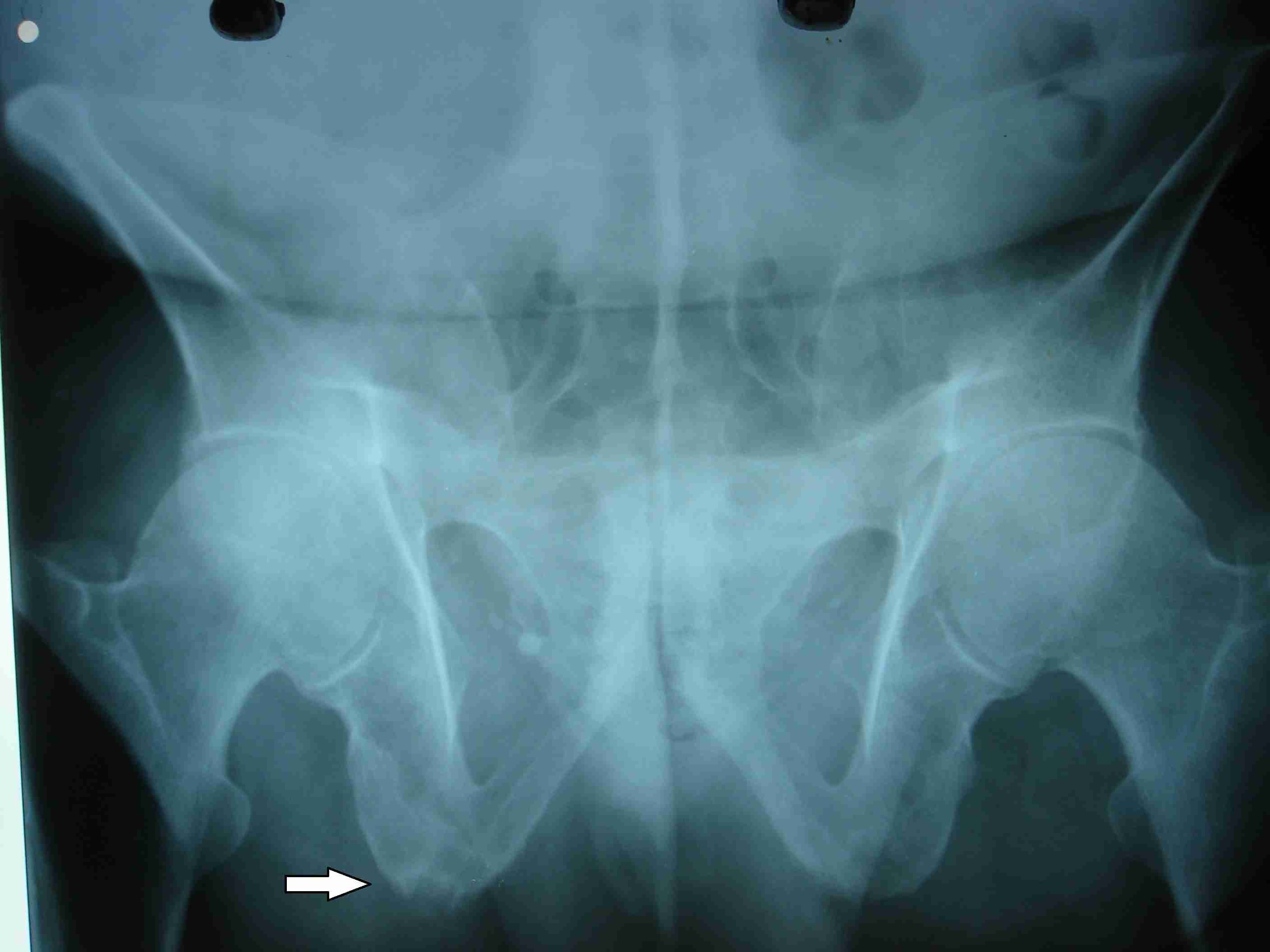
A skiagram of spine showed small erosions at the vertebral body corners, which were surrounded by reactive sclerosis (a shiny corner sign or a Romanus lesion) [Table/Fig-2], squaring of the vertebral body in the lumbar spine, calcification of the discs at multiple levels [Table/Fig-3] and posterior interspinous ligament ossification, which produced an appearance of a solid midline vertical dense line [Table/Fig-4]. Complete fusion of the vertebral bodies by syndesmophytes and other related ossified areas produced the characteristic bamboo spine appearance [Table/Fig-5] [7]. A pelvic radiograph showed ill-defined erosions with adjacent sclerosis at the right ischial tuberosity [Table/Fig-6].
Lateral radiograph showing erosions at the T12 and L1 vertebral bodies anterior corner, shiny corner sign or Romanus lesion (arrows)
Lateral radiograph showing L2-L3, L3-L4 and L4-L5 disk calcifications and L2-L3 anterior syndesmophytes
Skiagram lumbar spine frontal view showing posterior interspinous ligament ossification with linking of the spinous process, producing an appearance of a solid midline vertical dense line
Skiagram lumbar spine frontal view showing complete fusion of the vertebral bodies by syndesmophytes and other related ossified areas (Bamboo spine appearance)
Skiagram pelvis frontal view showing ankylosis of sacro iliac joint and illdefined erosions with adjacent sclerosis at the right ischial tuberosity (arrow)
Lab tests showed normochromic normocytic anaemia (Hb 8.9gm %), ESR -46mm/1st hour and a WBC count of 8700/mm3. The human leukocyte antigen (HLA) typing was positive for HLA B27. A diagnosis of AS was made according to the modified New York criteria [8]. Since the patient already had established deformities, he was managed symptomatically with analgesics and exercises.
DISCUSSION
Ankylosing Spondylitis (AS) is a chronic inflammatory disease of insidious onset. The primary pathologic site is the enthesis, or site of insertion of tendons or ligament capsules into the bone [9]. The typical findings like syndesmophyte formation, squaring of the vertebral bodies, vertebral end plate destruction and achilles tendinitis can be explained by the enthesitis [10]. The process usually starts at the sacroiliac joint. Other sites involved are iliac crest, ischial tuberosity, greater trochanter, patella and calcaneum [11]. Ankylosing Spondylitis shows a familial aggregation and may associate with diseases such as Reiter’s syndrome, ulcerative colitis and other bowel conditions. It also occurs more frequently in patients with psoriatic arthritis.
The most common presenting symptom is low back pain [5]. The inflammation progresses up the spine and affects the rib cage. Involvement of the costovertebral joints produces reduced chest expansion [1]. The differential diagnosis in the early stage is mainly other lumbar disc lesions. However, the main feature which helps in distinguishing the disc lesions from AS is that in young people, a disc lesion is usually related to a traumatic incident. The physical findings include loss of spinal flexion, extension, lumbar lordosis, diminished chest expansion and exaggerated thoracic kyphosis. The laboratory investigations show elevated levels of markers of inflammation like erythrocyte sedimentation rate and C-reactive protein. Few studies have shown lower levels of Vitamin A, C, E and β-carotene in plasma. Reduced glutathione and glutathione peroxidase values in the erythrocytes is seen in patients with AS than in controls [12]. Once the diagnosis is confirmed, the patient should be educated about the progress and complications of the disease. A regular lifelong exercise is the mainstay of treatment and the other treatment modalities include disease modifying drugs, biologicals and surgical corrections of the deformities and complications.
Our patient had chronic back pain, stiffness and the characteristic skeletal deformities. The Schober’s test was positive. A skiagram of the spine and pelvis showed the typical findings of established ankylosis. The human leukocyte antigen B27 typing was positive. He already had established deformities and so he was managed with analgesics and exercise therapy. Usually the disease will not affect the life expectancy, except in patients with severe deformities [13]. This report will give an idea about the presentation and the characteristic imaging findings of ankylosing spondylitis to the readers.
[1]. Khan MA, Ankylosing Spondylitis: Clinical features Rheumatology3rd edLondon:1423-27. [Google Scholar]
[2]. Ckou CT, Factors effecting pathogenesis of ASChin Med J. (Engl) 2001 114:212-13. [Google Scholar]
[3]. Braun J, Brandt J, Listing J, Zink A, Alten R, Golder W, Gromnica-lhle E, Kellner H, Krause A, Schneider M, Sorensen H, Zeidler H, Thriene W, Sieper J, Treatment of active AS with Infliximab-a double blind, placebo controlled multicentric trialLancet 2002 359:1187-93. [Google Scholar]
[4]. Braun J, Bollow M, Remlinger G, Eggens U, Rudwaleit M, Distler A, Prevalance of spondylopathies in HLA-B27 +ve and –ve blood donorsArthritis Rheum 1998 41:58-67. [Google Scholar]
[5]. Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A, Ankylosing Spondylitis, an overviewAnn Rheum Dis 2002 61(suppl 3 iii):8-18. [Google Scholar]
[6]. Zink A, Braun J, Listing J, Wollenhaupt J, Disability and handicap in rheumatoid arthritis and ankylosing spondylitis--results from the German rheumatological database. German Collaborative Arthritis CentersJ Rheumatol 2000 27:613-22. [Google Scholar]
[7]. Brent Lawrence H, Ankylosing Spondylitis and Undifferentiated Spondyloarthropathy. Emedicine medscape.com/article/332945-overview (Online). Updated: Nov 3, 2009. Available at: emedicine.medscape.com. Accessed April 18 ,2010 [Google Scholar]
[8]. Van der Linden S, Valkenburg HA, Cats A, Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteriaArthritis Rheum 1984 27:361 [Google Scholar]
[9]. Kelley WN, Harris ED, Ruddy S, Sledge CB, Textbook of Rheumatology 1997Spondyloarthropathies – Sjef van der LindenCh 59ed. 5:969-1014. [Google Scholar]
[10]. Kaya Taciser, Bal Serpil, Gunaydin Rezzan, Relationship between the severity of enthesitis and clinical and laboratory parameters in patients with ankylosing spondylitisRheumatol Int 2007 27:323-27. [Google Scholar]
[11]. Peh Wilfred CG, Ankylosing Spondylitis. Emedicine. Medscape. com/ article/386639 (online). Mar 25, 2009. Available at: emedicine. medscape.com. Accessed April 18 ,2010 [Google Scholar]
[12]. Nazıroglu M, Akkus S, Celik H, Levels of lipid peroxidation and antioxidant vitamins in plasma and erythrocytes of patients with ankylosing spondylitisClin Biochem 2011 Dec 44(17-18):1412-15. [Google Scholar]
[13]. Belachew D A, Sandu N, Schaller B, Guta Z, Ankylosing spondylitis in sub-Saharan AfricaPostgrad Med J 2009 85:353-57.doi:10.1136/ pgmj.2007.064717 [Google Scholar]