Ovaries are paired, pelvic, female reproductive organs. The diagnoses of ovarian neoplasms depend mainly on histopathological examinations, as they are inaccessible for cytological techniques, except when they are approached through imaging techniques. Even though ovarian masses can be approached by laproscopy and ultrasound guided aspiration, there are controversial views regarding their safety [1, 2]. The present study was done to evaluate the status of intraoperative cytology as a diagnostic and a supportive investigation for ovarian tumours.
MATERIAL AND METHODS
The present study was conducted in the Department of Pathology, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India during a time span of 13 months (June 2011 to June 2012).
This was a prospective study which was done on 50 suspected ovarian neoplasms. Imprint smears were made peroperatively from the fresh samples from various representative areas, immediately fixed in 95% ethyl alcohol and stained with the haematoxylin and eosin stain. The cytodiagnoses on smears were made, based on the cellularity, the pattern and the cell morphology. The interpretations of the cytology slides were assisted by the available clinical data and the gross findings. Rapid opinions regarding the benign or malignant nature of the lesion and the type of the tumour were given. For all the malignant lesions, the adequacy of the surgical margins was ensured. Peritoneal washings were done for the staging of malignant tumours. Since the imprint smears were not made from the peritoneum, these were not considered for the study. Later, the cytological diagnosis was compared with the histopathological diagnosis, taking it to be the gold standard.
RESULTS
The present study consisted of 50 cases. The age range varied from 2 to 65 years, the mean age being 42 years. Among the 50 cases, the final histopathological diagnosis showed that 20 were benign lesions, 4 were borderline epithelial neoplasms and that 26 were malignant tumours. The correlation between the intraoperative diagnosis and the final histopathological diagnosis is shown in [Table/Fig-1,2,3,4,5,6,7,8,9,10&11]. A diagnostic concordance was observed in 45 of the 50 cases. The overall diagnostic accuracy of the intra operative imprint cytology has been satisfactory, with those of 90% of the cases correlating with the final diagnoses. The characteristic cytological pattern was noted in various types of surface epithelial, sex cord stromal and germ cell tumours. Five of the study cases in which the intra operative imprint cytologies did not correlate with the final diagnoses included 2 endometrioid carcinomas which were misdiagnosed as cystadenocarcinomas, 2 mucinous carcinomas which were misdiagnosed as borderline mucinous tumours and 1 borderline mucinous tumour which was misdiagnosed as a mucinous cystadenoma.
Final histopathological diagnosis with cytological correlation by imprint cytology
| Number of cases | Histopathological diagnosis | Cytological diagnosis | Correlation |
|---|
| 3 | Papillary cystadenoma | Papillary cystadenoma | 3/3 |
| 4 | Papillary serous carcinoma | Papillary serous carcinoma | 4/4 |
| 2 | Endometrioid carcinoma | Cystadenocarcinoma (2) | 0/2 |
| 9 | Cystadenocarcinoma | Cystadenocarcinoma | 9/9 |
| 5 | Mucinous carcinoma | Mucinous carcinoma (3) Borderline mucinous tumor (2) | 3/5 |
| 4 | Borderline mucinous tumor | Borderline mucinous tumor (3) Mucinous cystadenoma (1) | 3/4 |
| 5 | Granulosa cell tumor | Granulosa cell tumor | 5/5 |
| 4 | Fibrothecoma | Fibrothecoma | 4/4 |
| 3 | Dysgerminoma | Dysgerminoma | 3/3 |
| 1 | Mixed germ cell tumor (dysgerminoma +yolk sac tumor) | Dysgerminoma | 1/1 |
| 8 | Mature teratoma | Mature teratoma | 8/8 |
| 2 | Metastatic adenocarcinoma | Metastatic adenocarcinoma | 2/2 |
| Total = 50 | | | 45/50 |
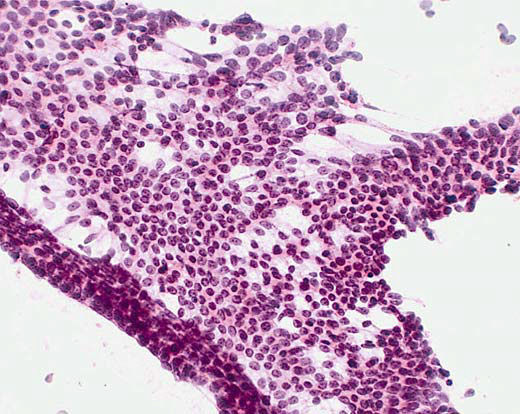
Serous benign cystadenoma. Monolayer and 2D cellular aggregate. Cells with uniform size and shape. Oval bland nuclei with regular chromatin and small, fine nucleoli, scant cytoplasm. Preservation of polarity and cohesiveness. Clean background. HE, x 200
(Image courtesy:Dr. Alvarez Santin C. et al.)
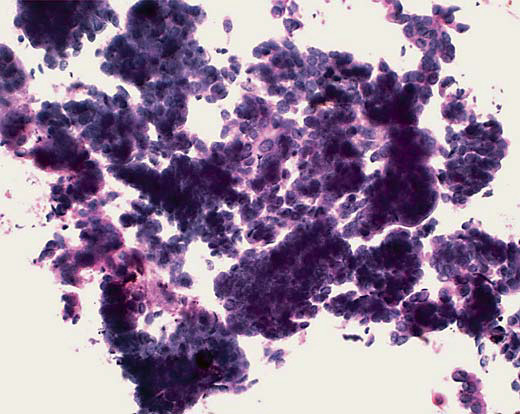
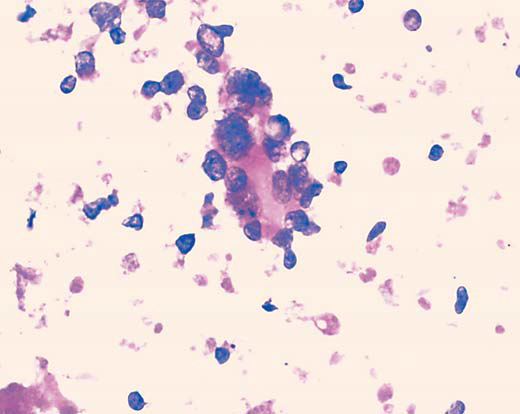
Serous borderline tumor. High cellularity. 2D and 3D dense cell groups. Scarce single cells. Low to moderate nuclear atypia. Oval and round nuclei, small, fine nucleoli, scant cytoplasm. HE, x200
(Image courtesy:Dr. Alvarez Santin C. et al.)
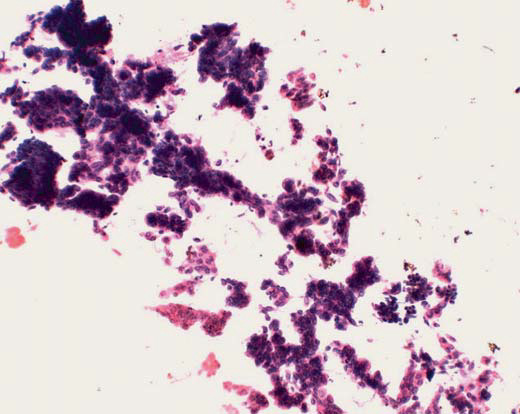
Serous borderline tumor. Branching papillary pattern with peripheral detachment of small epithelial nests. Low nuclear atypia. Clean background. HE, x100
(Image courtesy:Dr. Alvarez Santin C. et al.)
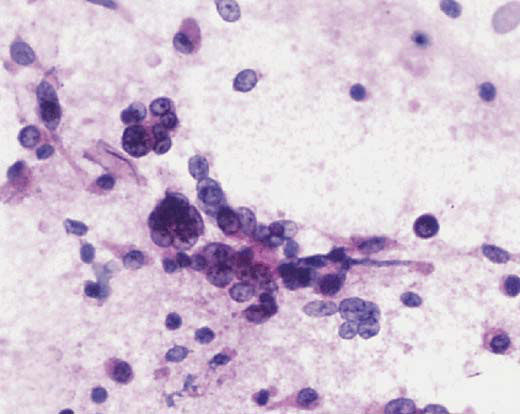
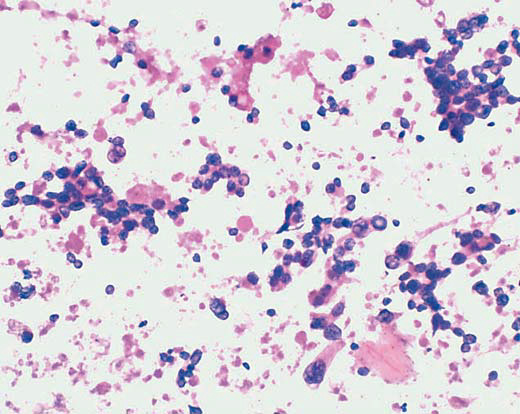
Serous carcinoma. Numerous single cells and small 3D groups. Loss of polarity and cohesiveness. High nuclear atypia. Irregular chromatin and prominent or macro nuclei. HE x200
(Image courtesy:Dr. Alvarez Santin C. et al.)
Clear cell carcinoma. High cellularity. Loosely cohesive cell clusters. Small, round papillary groups. Single cells. Eosinophilic secretion. HE, x 200
(Image courtesy:Dr. Alvarez Santin C. et al.)
Clear cell carcinoma. Three dimensional papillary groups with hyalinized cores. Hobnail cells with peripheral nuclear protrusion. High nuclear atypia, hyperchromasia. Vacuolated cytoplasm. HE, x 400
(Image courtesy:Dr. Alvarez Santin C. et al.)
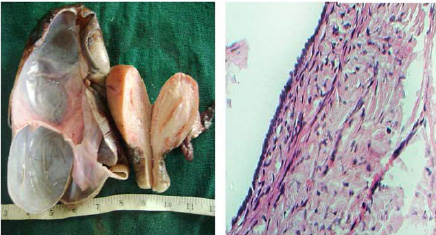
Serous cystadenoma. Gross picture showing the smooth inner wall. Photomicrograph showing cuboidal non ciliated epithelium. HE, x400
(Image courtesy:Dr. Alvarez Santin C. et al.)
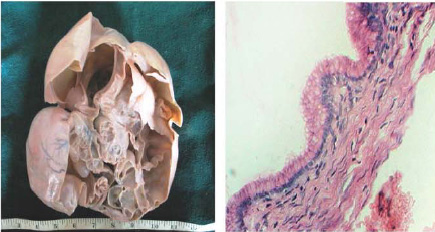
Mucinous cystadenoma. Gross picture showing multiloculated cysts filled with mucinous material. Photomicrograph shows columnar cells with intracytoplasmic mucin, HE 400x
(Image courtesy:Dr. Alvarez Santin C. et al.)
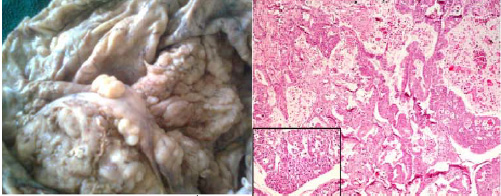
Serous cystadenocarcinoma, Gross picture shows inner cyst wall showing multiple papillary structures. Photomicrograph shows papillary arrangement of malignant cells, HE, 100x.Inset: pleomorphic cells with occasional mitosis HE, 400x
(Image courtesy:Dr. Alvarez Santin C. et al.)
Teratoma.Gross picture showing cystic areas filled with hair, sebum and fat
(Image courtesy:Dr. Alvarez Santin C. et al.)

DISCUSSION
Dudgeon and Patrick were the first to describe the imprint smears of fresh tissues in the rapid microscopic diagnoses of tumours [3]. Following this, several studies which were done in the past have discussed the use of imprint and touch preparations, especially as a tool for making the intraoperative diagnoses [4–6].
Few studies have documented ovarian cytological features in the imprint smears which were obtained during intraoperative procedures [7–13]. In this study, the routine use of cytological imprint smears allowed us to document these features and to underscore the advantages and the limitations of the technique.
Although the purpose of this study was not to give a precise measurement of the diagnostic performance of cytology in an intraoperative consultation, the results underscored that the inclusion of cytology in the intra operative diagnostic procedure enhanced its concordance with the definitive histopathological diagnosis. The results showed an improvement in the identification of the negative and true positive cases and a decrease in the proportion of the false positive diagnoses. Unnecessary radical surgeries for benign diseases or inadequate surgeries in cases of malignant disease may be thus avoided.
Specific ovarian neoplasms show characteristic cytological patterns and morphologies, thus suggesting almost accurate diagnoses. The knowledge on the patterns and the cell morphologies could help in the identification of ovarian neoplasms on cytology.
Khunamornpong et al., [12] studied the role of scrape cytology of the ovaries in an intraoperative consultation of ovarian lesions and found it to be a useful rapid cytodiagnostic tool. Michael et al., [14] compared cytology and frozen section in a study which was done on an intra operative consultation of ovarian lesions and found that the intra operative fine needle aspirations and scrapes were superior to the imprints.
Imprint cytology is the only method which gives the intraoperative diagnoses of ovarian tumours within 20 minutes, thus helping in tailoring the extent of the surgery. It is helpful, especially in young patients who need conservative surgeries in order to preserve their fertilities. Germ cell tumours can be managed by unilateral salpingoopherectomy, even if they are in the advanced stages, as these tumours are extremely sensitive to chemotherapy [15, 16].
The ability to deliver an immediate diagnosis by imprint cytology makes it an important part of the treatment at places where a frozen section facility is not available, which needs an advanced set up.
In conclusion, imprint cytology can be used as an adjunct to histopathology for a rapid and an early diagnosis, even in operation theatres, particularly in developing countries like ours, where the facility of frozen sections is often not available, since a rapid preliminary diagnosis may help in the surgical management planning.
Acknowledgement
We are thankful to Dr. Alvarez Santin C. et al., for allowing us to use study images of their article for this publication [17].(Post publication article amended on Oct 17, 2013)