Tuberculous Salpingitis: A Case Report
Annie Rajaratnam1, Prema D’Cunha2, Zevita Furtado3, Hilda Fernandes4
1 Assistant Professor, Department of Obstetrics & Gynaecology, Father Muller Medical College, Mangalore- 575002, Karnataka, India.
2 Professor, Department of Obstetrics & Gynaecology, Father Muller Medical College, Mangalore-575002, Karnataka, India.
3 Final Year Resident, Department of Microbiology, Father Muller Medical College, Mangalore-575002, Karnataka, India.
4 Professor, Department of Pathology, Father Muller Medical College, Mangalore-575002, Karnataka, India.
NAME, ADDRES, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Annie Rajaratnam, Assistant Professor, Department of Obstetrics & Gynaecology, Father Muller Medical College, Kankanady, Mangalore-575002, Karnataka, India.
Phone: 9449525915
E-mail: annierajaratnam@yahoo.com
Tuberculosis (TB) of the genital tract commonly occurs secondary to a primary lesion. The mode of spread is via the lymphatics, the haematogenous route or less commonly by a peritoneal spread. The fallopian tubes are the first targets, followed by the pelvic organs. Isolated cases of TB which occur in a unilateral fallopian tube are rare, particularly with it as a primary site. The aim of this study was to report a rare case of TB of the left fallopian tube in a post menopausal lady with no positive history, clinical or laboratory finding to suggest it to be a secondary focus. As the pre-operative diagnosis was that of a right ovarian neoplasm, the patient underwent staging laparotomy. TB of the left fallopian tube was diagnosed, as there were numerous typical granulomata throughout the fallopian tube.
Tuberculous salpingitis, Genital tuberculosis, Primary foci
INTRODUCTION
The prevalence of genital TB in the female population is 1-2% [1]. Genital TB is difficult to diagnose, as most of the cases are asymptomatic [2] and as they usually occur between the ages of 20-40 years. The women with genital TB may present with low grade fever, pelvic pain, menstrual irregularities, infertility and secondary amenorrhoea [3]. Genital TB begins simultaneously in both the fallopian tubes and then it spreads to the rest of the genital tract [4]. The ampullary region shows the earliest and the most extensive changes [5]. Primary tuberculosis of the fallopian tube is rare.
CASE REPORT
A 55 years old, P4L4, post menopausal lady presented with lower abdominal pain of two weeks duration. The pain was dull and continuous. She had no fever, weight loss or abnormal vaginal discharge. She had no past or family history of TB.
On examination, her Body Mass Index (BMI) was found to be 28 and her other systems were normal. P/A: A 20x18 cm cystic mass was felt in the right iliac fossa, which arose from the pelvis and there was no free fluid. P/S: The vagina and the cervix were healthy. P/V: The uterus was normal in size and mobile and a right adnexal mass of 20x18 cm was felt. The left fornix was free. Investigations: Hb: 11gms%, Total count: 6500 and ESR:17mm/hr. The liver and renal function tests were normal. CA-125 was 82.38u/ml. The urine culture showed no growth. The PAP smear was negative for malignant cells. The chest X-ray was normal. The ultrasound showed a mixed echoic mass of size, 10.5 x 5 x 5.7 cm in the right ovary. CT scan showed a 10.5 x 8 x 8.5cm right ovarian mass with mixed echogenecity. The lymph nodes were normal, with minimum free fluid in the abdomen. The risk malignancy index (the ultrasound features x the menopausal state x the value of CA-125) was 247.14. The preop diagnosis being that of an ovarian neoplasm, the patient was posted for a staging laparotomy. The per operative findings showed a right ovary of size, 10 x 8 x 8cm with torsion. The right fallopian tube, the uterus and the left adnexa were normal. [Table/Fig-1]. There was minimum free fluid. The rest of the abdomen was normal.
Per operative findings showing torsion of right ovarian cyst

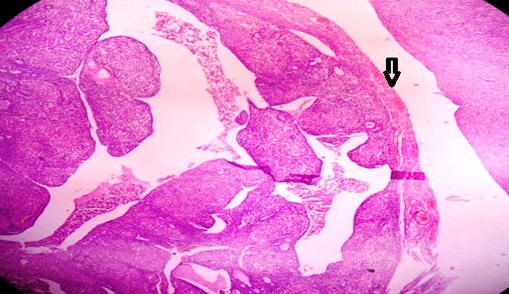
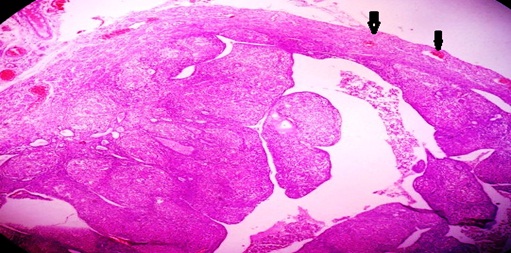
Histopathology: The peritoneal fluid was negative for malignant cells and Acid Fast Bacilli (AFB). The cervix showed chronic cervicitis and the endometrium revealed senile cystic atrophic changes. The right ovary showed diffuse areas of haemorrhage and infarction with a rim of viable ovarian stroma. The right tube and the left ovary were normal. The left tube showed the presence of multiple granulomas which were composed of aggregates of epithelioid histiocytes with scattered small lymphocytes and the Langhans type of multinuclear giant cells [Table/Fig-2a]. A scanner view which is showing the thinned wall of the tube (arrow) and the flattened epithelial folds with inflammation [Table/Fig-2b]. A scanner view of other portions of tube which is showing the congested peritubal vessels (arrows) and similar features as in [Table/Fig-2a], [Table/Fig-2c]. High power views showing multiple epitheloid granulomas (arrow) and the Langhans type of giant cells (star).
Scanner view showing thinned wall of the tube (arrow) and flattened epithelial folds with inflammation
Scanner view of the other portion of the tube showing congested peritubal vessels (arrows) and similar features as in [Table/Fig-2a]
High power view showing multiple epitheloid granulomas (arrow) and langhans type of giant cells (star)

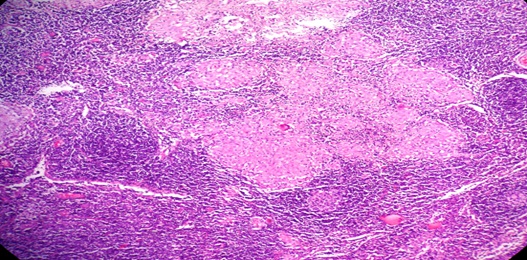
The pelvic lymph nodes showed granulomatous lymphadenitis which was suggestive of TB [Table/Fig-3]. The microscopic appearance was of tuberculous lymphadenitis of the pelvic lymph node, but AFB was negative. The omentum and the appendix were unremarkable. The post operative period was uneventful. Multidrug therapy is the main stay of the treatment and a short term treatment with antitubercular drugs for 6 months is effective for genital TB. Hence, the patient was started on the Category I treatment of Directly Observed Treatment Short Course (DOTS) ie. 2 (HRZE)3 as the intensive phase and 4 (HR) 3 as the continuation phase regimen, as it was considered to be a case of primary tubercular salpingitis.
Microscopic appearance of tuberculous lymphadenitis of the pelvic lymph node
DISCUSSION
The view that TB of the pelvic organs varies geographically, ethnically and with the type of patient, is a reflection of the lacunae in the knowledge and paucity of good studies [3]. Morgagni was the first to describe the signs of genital TB in women [2]. The wide variability in the extent and the site of the disease is due to the investigative procedures/techniques which are used [3]. Genital TB is always secondary and the patient may be unaware of the primary focus that is extragenital, which may most commonly be a pulmonary lesion [6]. Gynaecologists need to be aware that TB may present in an atypical manner. Genital TB is called “the great pretender” because it resembles the presentation of advanced ovarian carcinoma [7]. Though a microbiological proof is essential, the authorities may accept a histopathological proof (typical granuloma) to confirm the diagnosis of TB [8].
The criteria which are necessary for a diagnosis of primary genital TB are (1) the genital lesions should be the first tuberculous infections in the body and (2) the regional lymph nodes should demonstrate the same stage of the tuberculous development as do the genital organs [9]. Our case fulfilled both the criteria and hence, it was considered as a primary focus, as there was no history, clinical features or investigations to prove the involvement of any other organs or systems. Serum CA 125 is raised in peritoneal TB and in benign intra-abdominal conditions [10]. The raised CA 125 with active TB may be misinterpreted as ovarian cancer [7]. The tubes, ovaries and the serosal surface of the uterus may be involved in the peritoneal spread which originates from an intra abdominal lesion [2]. Our case did not have any intra-abdominal lesion.
Unilateral primary tubal TB is extremely rare, but due to the absence of a peritoneal lesion, tuberculosis of the fallopian tube is likely to be primary in origin [11] as in our case. Although culture methods are still the gold standard in the detection of genital tuberculosis, they are negative in one-third of the cases [12]. However, in the presence of risk factors/suggestive intra operative findings, the testing for TB in this set of the population who present with ectopic pregnancies may be justified, to prevent further morbidity, by initiating anti-tubercular therapy in the high prevalence areas [13].
A primary infection may occur if the male partner has active genito-urinary TB and the transmission is by sexual intercourse. In postmenopausal women, genital TB is rare and it constitutes 1% of the cases of postmenopausal bleeding. Our case did not have any history of a vaginal discharge, which correlated with the review reports of Gungorduk K et al., [14]. The exact cause of the low incidence of the disease in this age group is not known. Most of the authors believe that an atrophic endometrium is a poor milieu for the growth of the Mycobacterium tuberculosis bacilli [15].
Surely the future of a better and a reliable early diagnosis of genital TB lies in the development of a multiplex Polymerase Chain Reaction (PCR). A combination of suitable primers which target the repetitive sequences and the species specific gene sequences would be ideal, to detect more number of cases. A good history taking, along with a correct sampling with the use of various imaging modalities and the use of multiplex PCR, will certainly turn around the diagnostic difficulty of genital TB [16]. Thus, pelvic TB should be considered as a possibility in the women who present with a pelvic mass, in the absence of fever, ascites, and an elevated CA-125 level.
[1]. Seshadri Lakshmi, Essentials of gynaecology 2012 New DelhiWolters Kluwer Iindia Pvt Ltd [Google Scholar]
[2]. Tripathy SN, Tripathy SN, Gynaecological tuberculosis-An updateInd. J. Tub 1998 45:193 [Google Scholar]
[3]. Nagpaul Female genital tuberculosisThe Indian Journal of Tuberculosis 1991 38(4):187-88. [Google Scholar]
[4]. Rezvani Maryam, Shaaban Akram M, Fallopian tube disease in the non-pregnant patientRadiographics 2011 31:527-48. [Google Scholar]
[5]. Varma Thankam R, T. Tuberculosis of the female genital tractGlobal library for women’s medicine. Chennai 2008 [Google Scholar]
[6]. Maclean AB, Pelvic InfectionGreat Britian 1995 C.R. Whitfield [Google Scholar]
[7]. Botha MH, van der Merwe FH, TitleSA Fam Pract 2008 50(5):12-16. [Google Scholar]
[8]. Namavar Jahromi B, Parsanezhada ME, Ghane-Shirazi R, Female genital tuberculosis and infertilityInt J Gynaecol Obstet 2001 75:269-72. [Google Scholar]
[9]. Auerbach O, Tuberculosis of the female genital organsSurg Gynecol Obstet 1942 75:712 [Google Scholar]
[10]. Piura B, Rabinovich A, Leron E, Yanai-Inbar I, Mazor M, Peritoneal tuberculosis-An uncommon disease that may deceive the gynecologistEur J Obstet Gynecol Reprod Biol 2003 110(2):230-34. [Google Scholar]
[11]. Jones H Macnaughton, Primary Unilateral Tuberculosis of the Fallopian TubeBrit. Med. Journ 1884 177:87 [Google Scholar]
[12]. Seth Ankit, Kudesia Madhur, Gupta Kusum, Pant Leela, Mathur Anjali, Cytodiagnosis and pitfalls of genital tuberculosis: A report of two casesJ Cytol 2011 28(3):141-43. [Google Scholar]
[13]. Banerjee A, Prateek S, Malik S, Dhingra D, Genital tuberculosis in adolescent girls from low socioeconomic status with acute ectopic pregnancy presenting at a tertiary care hospital in urban Northern India: are we missing an opportunity to treat?Arch Gynecol Obstet 2012 286(6):1477-82. [Google Scholar]
[14]. Gungorduk K, Ulker V, Sahbaz A, Ark C, Tekirdag AI, Post menopausal tuberculous endometritisInfect Dis Obstet Gynecol 2007 2007:27028 [Google Scholar]
[15]. Mondal SK, Dutta TK, Nag DR, Biswas PK, Sinha MG, Histopathologic analysis of female genital tuberculosis with clinical correlation.A fifteen year study in a tertiary hospital of IndiaJ Basic Clin Reprod Sci 2012 1:25-29. [Google Scholar]
[16]. Bose Mridula, Female genital tract tuberculosis: How long will it elude diagnosis?Indian J Med Res 2011 134(1):13-14. [Google Scholar]