Desmoplastic Melanoma: A Diagnostic Dilemma
Ashwin K Alva1, Rajeshwara K V2, Udaykumar3
1 General Surgery, Senior Resident, Father Muller Institute of Medical Education and Research, Kankanady, Mangalore-575002, D.K Karnataka, India.
2 General Surgery, Assistant Professor, Father Muller Institute of Medical Education and Research, Kankanady, Mangalore-575002, D.K Karnataka, India.
3 General Surgery, Father Muller Institute of Medical Education and Research, Kankanady, Mangalore-575002, D.K Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajeshwara KV, Assistant Professor, Department of General Surgery, Father Muller Medical College, Kankanady, Mangalore-575002, India.
Phone: +919632961340
E-mail: drrajeshwarakv@gmail.com
Desmoplastic melanoma (DM) is an uncommonly encountered type of melanoma. A pigmentation is frequently absent, although a lentigo or lentigomaligna-like discolouration, adjacent to the nodule, is not uncommon. Hence, the clinical impression at presentation may vary from those of basal cell or squamous cell carcinomas, dermatofibromas or sarcomas to cysts and indurated plaque-like lesions which resemble scars. Making a cinical diagnosis of this tumour is difficult and it may very often mislead the physician.
The clinical appearance of DM may be highly variable and the diagnosis of the tumour is difficult. We are reporting a case of DM which was diagnosed histopathologically and confirmed by immunohistochemistry (IHC), for its rarity and unique presentation.
Demoplastic, Immunohistochemistry
CASE REPORT
An 80 years old female presented with the complaint of a non healing ulcer over the sole of the left foot, of four year’s duration, which was associated with bleeding on trivial trauma. It had initially started as a small bleb which had burst open to form an ulcer and it had gradually increased to the present size. She gave a history of itching and pigmentation in the surroundings the lesion, which was of recent onset.
Clinical Examination:
A solitary ulcer was noted over the plantar aspect of the left foot, 1 cm below the fifth metatarsophalangeal joint, which measured 4 by 4 cm in size, with regular rounded borders and patchy black pigmented areas along the boundary [Table/Fig-1]. The pigmentation had variegated shades. The floor of the ulcer was filled with an exuberant, unhealthy, granulation/tumour tissue with minimal serous discharge. No induration was noted surrounding the lesion and only a single node palpated in the left inguinal region, which belonged to the superficial group.
Clinical photograph of the ulcer over the sole of left foot

Investigations:
An edge biopsy of the ulcer raised the suspicion of a desmoplastic variant of malignant melanoma, following which IHC was done, which showed a strong positivity for S-100 and a negativity for HMB-45. Ultrasound guided fine needle aspiration of the groin node was negative for tumour deposits. A metastatic work up which was taken up in the form of a chest radiograph, abdominal ultrasonography and liver functions were normal. According to Lens MB et al., [1], the development of regional metastases was rare, the incidence ranging from 0-18.8%. Regional lymph node metastases occurred in 50 patients (7.1%), while systemic metastases developed in 139 patients (19.8%).
Management:
The patient underwent wide local excision of the lesion in the form of a forefoot amputation and primary closure of the amputation stump, with an inguinal node biopsy.
Histopathological Findings:
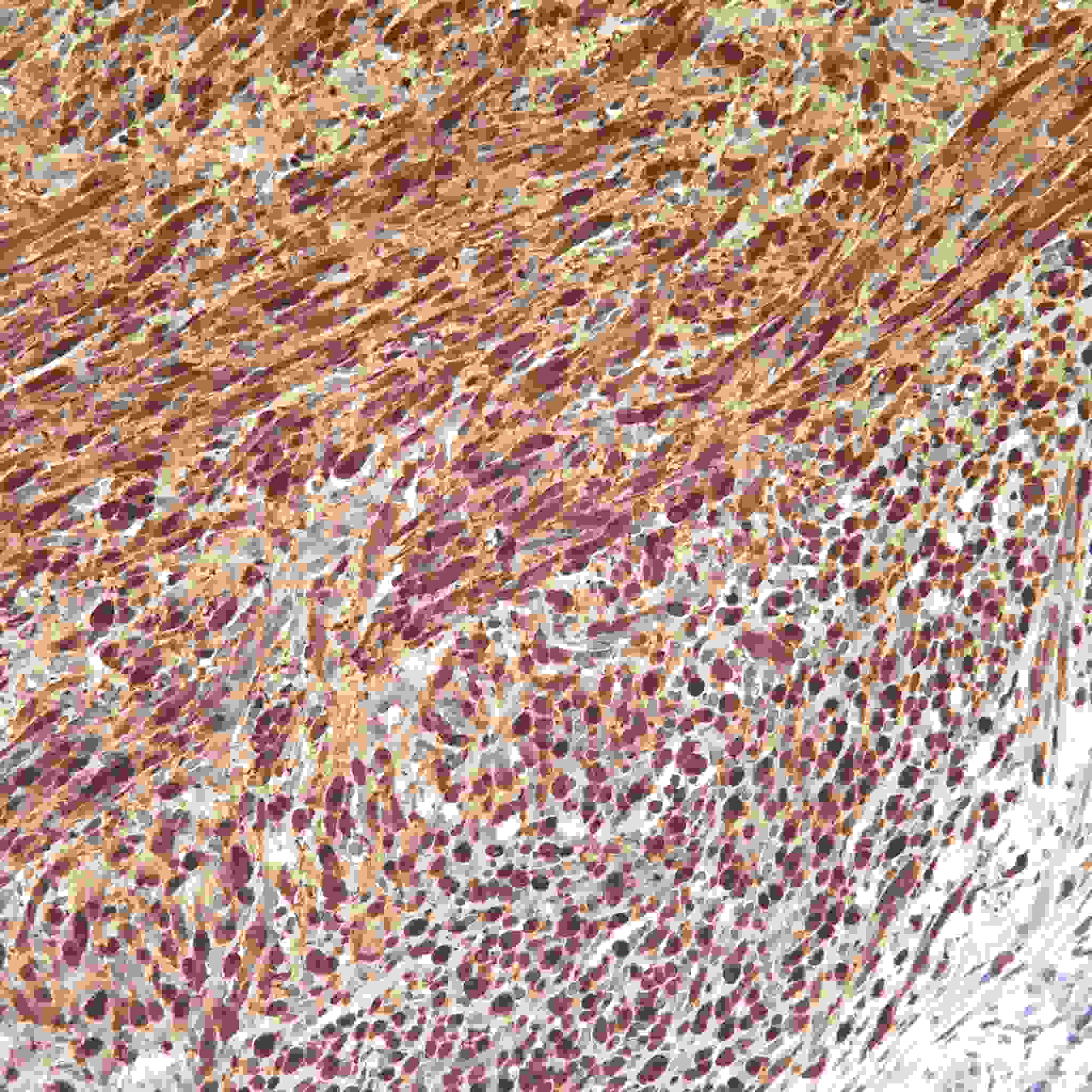
The sections showed a tumour which was composed of neoplastic spindle cells which were arranged in nests, trabeculae, fascicles, and cords. The intervening stroma was dense and fibrocollagenous, with desmoplasia [Table/Fig-2]. The S-100 staining showed a strong positivity [Table/Fig-3]. Hence, all the features favoured a diagnosis of DM, with all the margins being free of the tumour and the node being free of tumour deposits. The Clarks staging was level 4, which was in comparison with those of the cases of Lens MB et al., [1] , where most of the DMs belonged to the Clark levels 4 and 5.
Low power view of the intradermal tumour
Microscopic picture of the S-100 positivity
DISCUSSION
Malignant melanoma may express a variety of phenotypes, with different clinical and cytopathological features. DM is an uncommonly encountered type of melanoma which was first described by Conley et al., [2] in 1971, as an invasive melanoma which was composed of spindle cells which were surrounded by abundant collagen. Desmoplastic melanoma (DM) is an uncommonly encountered type of melanoma. Pigmentation is frequently absent, although a lentigo or lentigo maligna-like discoloration adjacent to the nodule is not uncommon [3].
The clinical appearance can be highly variable and it may mimick a variety of different lesions. Usually, it has an innocuous clinical appearance and is described as an indurated papule or nodule. Hence, the clinical impression at presentation may vary from those of basal cell or squamous cell carcinomas, sarcomas, dermatofibrosarcomas or sarcomas to cysts and indurated plaque like lesions [4].
There is a lack of statistically significant studies on the behaviour of DM, due to the small number of patients which was included in the studies, the patients’ advanced ages and the short follow-ups.
In this case, the lesion was located on the lower extremity. According to the critical review of Lens MB et al., [3], the lesions were most commonly located on the head and neck (53.2%), followed by the extremities (26.2%) and the trunk (20.6%). We had thought of basal cell carcinoma, squamous cell carcinoma and malignant melanoma as the differential diagnoses, only to prove by biopsy, that it was a case of DM. DM is characterized histologically by dermal and subcutaneous infiltrates of spindle shaped cells which are arranged singly or in thin fascicles within a prominent collagenous stroma. Thus, DM can be difficult to diagnose microscopically by the conventional haematoxylin and eosin staining. IHC is often recommended [5–9] for S-100. The sections showed a tumour which was composed of neoplastic cells which were arranged in nests, trabeculae, fascicles, and cords. The intervening stroma was dense and fibrocollagenous, with desmoplasia. The S-100 staining showed strong positivity. Hence, all the features favoured a diagnosis of DM.
This case has been reported in view of the rarity of the desmoplastic variant as such and also because of the confusion that prevailed in the pre-operative diagnosis.
[1]. Lens MB, Newton-Bishop JA, Boon AP, Desmoplastic malignant melanoma: a systematic reviewBr J Dermatol 2005 Apr 152(4):673-8. [Google Scholar]
[2]. Conley J, Latterly R, Orr W, Desmoplastic malignant melanoma (a rare variant of spindle cell melanoma)Cancer 1971 28:914-36. [Google Scholar]
[3]. Bruijn JA, Mihm MC Jr, Barnhill RL, Desmoplastic melanomaHistopathology 1992 20:197-205. [Google Scholar]
[4]. Sangueza OP, Requena L, Neoplasms with neural differentiation: a review. Part II. Malignant neoplasmsAm J Dermatopathol 1998 20:89-102. [Google Scholar]
[5]. Busam J, Desmoplastic MelanomaClinics in Laboratory Medicine 2011 31(2):321-330. [Google Scholar]
[6]. Reed Richard J, Leonard Donald D, American Journal of Surgical Pathology3(4) [Google Scholar]
[7]. Sheilds JA, Elder D, Arbizo V, British Journal of Ophthalmology71(4):279-284. [Google Scholar]
[8]. Herbert M, Reiman MD, Goeliner John R., Cancer60(9):2269-2274. [Google Scholar]
[9]. Jain S, Allen PW, Desmoplastic Malignant Melanoma and its variantsAmerican Journal of Surgical Pathology13(5) [Google Scholar]