MRI Sequence and Characteristic Features in ‘Giant Cell Tumor’ of Clivus
Ajit Mahale1, Dhananjaya K.V.N2, Muralidhar Pai3, Vinaya Poornima4, Kausalya Kumari Sahu5
1 Professor, Department of Radiodiagnosis, KMC Attavar, Mangalore, Karnataka-575001, India.
2 Senior Resident, Department of Radiodiagnosis, KMC Attavar, Mangalore, Karnataka-575001, India.
3 Professor, Department of Neuro-Surgery, KMC Attavar, Mangalore, Karnataka-575001, India.
4 Associate Professor, Department of Radiodiagnosis, KMC Attavar, Mangalore, Karnataka-575001, India.
5 Associate Professor, Department of Pathology, KMC Attavar, Mangalore, Karnataka-575001, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dhananjaya K.V.N, Senior Resident, Department of Radiodiagnosis, KMC Attavar, Mangalore, Karnataka-575001, India.
Phone: 9844546546 Email: dhananjayakvn@gmail.com
Giant cell tumours of the clivus are rare. These tumours present in the second and third decades of life and they are slightly more frequent in women than in men. We are presenting a case of a 20 years young patient who came with the complaints of headache, retro-orbital pain and recurrent transient bleeding from the nose since two and half months. MRI of the brain with contrast was done and its features were suggestive of a Giant cell tumour of the clivus. A transnasal endoscopic biopsy was done under general anaesthesia and the histopathology report suggested that the features were of a giant cell tumour. Excision of the mass was done by Transnasal endoscopy. Post operatively, the patient did not recover from the lateral rectus palsy which was there on the right side. The patient was discharged with an advice of a follow up and radiotherapy. Radiation therapy and chemotherapy may be effective as adjuvant treatments. Even though a recurrence usually occurs within 4 years of the initial treatment, these patients will need to be carefully followed for the remainder of their lives.
Clivus, Tumour, Osteogenic, MRI
INTRODUCTION
Giant cell tumours of the bone usually occur in the epiphysis of the long bones; especially those which occur in the distal femur, the proximal tibia, and the distal radius account for 60-70% of the giant cell tumours in adults, with a peak incidence between the third and fourth decades of life [1]. Giant cell tumours comprise 5% of all primary bone tumours and they occur mostly around the knee joint; 2-5% occur in the vertebrae, and 5 to 10% occur in the sacrum [2]. These tumours rarely occur in the skull, and they comprise less than 1% of all the reported giant cell tumours of the bone [3,4]. Their occurrence below the age of 15 years, is mostly unusual. The benign giant cell tumours of the bone are believed to arise from the non-osteogenic stromal cells of the bone marrow, in the region of the epiphysis [5]. Embryologically, the sphenoid and the temporal bones are generated through an endochondral bone formation, except for the greater wings and the pterygoid processes of the sphenoid. In contrast, the other skull bones are produced by an intramembranous bone formation. It has been suggested that this difference in their genesis may be related to the relative absence of these tumours in the other calvarial bones [6].
CASE DESCRIPTION
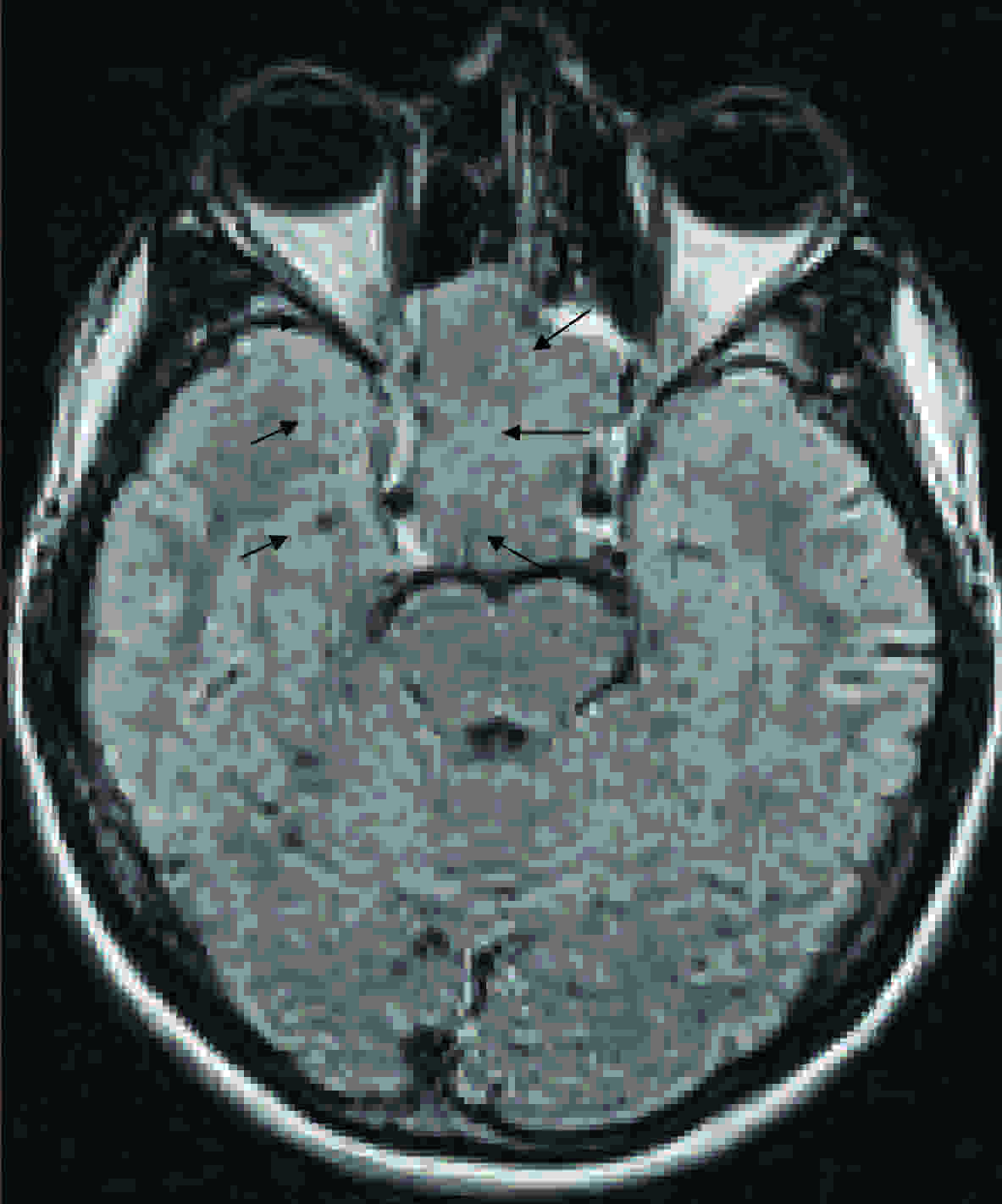
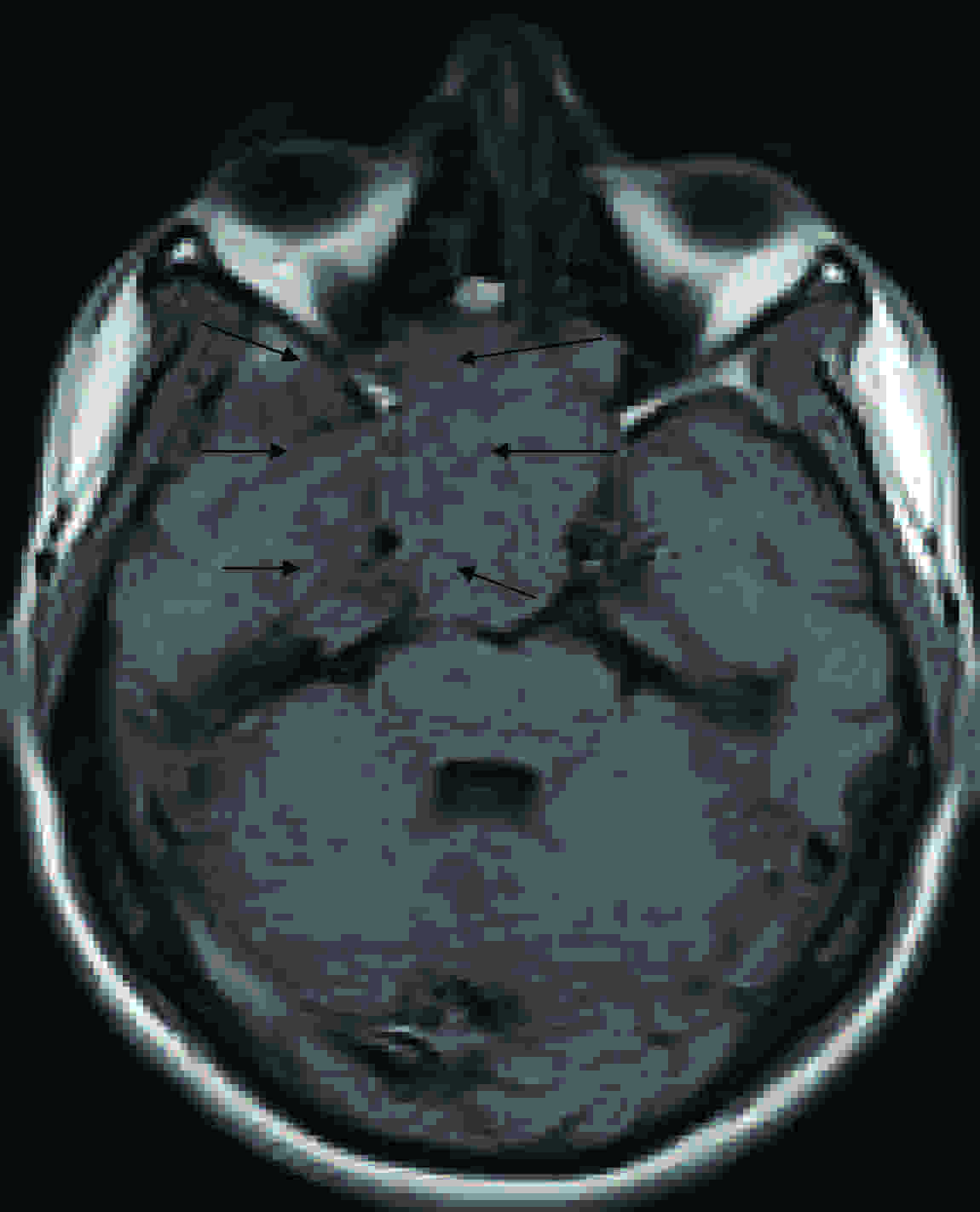
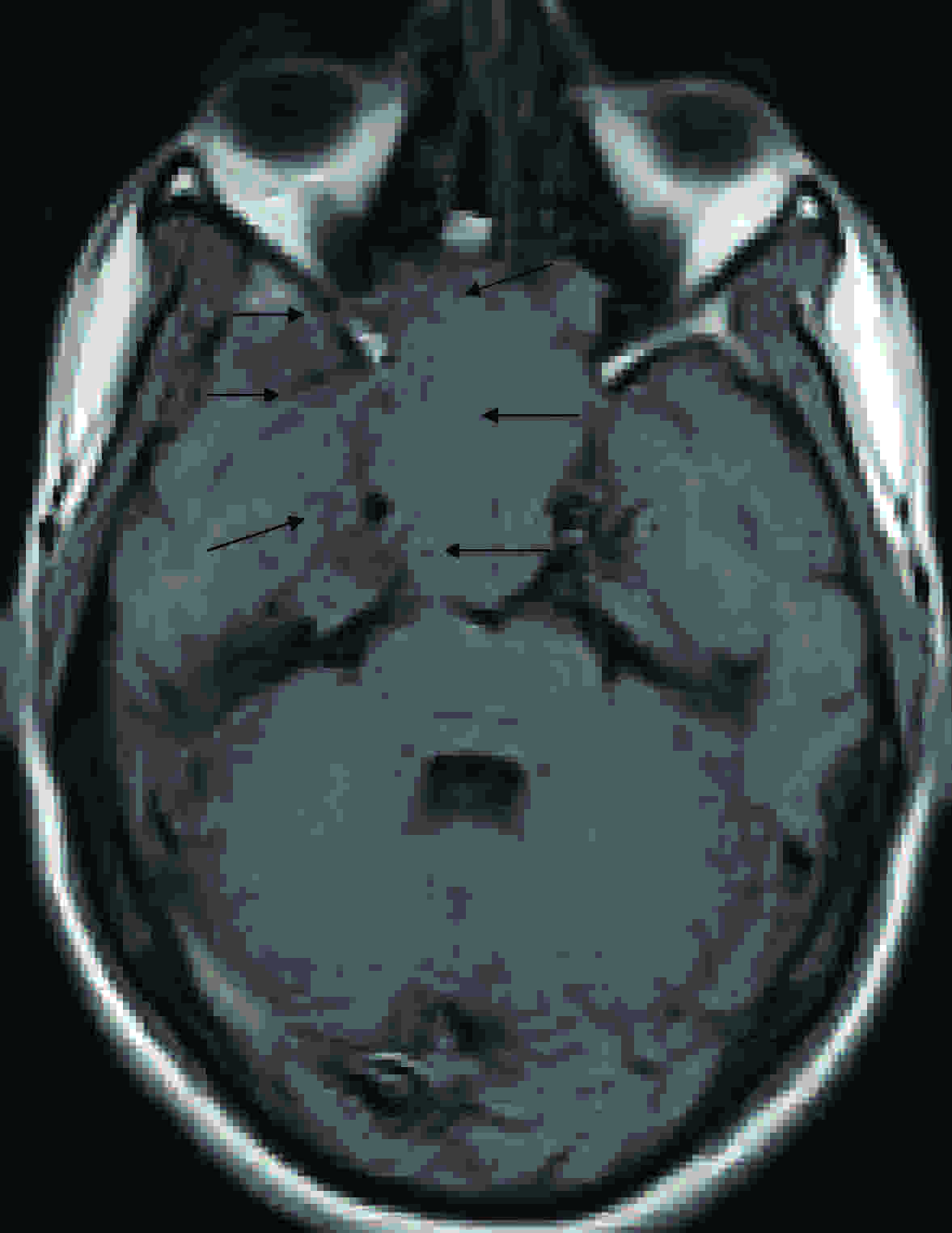
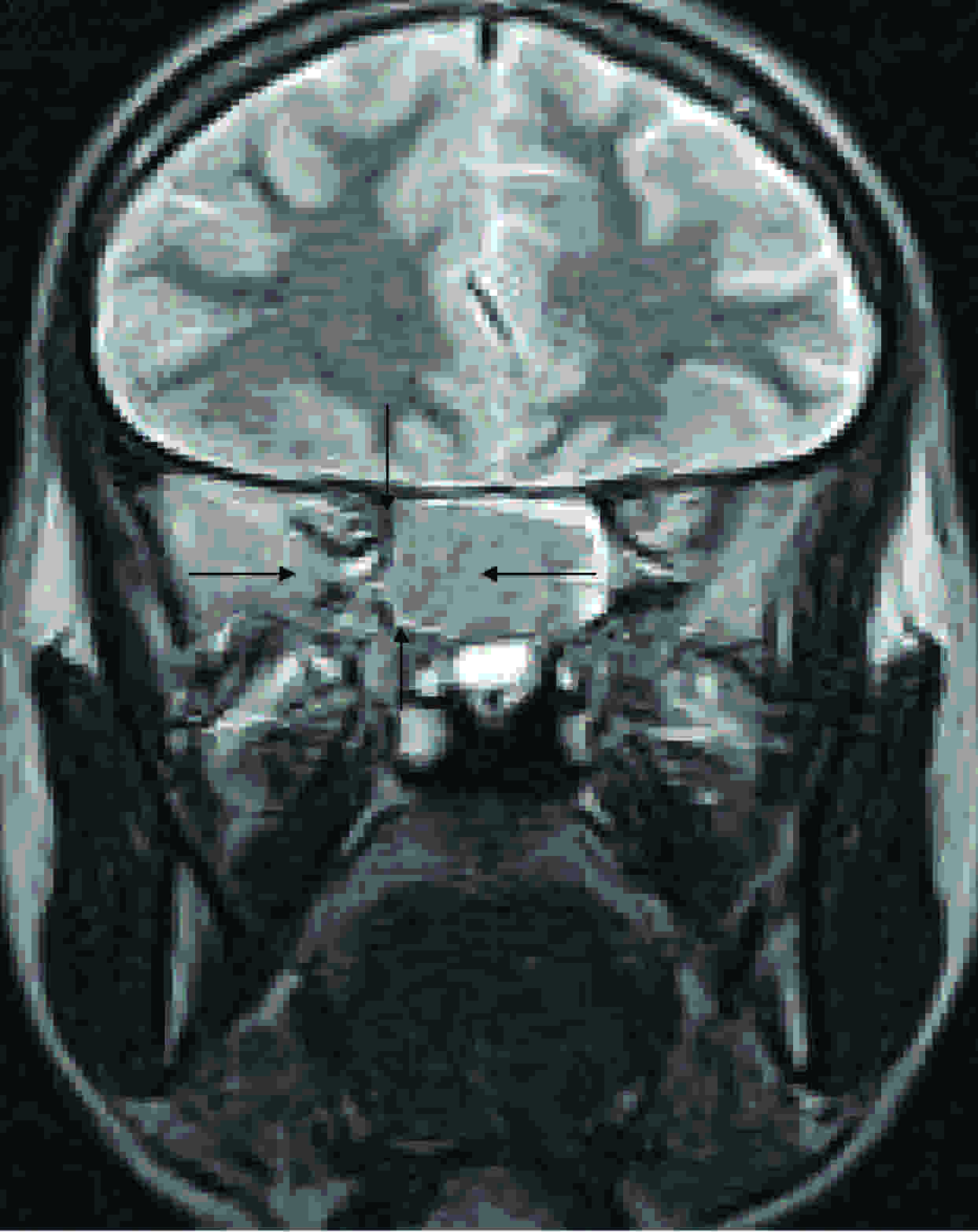
A 20 years old male patient came with the complaints of headache, retro-orbital pain and recurrent transient bleeding from the nose since two and a half months. He also complained of restricted right eye movements with double vision since two months and redness of the left eye since two months. There was no history of fever or trauma. On examination, his pulse rate was found to be 88/minute and his blood pressure was 120/80 mm Hg. The patient did not have any facial dysmorphism. Both his eyes showed chemosis. An ophthalmic examination showed a restricted field of vision, a restricted abduction movement and diplopia in the right eye, with normally reacting bilateral pupils and no glaucomatous changes in the optic discs. An endoscopic nasal examination which was done was normal, with no evidence of fresh bleeding or mass lesions in the nasal cavity and in the nasopharynx. 6th cranial nerve palsy was seen on the right side. The rest of the cranial nerves were normal. There was no other motor or sensory deficit. The other systems were found to be normal on examination. The blood investigations were within normal limits. Ultrasound scans of the abdomen and the pelvis were done, which showed hepatomegaly with fatty changes and a diffuse, hypoechoic pancreas. MRI of the brain with contrast was done and it reported a large, lobulated, Suprasellar and sellar mass lesion which measured 6.6x3x3 cms, which was iso to hypointense on the T1-, T2- and the FLAIR images [Table/Fig-1,2,3,4 and 5], with uniform, moderate enhancement on the post contrast images [Table/Fig-6,7,8 and 9]. The mass lesion extended into the ethmoid and the sphenoid bones and into the clivus posteriorly and also upto the anterior margin of the prepontoine cistern, reaching upto the posterior margin of the nasal septum and inferiorly indenting the nasopharyngeal region, causing widening of the sella and erosion of the bony sella. The pituitary and the stalk were not separable from the mass lesion. The mass lesion appeared to compress the optic nerves and to cause mild indentation on the anterior pons. The features were likely to be of a Giant cell tumour of the clivus, as was suggested by a histopathological examination correlation. The lab tests for CPS were negative. The tumour marker serum acid phosphatase level was normal. The chest radiograph was normal.
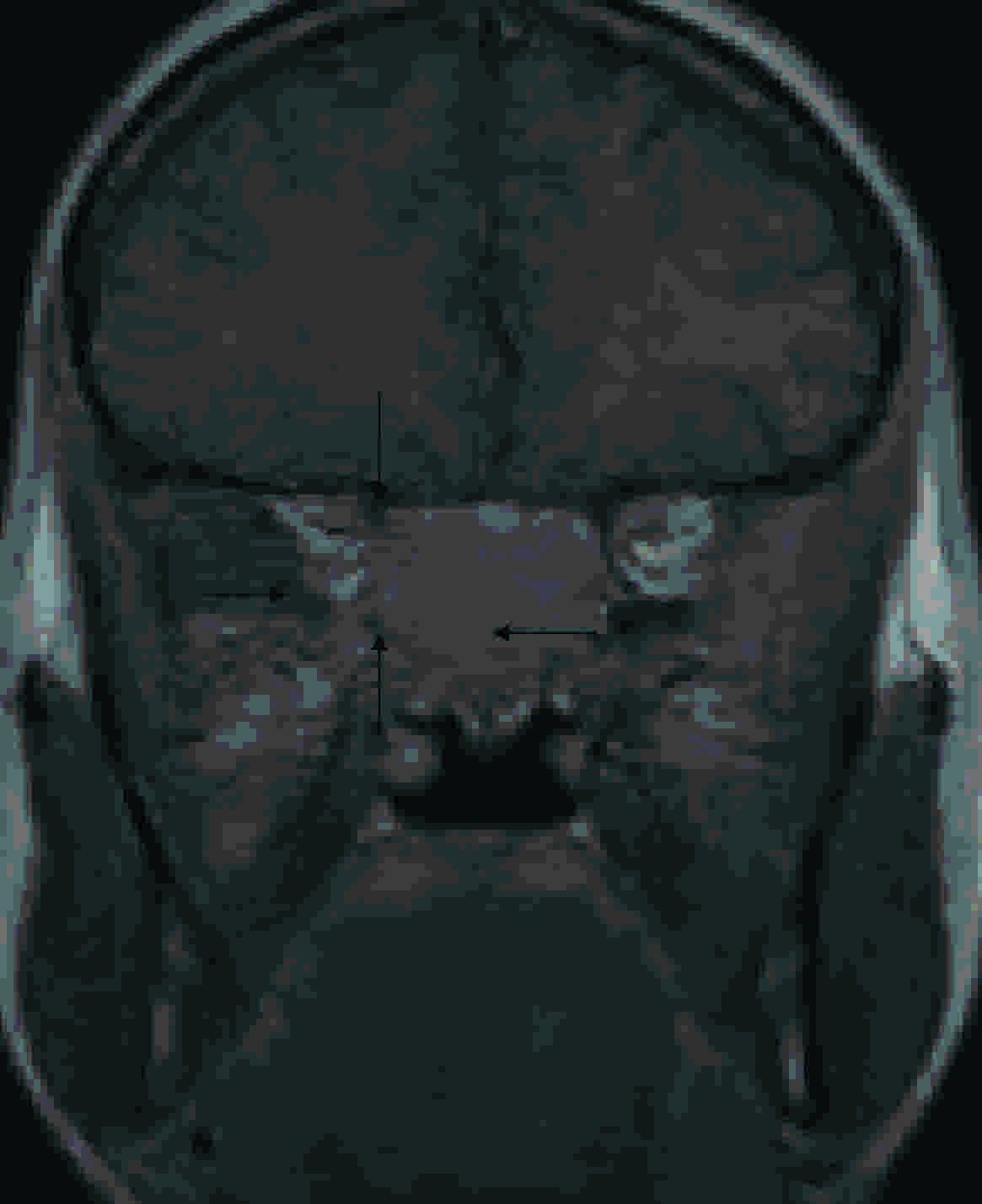
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Axial FlAIR images showing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Axial T2 FSE images showing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Axial T1 SE images showing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Coronal T2 FSE images showing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)
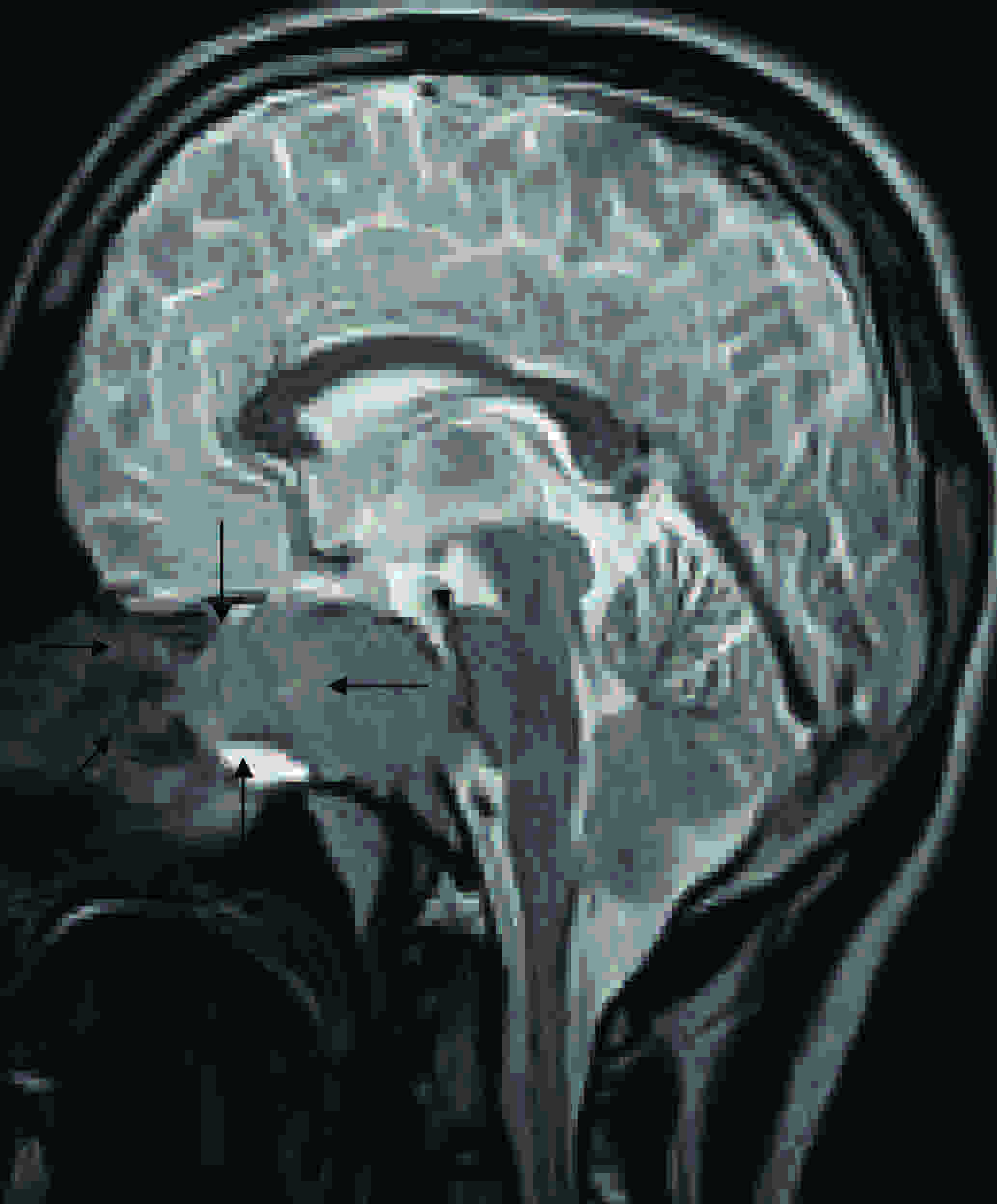
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Sagittal T2 FSE images showing large lobulated iso to hypo intense mass lesion in the region of clivus (Arrow marks)
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Coronal T1 SE post contrast images showing large lobulated moderately enhancing iso to hypointense mass lesion in the region of clivus (Arrow marks)
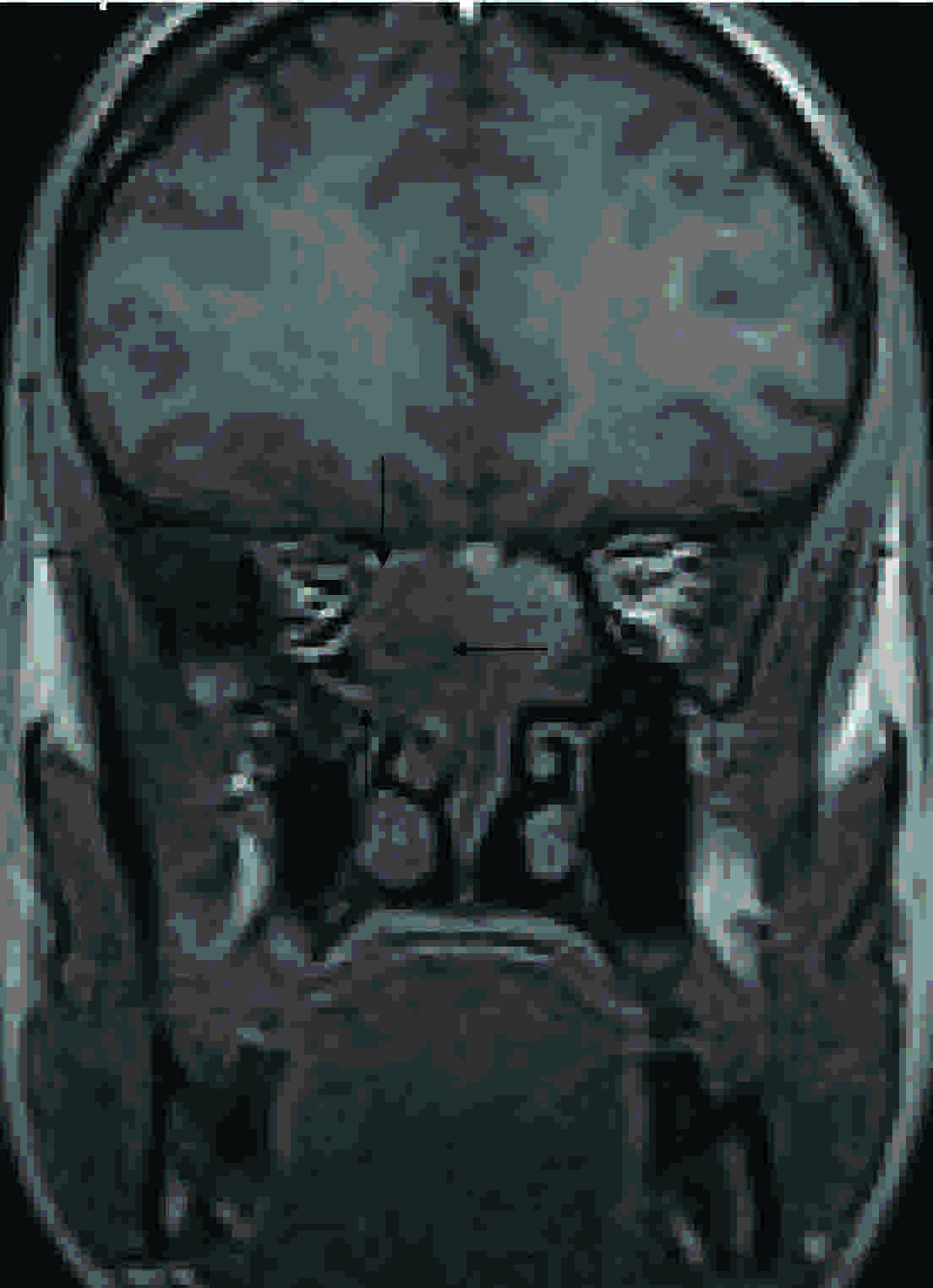
12 years old male child with headache, retroorbital pain and ophthalmoplegia. Coronal SPGR post contrast images showing moderately enhancing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)

12 years old male child with headache, retroorbital pain and ophthalmoplegia. Sagittal T1 SE post contrast images showing moderately enhancing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)

12 years old male child with headache, retroorbital pain and ophthalmoplegia. Sagittal SPGR post contrast images showing moderately enhancing large lobulated iso to hypointense mass lesion in the region of clivus (Arrow marks)
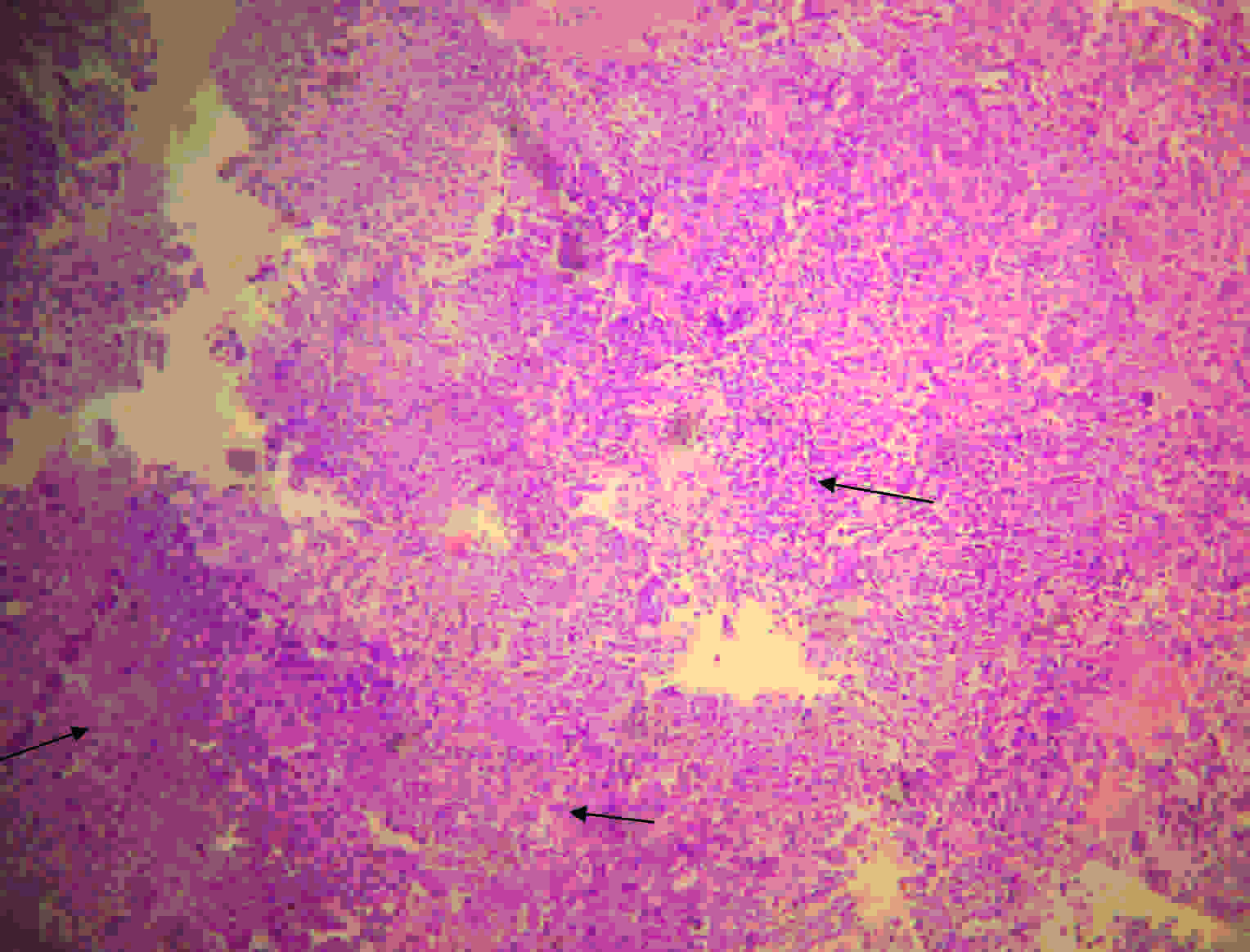
A transnasal endoscopic biopsy was done under general anaesthesia and it was sent for a histopathological examination. The tumour tissue was seen in the posterior part of the basal cavity (the middle meatus) through a transnasal approach. A very vascular but a friable tumour tissue was seen and a biopsy was taken from this site. It extended through the sphenoid sinus. The bone was completely eroded. No flare was seen and there was no normal morphology. A biopsy was taken and on gross examination, it was found to be dark-brown to pale white in colour. On microscopy, a tumour tissue was seen, which was composed of numerous, multinucleated, osteoclastic giant cells which were scattered on a background of oval to spindle shaped mononuclear cells with eosinophilic cytoplasm and hyperchromatic to vesicular nuclei, some with prominent nucleoli. Areas of necrosis, haemorrhage, inflammatory cells, fibrocartilagenous tissue, and bony trabeculae were seen. The features were of a giant cell tumour [Table/Fig- 10]. Excision of the mass was done by Transnasal endoscopy and the middle meatus was followed to reach the old biopsy site. The lesion was soft and suckable. An excision was done as much as possible. Its clearance was confirmed on the C-arm. It extended upto the sella, where there was a poor plane of delineation. Haemostasis was achieved and the nasal cavity was packed. Post operatively, the patient did not recover from the lateral rectus palsy which was there on the right side. The serum acid phosphatase level was below pre-operative levels. The patient was discharged with an advice of a follow up and radiotherapy.
12 years old male child with headache, retroorbital pain and ophthalmoplegia. On microscopy there was tumor tissue composed of numerous multinucleated osteoclastic giant cells (Arrow marks) scattered in a background of oval to spindle shaped mononuclear cells with eosinophilic cytoplasm and hyperchromatic to vesicular nuclei, some with prominent nucleoli. Areas of necrosis, hemorrhage, inflammatory cells, fibrocartilagenous tissue, and bony trabeculae are seen. Features are of giant cell tumor
DISCUSSION
Giant cell tumours of the sphenoid are rare [7]. These tumours, which present in the second and third decades of life and are slightly more frequent in women than in men, may present with various symptoms, which include headache, visual field defects, blindness, and diplopia [8]. When they do occur in the base of the skull, a surgical treatment is frequently difficult and therefore, the use of an adjuvant therapy is important [1,9]. A combination of surgery and radiotherapy is essential for the giant cell tumours which occur in the sites where an access is difficult [7]. Radiation therapy and chemotherapy may be effective as adjuvant treatments, especially when either the lesions are anatomically inaccessible or when a surgical excision is judged to be incomplete [10]. A Giant cell tumour of sphenoid responds well to adriamycin after a partial removal of the tumour [1]. It is conventionally treated with chemotherapeutic agents which consist of methotrexate, adriamycin, and cyclophosphamide, based on the strategies that have been successfully established for the treatment of sarcomas [11,12]. Two disadvantages of radiotherapy are, that the tumour is radioresistant and that there is a malignant transformation in the giant cell tumour [1,2,4,13,14]. Even though a recurrence usually occurs within 4 years of the initial treatment [13], these patients will need to be carefully followed for the remainder of their lives [1].
These tumours are locally aggressive, with a high rate of a local recurrence and a low potential for a distant metastasis [15]. Giant cell tumours of the sphenoid bone, despite their benign histologic appearance, may also be clinically devastating, because of their location and their capacity for the local destruction of the vital structures [13,16,17]. Endocrine abnormalities are relatively uncommon [7]. These insidiously growing, generally benign, solitary lesions are moderately well vascularized. They consist of mononuclear ovoid and spindle-shaped stromal cells which resemble young connective tissue. The nuclei contain moderate amounts of chromatin with centrally located nucleoli. Mitoses may be present. The cytoplasm may be diffusely granular or vacuolated. Characteristically, the multinucleated giant cells which have a similar granular or foamy cytoplasm are found among the stromal cells. In view of the similarities that can be found between the nuclei of the stromal and the multinucleated cells, the stromal cells can be regarded as the forerunners of the giant cells [5]. Multinucleate giant cells may be found in neoplastic or nonneoplastic bone lesions, as well as in the giant cell tumours of the bone. They are also found in osteosarcomas, chondroblastomas, malignant histiocytomas, and chondromyxoid fibromas. In nonneoplastic processes, the “brown tumour” of hyperparathyroidism, the giant cell reparative granuloma, and the aneurismal bone cyst are commonly associated with a giant cell population [18]. Among the lesions which occur in the sphenoid bone, that contain giant cells, the giant cell granulomas may be confused with the true giant cell tumours of the bone, although the former tend to occur in younger patients [19].
Modern imaging techniques have proved to be of immense value in the localization of the skull base lesions, and this is particularly true of the MR images that demonstrate the vascular structures without the need of angiography [7]. Attempts have been made to grade the giant cell tumours of the bone on the basis of the cytological features, such as the presence and the prominence of the nucleoli, the numbers of the giant cells, and the abundance of the mitotic figures. Because giant-cell tumours of the bone are histologically benign lesions, we do not grade these tumours [8].
[1]. Masaaki Yamamoto, Takeo Fukushima, Seisaburo Sakamoto, Masamichi Tomonaga, Giant cell tumor of the sphenoid bone: Long-term follow-up of two cases after chemotherapySurg Neurol 1998 49:547-52. [Google Scholar]
[2]. Dahlin DC, Cupps RE, Johnson EW, Giant cell tumor: a study of 195 casesCancer 1970 25:1061-70. [Google Scholar]
[3]. Dahlin DC, Giant cell tumor of bone: highlights of 407 casesAJR 1985 144:955-60. [Google Scholar]
[4]. Goldenberg RR, Campbell CJ, Bonfiglio M, Giant cell tumor of bone: an analysis of two hundred eighteen casesJ Bone Joint Surgery [Am] 1970 52:619-64. [Google Scholar]
[5]. Geissinger JD, Siqueira EB, Ross ER, Giant Cell Tumors of the Sphenoid BoneJ Neurosurg 1970 32:665-70. [Google Scholar]
[6]. Pitkethly DT, Kempe LG, Giant cell tumors of the sphenoid. Report of two casesJ Neurosurg 1969 30:301-04. [Google Scholar]
[7]. Laurence DW, David U, Daniel JA, Peter W, Nicholas P, Giant Cell Tumor of the Sphenoid BoneNeurosurgery 1992 30(4):576-81. [Google Scholar]
[8]. Wolfe JT III, Scheithauer BW, Dahlin DC, Giant cell tumor of the sphenoid bone: Review of 10 casesJ Neurosurg 1983 59:322-27. [Google Scholar]
[9]. Kemeny AA, Afshar F, Giant cell tumor of the sphenoid bone with coincidental galactorrhoea-a case reportBr J Neurosurg 1990 4:343-46. [Google Scholar]
[10]. Bertoni F, Present D, Enneking WF, Giant cell tumor of the bone with pulmonary metastasesJ Bone Joint Surg 1985 67A:890-900. [Google Scholar]
[11]. Kaise U, Neuamann K, Havemann K, Generalised giant cell tumor of bone: succeful treatment of pulmonmary metastase with interferon a, a case reportJ Cancer Res Clin Oncol 1993 119:301-03. [Google Scholar]
[12]. Rossen G, Caparros B, Huvos AG, Kosloff C, Nirenberg A, Cacavio A, Preoperative chemotherapy for osteosarcoma: selection of postoperative adjuvant chemotherapy based on the response of primary tumor to preoperative chemotherapyCancer 1981 49:1221-30. [Google Scholar]
[13]. Emley WE, Giant cell tumor of the sphenoid bone. A case report and the review of literatureArch Otolaryngol 1971 94:369-74. [Google Scholar]
[14]. Bitoh S, Takimoto N, Nakagawa H, Namba J, Sakaki S, Gohma T, Giant cell tumor of the skullSurg Neurol 1978 9:185-88. [Google Scholar]
[15]. Bennett CJ, Marcus RB, Million RR, Enneking WF, Radiation therapy for giant cell tumor of boneInt J Radiat Oncol Bio Phys 1993 26:299-304. [Google Scholar]
[16]. Bertoni F, Unni KK, Beabout JW, Ebersold MJ, Giant cell tumor of the skullCancer 1992 70:1124-32. [Google Scholar]
[17]. Wolfe JT, Scheithauer BW, Dahlin DC, Giant cell tumor of the sphenoid bone. Review of 10 casesJ Neurosurg 1983 59:322-27. [Google Scholar]
[18]. Robins SL, Cotrem RS, Kumar V, The Pathological Basis of Disease 1984 3rd edPhiladelphiaWB saunders Co [Google Scholar]
[19]. Ciapetta P, Salvati M, Bernardi C, Raco A, Di Lorenzo N, Giant cell reparative granuloma of the skull base mimicking an intracranial tumorSurg Neurol 1990 33:52-56. [Google Scholar]