Odontogenic infections have become one of the major sources of fascial space infections in the head and neck region, which have the potential to spread via the fascial spaces [1]. They can compromise the vital structures in this region or involve the distant structures. Although they are spatially confined, the purulent material may spread deeply into the contiguous fascial spaces such as the submandibular, sublingual, pterygomandibular and the buccal spaces [2]. Severe complications can result if the infection is not recognized and treated promptly and properly. The tendency to underestimate the severity and the extent of the abscess may be because of the multiple cervical fascial layers, the numerous portals of entry of the infection and the proximity of the vital structures [3]. The anatomical structures of the face and neck are included in the spaces which are bound by the fasciae and the understanding of this is essential for the diagnosis and the treatment of infections, because the fascia acts as an effective barrier [4]. Odontogenic infections occasionally spread beyond these barriers [5]. The location of abscesses in patients with such infections is commonly determined by physical examinations alone, but the abscesses of the deep subcutaneous layer can be difficult to locate [6]. In cases of acute odontogenic infections, we need to know whether the inflammatory process is in a stage of abscess formation, which requires primary evacuation of the pus and the administration of antibiotics or whether it is a cellulitis that can be generally treated with antibiotics alone. It is often difficult to diagnose the stage of the infection and to define its exact anatomic location [2].
Odontogenic infections, if they are not properly controlled, can spread to the adjacent head and neck fascial spaces. The spread could be very serious and rapid and it can lead to a critical airway obstruction; therefore, it requires an urgent management in some cases [1]. More serious complications such as life-threatening airway obstructions, mediastinitis, pericarditis, internal jugular vein thrombosis, epidural abscess, and carotid artery erosion have also been reported [7]. Traditionally, the open surgical incision-and-drainage procedure with an appropriate administration of antibiotics has been the mainstay of the treatment. However, an open surgical drainage may potentially carry the risk of inadvertent injuries to the neighbouring vital structures, such as the internal jugular vein, the carotid artery, and the cranial nerves, and subsequently cause devastating complications [8].
Various imaging modalities play an important role in the diagnosis of inflammatory diseases of the head and neck [9]. Plain radiographs, computed tomography (CT) scans, magnetic resonance imaging (MRI) and ultrasonography (USG) are the valuable diagnostic aids [10]. These powerful diagnostic tools have minimized the therapeutic dilemma. Though they are readily available, the plain radiographs pose a problem in yielding soft tissue details. The drawbacks of CT include its high costs, technique sensitivity, unavailability in all health care centres, increased doses of ionizing radiation (2-10 rd/slice), its inability to differentiate the soft tissues of similar radiodensities with vastly different chemical compositions and artifacts from any metallic substances and from motion of the patient [11]. The drawbacks of MRI include its high costs, technique sensitivity, a longer scan time, unavailability of the machines to the average physicians, danger to the magnetic information storage (e.g. Credit cards, tapes), relatively thick sections, and susceptibility to motion artifacts [12]. Thus, the images may suffer from the effects of patient motion. The high static magnetic field also poses a danger to those individuals with cardiac pacemakers, neurostimulator units, and intraocular foreign bodies [13].
Ultrasonography (USG) is a relatively affordable, easily performable, accessible, rapid, inexpensive, and a non-invasive technique [2]. USG is very useful in yielding valuable information regarding the extent, size and the location of intraoral odontogenic infections and infections of the fascial spaces of the maxillofacial area. No echoes are returned by fluids and thus, ultrasonography is very sensitive in detecting fluid collections [2]. It has recently been illustrated that USG is not only of diagnostic value in the management of abscesses in the maxillofacial region, but that it can also can be used therapeutically [14].
This study was conducted to evaluate the efficacy of ultrasonography (USG) in diagnosing the pathological nature, size and the extent of the fascial space infections of odontogenic origin (both superficial and deep) and to compare the results with the clinical evaluation (CE) and the surgical exploration (SE).
METHODOLOGY
A total number of 34 patients (M/F) who were aged between 14-71 years, who reported with odontogenic infections which involved the superficial and the deep fascial spaces of the head and neck, were selected from the Dental OPD, Department of Oral Medicine and Radiology, M. S. Ramaiah Dental College and Hospital, Bangalore, from Nov 2008 to June 2010.
An approval was obtained from the ethical committee of the institution with regards to the study. Informed consents were taken from all the patients after explaining the aim and the methodology of the study to them. A case sheet was formulated to record a detailed patient history, the clinical examination of the swelling and the diagnostic procedures which included conventional radiography and USG and the results were compared with those of the gold standard SE.
The patients with odontogenic infections which involved the superficial and the deep fascial spaces of the head and neck were included in this study. The types of patients who were excluded from the study were patients with toxic symptoms like asphyxia who needed an emergency management, those with pathologies which caused swelling of the face like cysts and tumours of odontogenic origin and patients with bony pathologies such as hyperparathyroidism, Paget’s disease, fibrous dysplasia, etc.
The conventional radiographic examination
A preoperative panoramic radiograph was taken to locate the foci of the infection by using a Panoramic X-ray machine [PLANMECA, made in FINLAND, the exposure parameters were 70 kVp, 10 mA, 18 sec and Kodak T MAT G/RA films (Eastman Kodak Co. New York, NY, USA) with a film size of 6X12 inches in a Kodak X-OMAT cassette with intensifying screens]. The radiographs were processed manually in fresh solutions and they were allowed to air dry. They were viewed and evaluated on a view box under the normal operating illumination. The focus of the infection was assessed by a clinical examination, which was confirmed on a panoramic radiograph.
Ultrasound examination
After the radiographic confirmation, the patients were subjected to US examinations over the suspected area in the transverse and axial directions, to determine the presence or absence of a fluid collection and its anatomic location. The tooth and the suspected area under investigation were subjected to a US examination by using the diagnostic ultrasound machine, Voluson 730 Pro Machine (GE Medical Systems) with colour Doppler (CD), which incorporated a high definition and multifrequency and with an ultrasonic probe (LA-39) which operated at a frequency of 8-11MHz. The ultrasound probe was covered with an ultrasound gel (Ultragel; Medicon, India) which was positioned on the face, against the skin, which corresponded to the involved area, and its position was changed several times to obtain an adequate number of transverse (axial) planes to define the extent of the lesion [Table/Fig-1].
Ultrasound scans in different planes

All the lesions were measured in 3 planes i.e. anteroposterior, superoinferior and mesiodistal and the dimensions were recorded. Colour Doppler was applied to depict the anatomic view of the vessels and to show the mean velocity and the direction of the blood flow in the region of the infection, in the cases which were suspected to have abscesses. All the grayscale ultrasound images were analyzed, and the focal lesions were measured by using onscreen calipers. The ultrasound echogenicities were described in comparison with the adjacent tissues as follows: hyperechoic (brighter), isoechoic (equal), hypoechoic (darker), anechoic (no internal echoes) or mixed. They were the key in staging the infections from the acute phase to a complete abscess formation.
Surgical exploration
The details which were obtained from USG such as the stage and the extent of the lesion were reported to an oral surgeon and the treatment plan was decided accordingly. Cellulitis was medically managed with systemic antibiotics like amoxicillin and clavulanic acid (Tablet Augmentin, 625mg thrice daily for 5 days) and the patients were recalled for review. Most of the patients showed signs of reduced pain and swelling. The patients with space infections were subjected to incision and drainage, with knowledge on the extent and the proximity to the vital structures, which was obtained through USG. All the included cases showed 100% correlation with the USG findings. The data analysis was carried out by using the SPSS software package (SPSS Inc, Chicago, V.10.5, USA). The usefulness of US, SE and CE was evaluated by using the Bayesian method in terms of the true positives (TPs), false positives (FPs), true negatives (TNs) and false negatives (FNs) which were determined. The sensitivity, specificity, positive predictive value and the negative predictive value and the percentage accuracy of the diagnostic techniques were measured.
RESULTS
Clinical examination
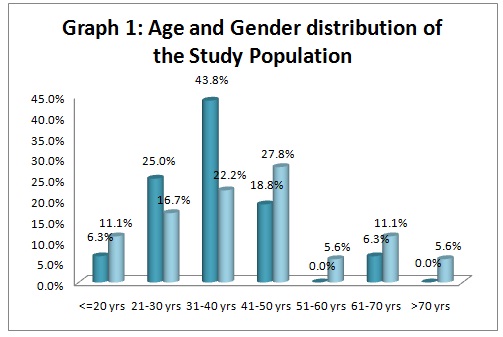
The distribution of the age in the study sample was 34. The median age was found to be 39.12 years, with a range of 14-71 years. The maximum number of individuals who were affected was in the age group of 31-40 years (32.4%), followed by those in the age group of 41-50 years (23.5 %) [Table/Fig-2]. The diagnosis of odontogenic space infections by CE validated that out of the 34 cases, 25 were diagnosed with abscesses (73.5%) and 9 with cellulitis (26.5%) [Table/Fig-3].
Distribution of Study Samples by Age Groups and Gender
| Gender | Age | Total |
|---|
| <=20 yrs | 21-30 yrs | 31-40 yrs | 41-50 yrs | 51-60 yrs | 61-70 yrs | >70 yrs |
|---|
| Male | 1 | 4 | 7 | 3 | 0 | 1 | 0 | 16 |
| 6.3% | 25.0% | 43.8% | 18.8% | .0% | 6.3% | .0% | 100.0% |
| Female | 2 | 3 | 4 | 5 | 1 | 2 | 1 | 18 |
| 11.1% | 16.7% | 22.2% | 27.8% | 5.6% | 11.1% | 5.6% | 100.0% |
| Total | 3 | 7 | 11 | 8 | 1 | 3 | 1 | 34 |
| 8.8% | 20.6% | 32.4% | 23.5% | 2.9% | 8.8% | 2.9% | 100.0% |
Validity of Clinical Diagnosis
| Frequency | Percent |
|---|
| Abscess | 25 | 73.5 |
| Cellulitis | 9 | 26.5 |
| Total | 34 | 100.0 |
Ultrasound examination
Of the 34 cases, 22 were diagnosed with abscesses (64.7%) which showed anechoic areas, which could be solitary or multiple well defined foci of pus. 11 cases with cellulitis (32.4%) showed hyperechoic areas than normal areas, because of a massive inflammatory infiltration into the infected region and 1 case was sialadenitis with an abscess (2.9%). Among these, an isolated submandibular space infection (14.7%) was the highest which was reported among the patients, followed by a buccal space infection (11.8%). There were also involvements of other primary spaces of the maxilla and the mandible. 2 cases were reported to have parotid space involvement (5.9%); 1 with a retropharyngeal abscess (2.9%); 1 with submandibular and parapharyngeal spaces (2.9%) and 1 patient with an extensive involvement of the left buccal, lateral pharyngeal and the anterior mediastinal spaces (2.9%) [Table/Fig-4].
Validity of USG Diagnosis
| Diagnosis Ultrasound | Frequency | Percent |
|---|
| Abscess | 22 | 64.7 |
| Cellulitis | 11 | 32.4 |
| Abscess & Sialadenitis | 1 | 2.9 |
| Total | 34 | 100.0 |
Surgical exploration
When these patients were surgically or medically managed, 23 cases were found to have abscesses (67.6%) and 11 had cellulitis (32.4%) [Table/Fig-5].
Validity of Surgical Diagnosis
| Surgical Diagnosis | Frequency | Percent |
|---|
| Abscess | 23 | 67.6 |
| Cellulitis | 11 | 32.4 |
| Total | 34 | 100.0 |
Summary of the parameters obtained by clinical examination, ultrasound and surgical exploration are explained in a concise cumulative data[Table/Fig-6].
Summary of the parameters obtained by clinical examination, ultrasound and surgical exploration
| Method | Accuracy | Sensitivity | Specificity |
|---|
| Clinical | 67.6% | 0.647 | 0.324 |
| Ultrasound | 97.1% | 1.000 | 0.957 |
| Surgical | 95.7% | 0.986 | 0.936 |
The study showed that the mandibular molars are the most commonly involved and the affected space is tha buccal space [Table/Fig-7].
Accuracy of USG Diagnosis in determining the spaces affected according to the teeth involved
| Teeth Involved | Diagnosis Ultrasound | Total |
|---|
| Abscess | Cellulitis Abscess & Sialadenitis |
|---|
| 15 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| 16 | 2 | 4 | 0 | 6 |
| 33.3% | 66.7% | .0% | 100.0% |
| 17 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| 26 | 1 | 2 | 0 | 3 |
| 33.3% | 66.7% | .0% | 100.0% |
| 28 | 1 | 0 | 1 | 2 |
| 50.0% | .0% | 50.0% | 100.0% |
| 36 | 3 | 0 | 0 | 3 |
| 100.0% | .0% | .0% | 100.0% |
| 37 | 2 | 0 | 0 | 2 |
| 100.0% | .0% | .0% | 100.0% |
| 45 | 0 | 1 | 0 | 1 |
| .0% | 100.0% | .0% | 100.0% |
| 46 | 3 | 2 | 0 | 5 |
| 60.0% | 40.0% | .0% | 100.0% |
| 48 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| 13,14 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| 14,15 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| 16,17 | 1 | 1 | 0 | 2 |
| 50.0% | 50.0% | .0% | 100.0% |
| 35,36 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| 36,37 | 2 | 0 | 0 | 2 |
| 100.0% | .0% | .0% | 100.0% |
| 43,44 | 0 | 1 | 0 | 1 |
| .0% | 100.0% | .0% | 100.0% |
| 47,48 | 1 | 0 | 0 | 1 |
| 100.0% | .0% | .0% | 100.0% |
| Total | 22 | 11 | 1 | 34 |
| 64.7% | 32.4% | 2.9% | 100.0% |
Comparison between the clinical vs the USG diagnosis
Age Distribution of the study population showed that the peak age group affected was 31-40 years which is demonstrated in the [Table/Fig-8].
Age and Gender distribution of the Study Population
Out of the 25 cases which were diagnosed as abscesses clinically, only 18 were found to be abscesses and out of the 9 cases which were diagnosed as cellulitis, only 4 were found to be cellulitis when they were subjected to USG evaluations [Table/Fig-9].
Sensitivity, Specificity, PPV and NPV of Clinical diagnosis vs Ultra sound
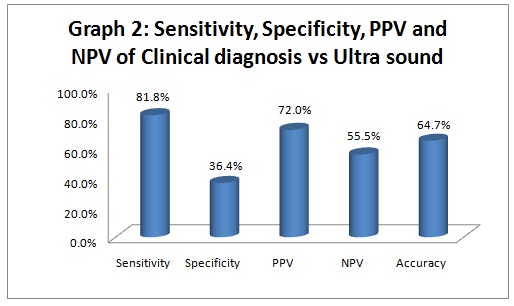
Sensitivity: 81.8%,
Specificity: 36.4%,
Positive Predictive Value: 72.0%,
Negative Predictive Value: 55.5%,
Accuracy: 64.7%
Comparison between the clinical vs the surgical diagnosis
Out of the 25 cases which were diagnosed as abscesses clinically, only 18 were found to be abscesses and out of the 9 cases which were diagnosed as cellulitis, only 4 were found to be cellulitis, 5 cases turned out to be abscesses which required surgical drainage [Table/Fig-10].
Sensitivity, Specificity, PPV and NPV of Clinical diagnosis vs Surgical Diagnosis
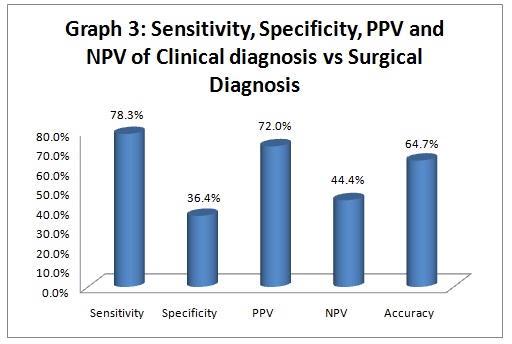
Sensitivity: 78.3%,
Specificity: 36.4%,
Positive Predictive Value: 72.0%,
Negative Predictive Value: 44.4%,
Accuracy: 64.7%
Comparison between the USG vs. the surgical diagnosis
All the 22 cases which were diagnosed as abscesses on the USG examination were also proved to be abscesses when they were surgically explored. Also, all the 11 cases which were diagnosed as cellulitis in USG were diagnosed as cellulitis and they were medically managed [Table/Fig-11].
Sensitivity, Specificity, PPV and NPV of Ultra sound vs Surgical Diagnosis
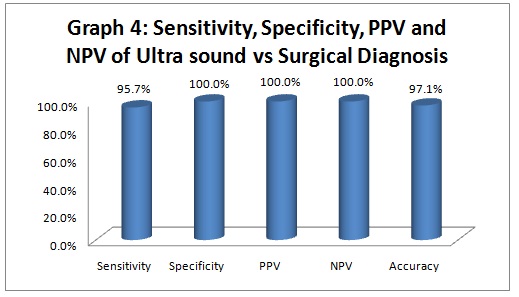
Sensitivity: 95.7%,
Specificity: 100.0%,
Positive Predictive Value: 100.0%,
Negative Predictive Value: 100.0%,
Accuracy: 97.1%
DISCUSSION
Odontogenic space infections, when they are not recognized early, can lead to life threatening situations and even death [15]. The management of oral and maxillofacial infections is a topic that deserves a much more intensive and a high quality research.16 USG can be used for the purpose of diagnosing intraoral odontogenic infections and infections of the superficial and deep fascial spaces of the maxillofacial area [14]. The relatively blind surgical incision and drainage of the abscesses, based on the diagnoses which are made by the physical examination, may result in excessive harm, unnecessarily extensive incisions, excess time, and a failure in locating and evacuating the abscess cavity.
Peleg et al demonstrated the usefulness of ultrasonography as a diagnostic tool for superficial fascial space infections. They had conducted a study on 50 patients with acute odontogenic infections of the superficial fascial spaces, in which a USG evaluation helped in identifying abscesses in 22 patients and cellulitis in 28 patients [2]. In our study, we found that among the 34 patients with both superficial and deep space infections, who were subjected to USG with a colour Doppler evaluation, we could successfully identify abscesses in 22 patients, cellulitis in 11 patients and sialadenitis and a parotid abscess in one patient, which helped us in aiding the surgeon in a better management of these patients. A study was done by Misurya et al., on 25 patients who presented with fascial space infections of the head and neck region. They were evaluated clinically and ultrasonographically and it was concluded that the addition of the ultrasonographic findings to the findings of the clinical examination, increased the sensitivity and the specificity for the detection of abscesses, it increased the diagnostic accuracy and it also helped in a proper treatment planning [16]. In our study, a patient [Table/Fig-12] who was clinically diagnosed as cellulitis, when subjected to a USG evaluation, showed an anechoic focal collection in the infraorbital space. In this above case, if the patient would have just been treated for cellulitis, based on the clinical diagnosis, the abscess would have spread from the infraorbital space to the cavernous sinus, resulting in a life threatening cavernous sinus thrombosis. The USG method could be considered as a quick, widely available, inexpensive, and relatively painless one. It can be repeated as often as necessary without any risk to the patient [17].
A case of infraorbital space abscess. a, Clinical picture showing swelling resembling cellulitis
b, Cropped panoramic radiograph showing involvement of maxillary canine on right side
c, Ultrasound image showing multiple anechogenicities in the infraorbital space confirming the presence of an abscess

Ultrasonography was reported to be a useful tool in detecting abscesses, but it could not differentiate an abscess from the surrounding blood vessels [18]. A combination of colour Doppler USG with a grey scale solved this problem.
In a study which was performed by Yusa et al., USG with colour Doppler which was performed in eight patients, yielded useful information in two cases. They found that in one case, the common carotid artery and the internal jugular vein were close to the abscess and that the facial artery was close to the abscess in the other case [6]. Similarly, in our study, one of the patients [Table/Fig-13] had a submandibular space infection which extended to the lateral pharyngeal space and the anterior mediastinum. By colour Doppler, we were able to find that the left internal jugular vein was involved closely with the abscess and that it was thrombosed, with absolutely no flow through it. Additionally, USG revealed that the submandibular gland and the entire anatomy of the carotid region were distorted, thus advocating the need for an immediate surgical drainage.
A case of lateral pharyngeal space abscess. a, Clinical picture showing a pterygomandibular space abscess
b, Cropped panoramic radiograph showing involvement of mandibular first molar on left side
c, Ultrasound image showing anechoiec collection in the left submandibular space, lateral pharyngeal space extending into the anterior mediastinum
d, Color Doppler showing involvement of the left internal jugular vein with no blood flow

Baurmash, in a study, had evaluated a large parotid abscess with the help of USG and he had found a large hypoechoic, dark area within the parotid gland, which had confirmed the presence of a parotid abscess cavity [19]. Similarly, in our study, ultrasound showed the presence of a large parotid abscess cavity (hypoechoic, dark area) and it gave accurate information about the size of the abscess. Our study clearly demonstrated the usefulness of the USG evaluation in space infections and also its superiority over the clinical diagnosis, while on clinical inspection, it was extremely difficult to stage the infection.
An intraoral USG (IOU) was reported to differentiate a peritonsillar abscess from cellulitis. IOU is a relatively simple and a safe procedure to perform, the learning curve is short, and the patients tolerate the procedure well [20]. In the present study, an intraoral USG was not performed. An intraoral approach could be adopted in the future, to assess the deeper fascial space infections, such as those in the peritonsillar, parapharyngeal and the sublingual spaces [21].
CONCLUSIONS
In the field of Oral and Maxillofacial Radiology, the recent advancements in the imaging modalities are currently the topic of interest. In the process of diagnosing a disease, the oral radiologist should select an imaging modality which not only provides an accurate diagnosis, but which is also affordable and less harmful, in terms of the exposure of ionizing radiations to the patients. An ultrasonographic imaging is considered to be non invasive, there are no ionizing radiations and it is cheap, readily available and repeatable. Based on our results, we conclude that USG is a valuable addition in the diagnosis of odontogenic fascial space infections, in demonstrating the stages of infections and in aiding the surgeons towards a successful management.
Though USG, as a diagnostic tool, has been widely used in the medical field, its application in dentistry has not been sufficiently ventured into. In our routine practice, the importance of USG should be emphasized to all the practitioners. A small, portable USG machine will definitely be affordable in a dental hospital setup, which will aid the oral radiologists in accurately diagnosing various maxillofacial diseases.