INTRODUCTION
Benign fibro—osseous lesions (BFOLS) and giant cell lesions are dimorphic conditions that consist of a fibro-osseous component in common. BFOLS such as Fibrous dysplasia (FD) are developmental tumour like conditions that occur Unilaterally, diagnosed in the second decade of life and are relatively common in the maxillae. Females are less affected than males, with variable radiographic appearances and never crossing the midline. The patients may exhibit a subsequent regrowth of the lesion and this is estimated to be around 25-50%.
CGCG mostly occurs in the younger age group, with a predilection for females, being more common in the mandible and prevalent in the anterior than in the posterior jaws, often crossing the midline and producing an asymptomatic expansion of the cortical plates, with variable radiographic appearances which range from a unilocular to a multilocular radiolucency. It has been suggested to be a reparative than a neoplastic lesion. Its clinical behaviour ranges from an indolent, slow growing, asymptomatic mass to an aggressive lesion that causes pain, root resorption and a tendency to recur after its excision.
With indifferent clinical and radiologic features, the association of BFOLS and CGCG is always a chance of occurrence. The lesions that present as the elements of different pathologies in one lesion are referred to as “hybrid” lesions. Hybrid lesions which consist of CGCG with fibro-osseous lesions are very rare, with only seven maxilla-mandibular cases being reported in the literature, out of which only one case of CGCG in association with FD has been reported till now.
This may also be because of the negligence of the pathologists in diagnosing the cases by considering only one prominent histopathology feature. With uncertain clinical and radiological features, the histopathological examination remains the main stay of the focus in the diagnosis of these types of lesions. We are reporting a hybrid lesion that consisted of a FD with a CGCG. The uncertainty of these types of lesions, their association, and the presence of giant cells raise a lot of doubts about their origin.
CASE REPORT
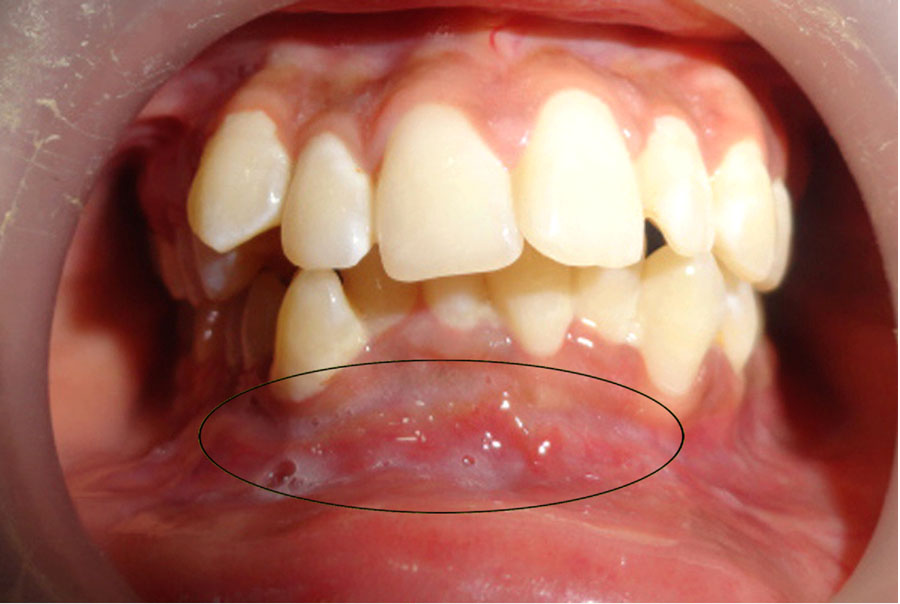
An 18 year old female patient reported to the Dental Out Patients Department (OPD) at Sri Sai College of Dental Surgery, Vikarabad, with a swelling that was insidious in onset, slow growing and non-painful, which involved the right angle of the mandible, with a duration of six months. The intra oral examination revealed a lesion which extended from the distal aspect of the lower left canine to the right first molar, causing obliteration of the vestibule, with a swelling which measured approximately 3*1 cm [Table/Fig-1].
Intra-oral view: The lesion is extending from the lower left mandibular canine to the right mandibular first molar area, crossing the mid-line
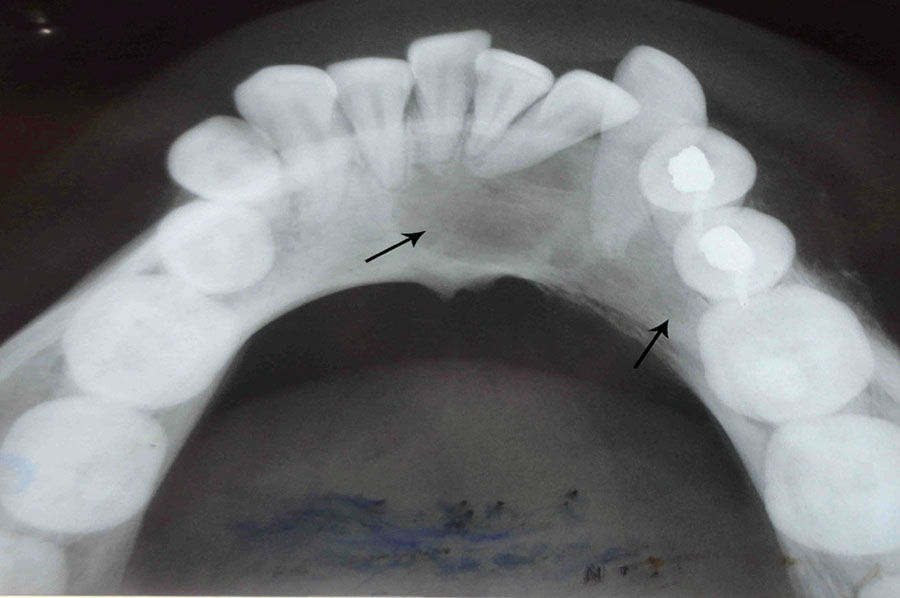
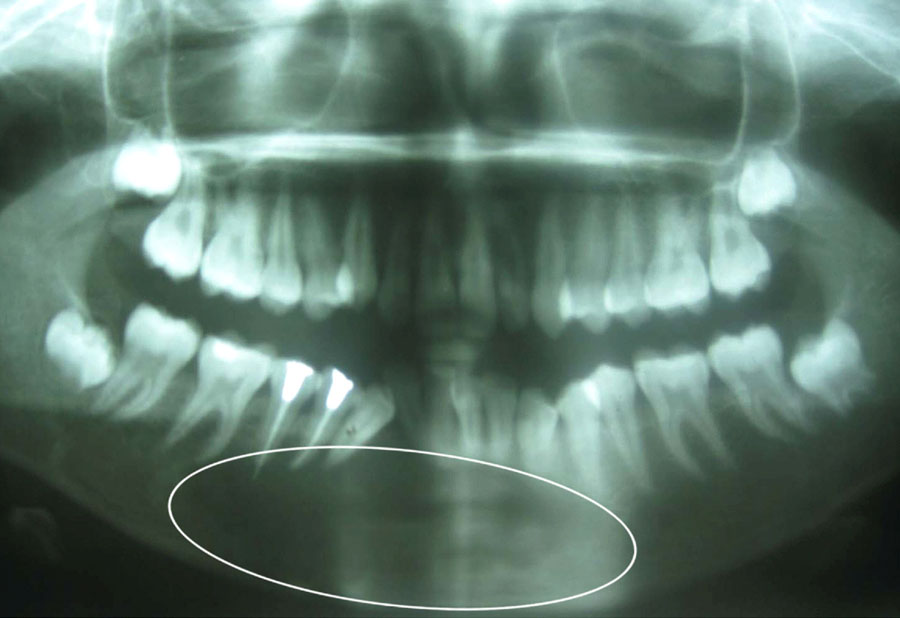
The occlusal radiograph revealed a multilocular radiolucency which extended from the mesial side of left mandibular lateral incisor to the right first molar area, crossing the midline, which was in continuity with the adjacent normal bone [Table/Fig-2]. The orthopantomograph (OPG) revealed a diffuse, multilocular radiolucency which extended anterioposteriorly from the left manibular canine to the right first mandibular molar area, superioinferiorly from the superior border of the mandible to 1 cm below the lower border of the mandible, with root resorption w.r.t to 33-42 and flaring of the roots w.r.t 43-45 [Table/Fig-3].
Occlusal view: Diffuse multilocular radiolucency with periapical resorption areas i.r.t 32, 31 crossing the midline and extending from 41-46
OPG reveals a diffuse, multilocular, radiolucent lesion extending from 34-46, with root resorption and flaring of roots i.r.t 43, 44, and 45
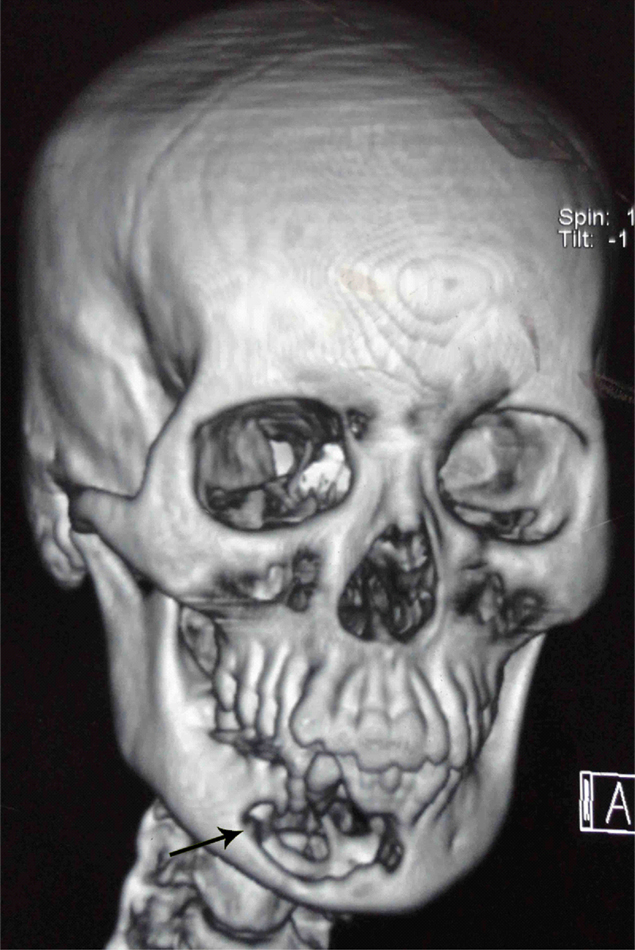
A computed tomography (C.T) scan was carried out and the three-dimensional images showed a well-defined, expansile, destructive, hypodense mass, with thin residual septae like areas [Table/Fig-4]. The routine haemogram and the urine examination were normal.
C.T scan: Three - dimensional CT volume rendering showing the extension of the tumor
On aspiration of the lesion, about 1.5 ml of blood mixed serous fluid was collected and sent for a biochemical analysis, that revealed that the serum calcium phosphatase, alkaline phosphatase (ALP) and the parathormone levels were within the normal range, thereby excluding the possibility of hyperparathyroidism. The protein content of the fluid was 7.9g/dl.
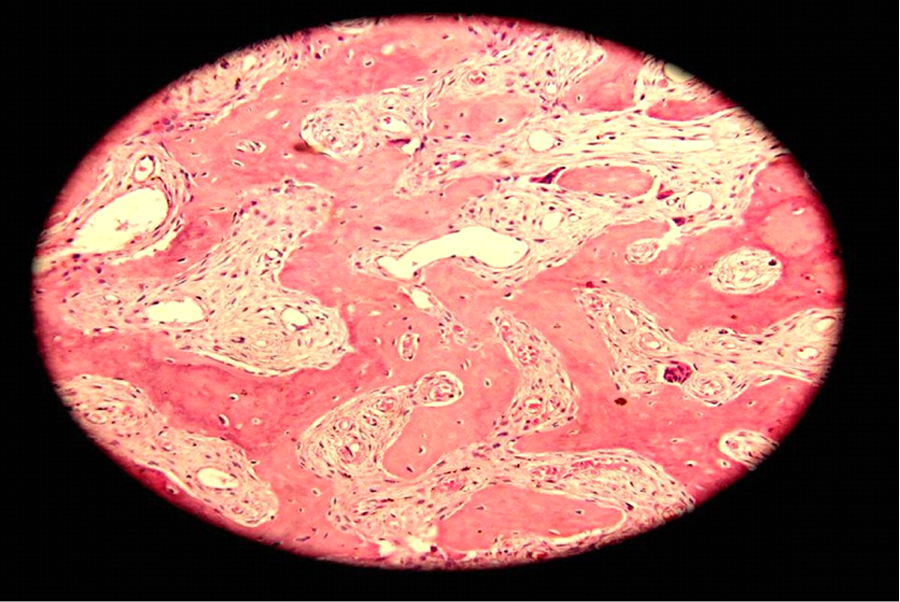
An incisional biopsy was carried out under local anaesthesia, on the buccal side of the lesion, through the thick covering of the bone and a soft tissue specimen was sent for histopathologic analysis. In the gross examination, a tan brown, elliptical tissue which measured 0.5*0.5*1.0 cm, which was hard in consistency, was observed. The microscopic examination revealed irregularly shaped bony trabeculae that were not connected to each other and they had assumed curvilinear shapes (a Chinese letter pattern appearance). These bony trabeculae lacked the osteoblastic border and were arranged in the fibrous stroma with extravasated erythrocytes [Table/Fig-5]. It was reported as Fibrous dysplasia.
Microscopic view of the incisional biopsy specimen showing, interconnecting bony trabeculae that are irregular in shape, lined by osteoblastic rimming at few places and resembling chinese letter pattern. (H&E, 40x)
Based on the histopathological diagnosis, a decision was made to excise the whole lesion and it was sent for a histopathologic examination. The gross specimen consisted of a soft tissue mass which was approx 2*2*1.5 cm in dimension and brown in colour at one end and blackish white at the other end, with irregular borders and it was soft to firm in consistency [Table/Fig-6]. The specimen was sectioned into two and sent for a histopathological analysis. The histopathological examination of the excised specimen revealed abundant giant cells in a fibrous stroma along with vesiculated fibrohistiocytic proliferation. Evenly dispersed giant cells, each having 2 to 8 nuclei in them, which were in close approximation with the proliferating blood vessels, which were admixed with areas of haemorrhage, were observed [Table/Fig-7]. On the high power field (HPF), 2-3 giant cells were seen.
Macroscopic specimen: A soft tissue mass brown to blackish white in color with regular borders, smooth in surface and firm in consistency

Microscopic view of the excisional biopsy specimen showing abundant giant cells in a fibrous stroma along with fibro-histiocytic proliferation (H&E, 40x)
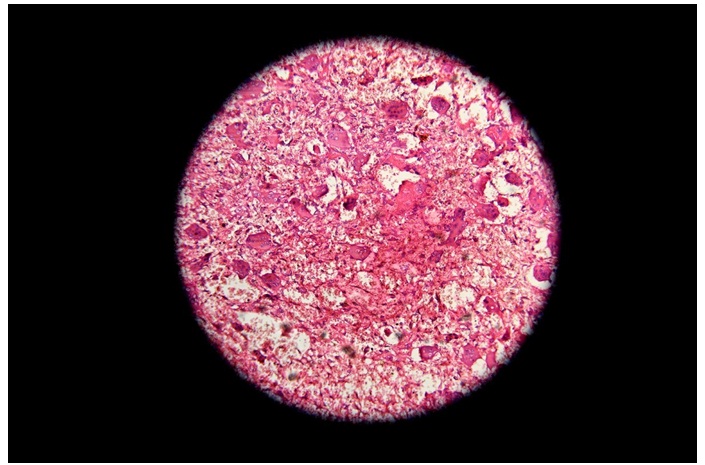
Few newly forming bony trabeculae with a prominent osteoblastic rimming and osteoid formation were also observed. The tumour mass had infiltrating margins and residual bony spicules towards the periphery. The bony trabeculae displayed a curvy pattern without any osteoblastic rimming in few areas of the peripheral lesion. It was reported as a central giant cell granuloma. The histological aspects pointed to a diagnosis of a central giant cell granuloma which was associated with a benign fibro-osseous lesion, a Fibrous dysplasia.
DISCUSSION
Making a differential diagnosis among these BFOLS is very difficult, as these lesions do not present a well defined behaviour. A substantial correlation between the patient history, the clinical features, the imaging findings and the histopathology is necessary. The case which is being reported here, consisted of two different lesions, one, a fibrous dysplasia and the other, a central giant cell granuloma. The concomitant presence of one entity with other lesions, compelled the authors to think about the de-facto existence. Fibrous dysplasia is a rare lesion which occurs in the mandible and it is more common in men [1,2]. The case which is being described here was unique with respect to its location and gender prelidiction. The lesion in our case was observed in the mandible and in a female patient.
Histologically, Fibrous dysplasia shows irregularly shaped bony trabeculae that are not connected to each other. These trabeculae show a Chinese letter pattern appearance . These bony trabeculae lack osteoblastic borders and are arranged in the fibrous stroma along with extravasated erythrocytes and few giant cells. The lesional tissue which fuses with the adjacent uninvolved bone is typical of a fibrous dysplasia.
CGCG is composed of two distinct populations of cells viz. multi nucleated giant cells (MGCs) and spindle shaped stromal cells [2–9]. The latter are thought to be proliferating tumour cells and they form the active cycling compartment. Histologically, in a giant cell containing lesion, haemorrhage occurs with intact areas of frank or partially degenerated RBCs and numerous MGCs and spindle cells are also observed in the stroma, along with mononuclear fibrohistiocytic cells [9,10].
The presence of multi nucleated giant cells (MGCs) that are common to both a FD and a CGCG can help us in understanding the nature of the giant cells. Although the aetiopathogenesis of CGCG of the jaw bones has not yet been established, it was suggested that it could be the result of an exacerbated reparative process which was related to some previous trauma and an intraosseous haemorrhage that had triggered the reactive granulomatous process [11,12]. The association of t(X; 4) (q22; q31.3), was also suggested as an aetiology of CGCG [13].
Although, the nature and the origin of giant cells have been discussed by many authors, the concept of a giant cell origin is still not obscure. One of the proposed hypotheses (I st theory) for the giant cells was a haemorrhage [14]. If the bony matrix of the vessel was weak or defective, it could result in a haemorrhage that could be in the form of intact, fragmented or degenerated red blood cells. This could provide plasma proteins, that could further stimulate the fibroblasts and eventually activate the stromal cells, which in turn could facilitate their conversion into osteoclasts that could give rise to giant cells.
The other hypothesis (II nd theory) was also a hemorrhage, but it could directly provide fresh monocytes from the blood, that could get activated in turn and proliferate into stromal cells. These stromal cells release chemokines such as interleukin-1 (IL-1) and proteases that further cause recruitment of the monocytes and get transformed into osteoclasts, and eventually into giant cells [Table/Fig-8] [14].
Hypothecated mechanism of pathogenesis of giant cell formation
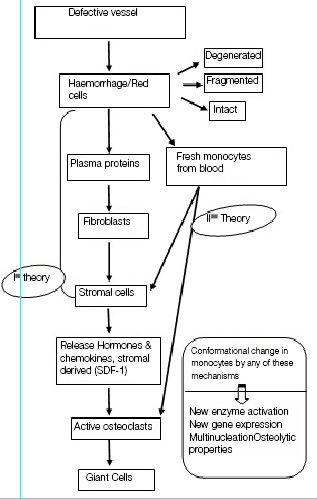
The stromal derived factor (SDF-1) is a significant chemoattractant which is involved in the recruitment of the haematopoietic osteoclast precursor cells (monocytes) during osteoclastogenesis. They also recruit monocytes and induce their differentiation into osteoclastic giant cells through the release of cytokines [15,16]. There may be some conformational changes in the monocytes that can occur because of the activation of new enzymes, the expression of new genes or due to multinucleation or osteolytic properties.
The mononuclear stromal cells may be the precursors of MGCs that may show characteristics of the osteoclast phenotype and a similar kind of pathogenesis may be involved in the formation of MGCs in the other giant cell containing lesions of the jaws.16, 17 They induce osteoclast formation from the mononuclear blood cells via the RANKL-RANKL interaction. The RANKL which is present on the stromal cells influences the differentiation of the giant cells from RANK, that expresses mononuclear cells [17].
It can also be proposed that giant cells can also arise from the stromal elements and react with the epithelial elements, which may behave as foreign bodies [18].
When the giant cell lesions are associated with fibrous dysplasia or other fibro-osseous conditions of the jaws, the association of these giant cells may represent a reaction that may eventually stimulate the necessary stromal changes within the original lesion. This stromal change could involve the osteoblasts, who have the capacity to activate the osteoclasts into giant cells through a paracrine mechanism [10,18,19].
CONCLUSION
Since very few cases have been reported in the literature, the information on the enigmatic association of a FD with a CGCG is obscure. The clinical, radiographic and the histologic features which have been described here, may contribute to the further diagnosis of new cases. The clarity to their adjunctive association, that is very lucid, will now become very obvious, when more cases are reported in future .They may also lead us to understand the interrelationship between them in a better way. By examining and investigating them properly, a definitive diagnosis can be established.
[1]. Alwai F, Benign Fibro-osseous diseases of maxillofacial bones. A review and differential diagnosisAm J Clin Pathol 2002 118 Suppl:S50-70. [Google Scholar]
[2]. Jaffe HL, Giant cell reparative granuloma, traumatic bone cyst and fibrous (fibro-osseous) dysplasia of jaw bonesOral Surg Oral Med Oral Pathol 1953 6(1):159-75. [Google Scholar]
[3]. Waldron CA, Shafer WG, The central giant cell reparative granuloma of the jaws: an analysis of 38 casesAm J Clin Pathol 1966 45(4):437-47. [Google Scholar]
[4]. Whitaker SB, Waldron CA, Central giant cell lesions of the jaws: A clinical, radiologic, and histopathologic studyOral Surg Oral Med Oral Pathol 1993 75(2):199-208. [Google Scholar]
[5]. Kaffe I, Ardekian L, Taicher S, Littner MM, Buchner A, Radiologic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 1996 81(6):720-26. [Google Scholar]
[6]. De Lange J, van den Akker HP, Clinical and radiological features of central giant-cell lesions of the jawOral Surg. Oral Med Oral Pathol Oral Radiol Endod 2005 99(4):464-70. [Google Scholar]
[7]. Kruse-Losler B, Diallo R, Gaertner C, Mischke KL, Joos U, Kleinheinz J, Central giant cell granuloma of the jaws: A clinical, radiologic, and histopathologic study of 26 casesOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101(3):346-54. [Google Scholar]
[8]. Chuong R, Kaban LB, Kozakewich H, Perez-Atayde A, Central giant cell lesions of the jaws: a clinicopathologic studyJ Oral Maxillofac.Surg 1986 44(9):708-13. [Google Scholar]
[9]. Crusoe-Rebello I, Torrens MG, Burgos V, Oliveira C, Santos JN, Azevedo RA, Hybrid lesion: central giant cell granuloma and benign fibro-osseous lesionDentomaxillofac Radiol 2009 38(6):421-25. [Google Scholar]
[10]. Farzaneh AH, Pardis PM, Central giant cell granuloma and fibrous dyplasia occuring in the same jawMed Oral Patol Oral Cir Bucal 2005 (10 suppl 2):E130-132. [Google Scholar]
[11]. Kauzman A, Li SQ, Bradley G, Bells RS, Wunder JS, Kandel R, Central giant cell granuloma of the jaws: assessment of cell cycle proteinsJ Oral Pathol Med 2004 33(3):170-76. [Google Scholar]
[12]. Ustundag E, Iseri M, Keskin G, Muezzinoglu B, Central giant cell granulomaInt J Pediatr Otorhinolaryngol 2002 65(2):143-46. [Google Scholar]
[13]. Buresh CJ, Seemayer TA, Nelson M, Neff JR, Dorfman HD, Bridge J, t(X;4)(q22;q31.3) in giant cell reparative granulomaCancer Genet Cytogenet 1999 115(1):81-91. [Google Scholar]
[14]. Haque AU, Moatasim A, Giant cell tumor of bone: a neoplasm or a reactive condition?Int J Clin Exp Pathol 2008 1(6):489-501. [Google Scholar]
[15]. Liu B, Yu SF, Li TJ, Multinucleated giant cells in various forms of giant cell containing lesions of the jaws express features of osteoclastsJ Oral Pathol Med 2003 32(6):367-75. [Google Scholar]
[16]. Itonaga I, Hussein I, Kudo O, Sabokbar A, Watt-Smith S, Ferguson D, Cellular mechanisms of osteoclast formation and lacunar resorption in giant cell granuloma of the jawJ Oral Pathol Med 2003 32(4):224-31. [Google Scholar]
[17]. Miyamoto N, Higuchi Y, Tajima M, Ito M, Tsurudome M, Nishio M, Spindle-shaped cells derived from giant-cell tumor of bone support differentiation of blood monocytes to osteoclast-like cellsJ Orthop Res 2000 18(4):647-54. [Google Scholar]
[18]. Penfold CN, McCullagh P, Eveson JW, Ramsay A, Giant cell lesions complicating fibro-osseous conditions of jawsInt J Oral Maxillofac Surg 1993 22(3):158-62. [Google Scholar]
[19]. Flanagan AM, Nui B, Tinkler SMB, Horton MA, Williams DM, Chambers TJ, The multinucleate cells in giant cell ganulomas of the jaw are osteoclastsCancer 1988 62(6):1139-45. [Google Scholar]