Misplaced Intrauterine Contraceptive Devices: Common Errors; Uncommon Complications
Vishwas Johri1, Kailash C Vyas2
1 Assistant Professor, Department of Surgery, R.N.T Medical College, Udaipur, Rajasthan 313001, India.
2 Professor Emeritus, Department of Surgery, R.N.T Medical College, Udaipur, Rajasthan 313001, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Vishwas Johri, 8/288, Vidhyadhar Nagar, Jaipur,302039, Rajasthan
Phone: 094601-20556
E-mail: vishwas@gmail.com
Contraception is essential in a developing country like India. Intrauterine Contraceptive Devices (IUCDs) are amongst the most frequently used methods of contraception. The patients with misplaced IUCDs may present with pregnancies or ‘lost strings’ or they may remain asymptomatic.
Misplaced IUCDs, Copper-T in the sigmoid colon, Copper-T in the urinary bladder, An intravesical calculus over an IUCD
INTRODUCTION
Two cases of misplaced IUCDs are being reported, both, because of their unusual presentations and because of their impact on the acceptance of the family planning services.
Case 1 is a result of the transmigration of an IUCD from the uterus to the sigmoid colon, where it was found to be partially buried in its wall. Case 2 is unique, as the transuterine and the transvesical emigration of an IUCD is a rare complication and although it seems technically difficult, since the history of the patient was short and as it was inserted by an ANM , the possibility of an IUCD placement, directly into the urinary bladder, could not be ruled out.
CASE REPORT
Case 1
A 40 years old G2P2A0L2 woman presented to the gynaecology outdoor department with the complaint of menorrhagia, which she attributed to a copper-T which was inserted 15 years ago. She had no other complaints; her per-speculum examination didn’t show any threads of the IUCD. She was advised hysterectomy for the management of her complaints, after which she was referred to us for the management of her lost IUCD.
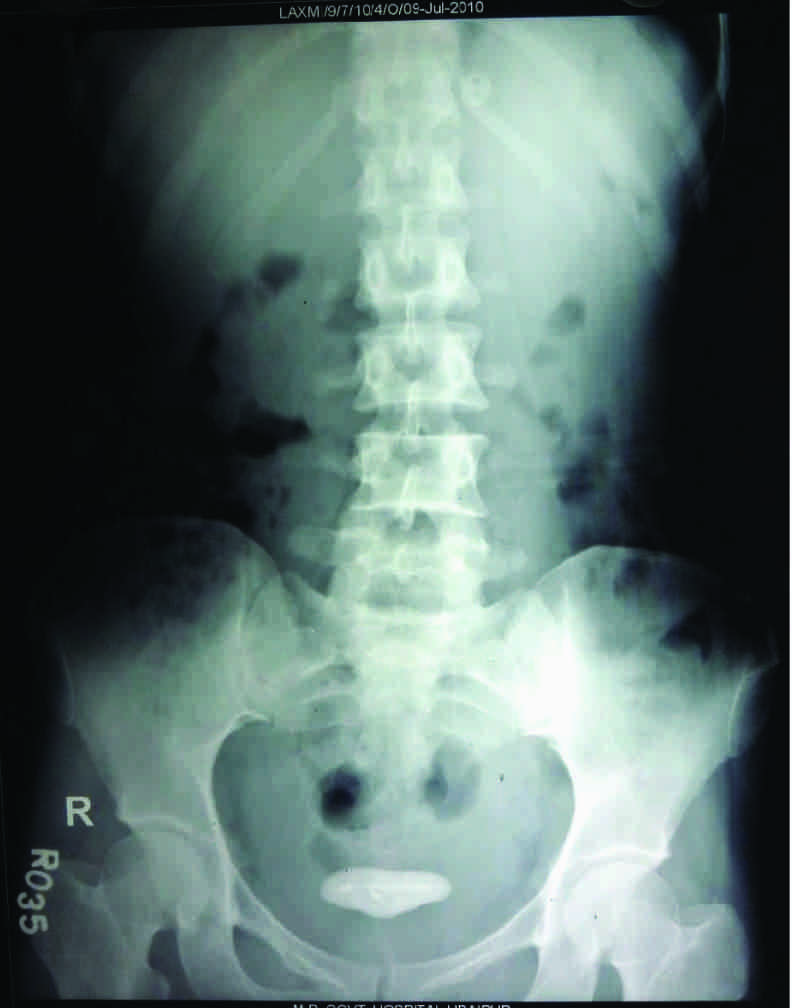
The patient had a soft abdomen, with regular bowel habits. Her per-rectal examination was normal. An X-ray of her abdomen revealed that the copper-T was in the left side of her abdomen [Table/Fig-1a].
X-ray abdomen showing misplaced IUCDI in sigmoid colon

Intra-operatively, the IUCD was found to be partly buried in the proximal sigmoid colon. A primary sigmoidotomy was made around the partly buried limb of the copper-T, through which the remaining copper-T was extracted, which was lying freely in the colon. The sigmoidotomy was closed in two layers. The patient did well postoperatively and was discharged on the 7th postoperative day.
Case 2
A 26 year old G2P2A0L2 woman presented to the gynaecology outdoor department for the removal of her IUCD and for tubal ligation. She gave a history of a copper-T insertion, 7 months back, Vyasat a Primary Health Centre (PHC) by an ANM. Her per speculum examination failed to reveal any threads of the IUCD. She was then referred to us.
The patient had a soft abdomen, with regular bowel habits. She had no other complaints. An X-ray of her abdomen revealed an intravesical calculus, inside which the metallic arms of the copper-T were distinctly visible [Table/Fig-1b]. The diagnosis was confirmed after the cystoscopic visualization of a free floating calculus in the urinary bladder. There were no tell-tale signs which would suggest an intravesical copper-T emigration.
X-ray abdomen showing an intravesical calculus with an IUCD inside it
The calculus was removed through a suprapubic cystolithotomy [Table/Fig-2a and 2b] and the patient was discharged on the 7th postoperative day.
Showing the vesical calculus ACu-T 380A is placed alongside for comparison

Vesical calculus over a Cu-T nucleus ACu-T 380A is placed alongside for comparison

DISCUSSION
IUCDs have been in wide use since 1965 [1]. IUCD migrations from the uterus occur with a reported incidence of 0.5-1%/1000 IUCD insertions [2]. Misplaced IUCDs have been reported from several itneighbouring organs such as the intestinal tract [3] and the urinary bladder, which lead to the formation of vesical calculi [4]. They may lead to perforation of the appendix, thus mimicking appendicitis [5]. They may also be found embedded in the omentum [2]. They may have been mistakenly inserted into the rectum [6] and probably into the urinary bladder, as this case report has suggested.
The mechanism of migration is thought to be the insertion procedure itself or a chronic inflammatory reaction with a gradual erosion through the uterine wall. The incidence is influenced by several factors, which include the timing of the insertion, the parity, a history of previous abortions, the type of IUCD which is inserted, the experience of the operator and the position of the uterus [7]. A delayed onset of symptoms supports a secondary migration [1]. The mechanism of an incorrect placement can only be attributed to an incomplete and faulty training, as well as the reliance of the patients on the untrained or inadequately trained paramedical staff instead of a well trained doctor/gynaecologist.
A plain radiograph of the abdomen is usually the initial examination of choice, for verifying the presence of an IUCD in the pelvis. Once it is found, an ultrasound examination can be done to determine the location of the IUCD which is relative to the uterus. The treatment of the misplaced IUCD is surgical, either laparoscopy or laparotomy. Withdrawal of the migrated IUCD is advisable even if its migration has not given rise to any clinical symptoms [8], so that further complications like a bowel and bladder perforation or a fistula formation may be averted.
CONCLUSION
In India, where the population stood at more than 1.2 Billion at the last count, family planning is the need of the hour. It is therefore essential, that every effort should be made to bring down the failure and the complication rates of the contraceptive measures, so that more couples can be drawn towards these services. An IUCD is a safe method of contraception. The caregivers should ensure that a mere insertion is not the end point of their services. They should also educate the clients about the potential benefits, adverse effects and the complications of the device. A regular self examination for the “missing threads” should be made mandatory.
Proper training of the paramedical staff at the apex centres should be made compulsory, so that they are able to provide safe and better family planning services.
[1]. Zakin D, Stern WZ, Rosenblatt R, Complete and partial uterine perforation and embedding following insertion of intrauterine devicesObstet Gynaecol Surg 1981 36:335-53. [Google Scholar]
[2]. Kriplani Alka, Garg Pradeep, Sharma Meenakshi, Agarwal Nutan, Laparoscopic removal of extrauterine IUCD using fluoroscopy guidance: a case reportJournal of Gynaecologic Surgery 2005 21(1):29-30. [Google Scholar]
[3]. Key TC, Kreutner AK, Gastrointestinal complications of modern intrauterine contraceptive deviceObstet Gynecol 1980 55:239-44. [Google Scholar]
[4]. Singh I, Intravesical cu-T emigration: an atypical and infrequent cause of vesical calculusInt Urol Nephrol 2007 39(2):457-59. [Google Scholar]
[5]. Carson SA, Gatlin A, Mazur M, Appendiceal perforation by copper-7 intrauterine contraceptive deviceAm J Obstet Gynecol Nov 1, 1981 141(5):586-87. [Google Scholar]
[6]. Maru Laxmi, Jharvade Hemlata, Lall Pooja Rani, An unusual case of copper-T in rectumJ Obstet Gynecol India 2005 55(1):79-80. [Google Scholar]
[7]. Heartwell S, Schlesselman S, Risk of uterine perforation among users of intrauterine devicesObstet Gynecol 1983 61:31-36. [Google Scholar]
[8]. Treisser A, Colau JC, Causes, diagnosis and treatment of uterine perforations by intrauterine devicesJ Gynecol Obstet Biol Reprod 1978 7:837-47. [Google Scholar]