Primary fallopian tube carcinoma is an extremely uncommon neoplasm of the female genital tract. Primary Fallopian Tube Carcinoma (PFTC) has a clinical and a histological resemblance to Epithelial Ovarian Cancer (EOC). We are reporting a case of PFTC in a 55 year old tubectomized, postmenopausal woman with the non-specific complaints of a watery vaginal discharge and lower abdominal pain. The clinical and radiological findings suggested a bilateral tubo-ovarian abscess. On laprotomy, a bilateral fallopian tube tumour was seen, with a focal extension to the surface of the right ovary from the right fallopian tube. Total abdominal hysterectomy, bilateral adnexectomy andomentectomy, along with excision of the draining lymph nodes, was done. The histopathological examination revealed a bilateral papillary serous carcinoma of the fallopian tube. The patient was treated with adjuvant chemotherapy with Paclitaxel. There was no evidence of any recurrence, after 2 years of regular follow up. The clinical signs and symptoms of fallopian tube neoplasms are usually non-specific. The primary treatment remains a surgical resection, followed by adjuvant chemotherapy or radiation. The prognosis is poor, although long-term survivors have been reported.
Primary fallopian tube carcinoma, Serous adenocarcinoma
INTRODUCTION
The fallopian tubes are frequently involved in benign gynaecological conditions and are common sites for metastases. Primary malignancies are rare at this site. Primary fallopian tube carcinoma is an uncommon tumour which accounts for approximately 0.14%-1.8% of the female genital malignancies [1]. PFTC has been described in high-risk breast—ovarian cancer families with germ-line BRCA-1 and BRCA-2 mutations [2]. The true incidence of PFTC has been underestimated, because PFTC may have been mistakenly identified as an ovarian tumour due to its histological resemblance to it. A bilateral involvement is still rare. The diagnosis is seldom made pre-operatively, because the signs and symptoms are not specific and are often mistaken for those of a tubo-ovarian abscess or an ovarian tumour [1]. We are reporting an extremely rare case of a bilateral fallopian tube carcinoma in a 55 year old female, with review of the literature.
CASE REPORT
A 55 years old, post menopausal female who was gravid 3, para 2, living child 2 (Parity index - G3P2L2), presented with the complaints of a watery discharge per vagina and a recurrent right lower abdominal pain, of 1 year’s duration. The vaginal discharge was non-foul smelling and watery in consistency. The abdominal pain was a dull ache in the right lower abdomen, which radiated to the back. There was no history of fever and chills. The abdomen examination revealed tenderness in the right iliac fossa and there was no evidence of ascites. The general and other systemic examinations were unremarkable. The per-vaginal examination revealed a retro-verted uterus and the cervix was in line at the level of the introitus. Fullness and tenderness were noted in the right fornices and the left fornices showed motion tenders. The speculum examination was unremarkable. The serological tests for the Human Immunodeficiency Virus and hepatitis were negative. Ultrasonography revealed a bilateral tubo-ovarian solid to cystic lesion, which suggested a bilateral tubo-ovarian abscess. Computed tomography scan of the abdomen revealed an enhanced soft tissue density mass lesion in the right adnexae, with a cystic and an enhancing solid component which measured 5.7 x 3.8cms. The left adnexae also showed a soft tissue density which measured 3.7 x 2.4cms, with a peripheral calcific density [Table/Fig-1], which suggested the possibility of a bilateral tubo — ovarian abscess.
CT Imaging showing soft tissue density mass lesion in the right adnexae with cystic and enhancing solid component measuring 5.7 x 3.8cms. Left adnexae also showed a soft tissue density measuring 3.7x2.4cms with peripheral calcific density

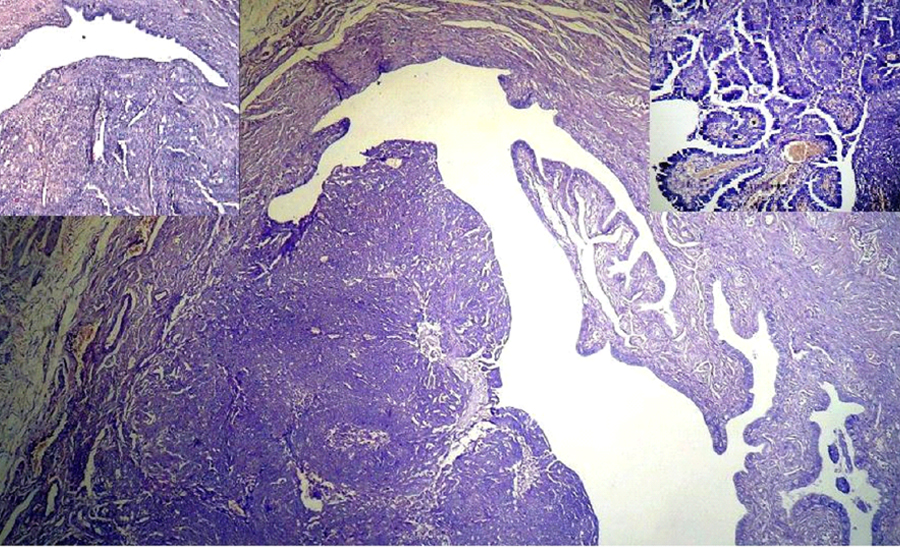
On laprotomy, a bilateral fallopian tube tumour was seen, with a focal extension of the tumour to the surface of the right ovary, from the right fallopian tube (anatomic primary stage IIA). A total abdominal hysterectomy, a bilateral adnexectomy, an omentectomy and excision of the para-aortic lymph nodes were done. The uterus and the cervix appeared to be normal. The right fallopian tube was dilated, with a thickened wall near the fimbrial end and it measured 5.5 x 3.5cms. Its cut surface showed a grey white tumour with serous material, which infiltrated the wall and extended to the surface of atrophied right ovary. The left tube was also dilated and thickened and it measured 3.7x2.4cms. Its cut surface appeared grey white. The left ovary appeared to be atrophic [Table/Fig-2]. Microscopy of the left fallopian tube showed an in situ carcinoma, while the right fallopian tube showed an invasive papillary serous carcinoma, with focal extension into the surface of the right ovary. The tumour cells were pleomorphic, with branching papillae, acini, and a solid pattern, which had vesicular to hyper chromatic nuclei, and increased mitoses [Table/Fig-3]. The left ovary did not show any evidence of the tumour. The endometrium, myometrium, cervix, and the omental adipose tissue were free from the tumour invasion. There was no evidence of any metastatic tumour in the excised lymph nodes. The histological features suggested a papillary serous adenocarcinoma of the bilateral fallopian tube, with a focal extension to the right ovary (Stage IIA- T2a N0 M0 G3). Post operatively, the patient received 6 cycles of adjuvant chemotherapy, Paclitaxel (175mg/m2). There was no evidence of any recurrence of the tumour with regular follow up, after 1 year post chemotherapy.
Gross : Tumor arising from bilateral fallopian tubes, extending to right ovary

Papillary tumor arising from the lumen of left fallopian tubes (H&E X100). Inset: Papillary tumor arising from the lumen of right fallopian tubes (upper right). (Upper left). Higher magnification view showing papillary tumor lined by pleomorphic tumor cells. (H&E X 400)
DISCUSSION
Primary adenocarcinoma of the fallopian tube was first described by Renand in 1897, and it is the rarest malignancy of the female genital tract [3]. Clinically and histologically, it resembles an EOC. PFTC most frequently occurs between the fourth and sixth decades of life, with a median age of 55 years [3]. The aetiology of PFTC is unknown. The frequency and structure of the BRCA mutations had similarities with those which were found in the breast the serous ovarian, and the uterine carcinomas, and consequently, a common molecular pathogenesis was claimed [2]. PFTC is characterized by an extremely unstable phenotype with highly scattered DNA ploidy patterns and frequent p53 gene alterations [4]. The patients with PFTC are usually diagnosed at an earlier stage due to the shorter history of the symptoms and they often present with abdominal pain which is secondary to the tubal distention. Latzko’s triad of symptoms, which consist of an intermittent, profuse, serosanguinous vaginal discharge, a colicky pain which is relieved by the discharge, and abdominal or pelvic masses, has been reported in 15% of the cases [5]. In many cases, the preoperative diagnosis of PFTC is extremely rare. A diagnosis of PFTC may be suspected in cases of postmenopausal bleeding or spotting, with negative findings on colposcopy, cervical biopsy, diagnostic endometrial curettage and abnormal Pap smears [5]. A transvaginal and a transabdominal ultrasound can most often detect the solid and cystic components with papillary projections, and the associated findings like peritumoural ascites, intrauterine fluid collection, and hydrosalpinx. The diagnosis of PFTC is usually first made by a pathologist during a histopathological examination.
The most common histological types of PFTC are serous, endometrioid, mixed, undifferentiated, clear cell , transitional, and mucinous. The serous and the endometrioid types are more commonly seen [6]. The histological differentiation of the tumour as a prognostic factor is unhelpful. The CA-125 antigen is often expressed by PFTC, although CA-125 per se is not diagnostic for PFTC. CA-125 is also a useful early and a sensitive marker for the tumour progression during the follow-up [7]. Primary PFTC can coexist with other tumours. Ayas et al has described the serous type of PFTC with synchronous cervical epidermoid carcinoma in situ [8].
Bilateral PFTC which was associated with uterine leiomyomas was noted by Sarangthem et al., [9].
It is difficult to differentiate PFTC from EOC. The patients should meet at least one of the following criteria for the diagnosis of PFTC [10]. (a) The main tumour is in the tube and it arises from the endosalpinx; (b) Histologically, the pattern reproduces the epithelium of the mucosa and it often shows a papillary pattern; (c) If the wall is involved, the transition between the benign and the malignant epithelium should be demonstrable and (d) The ovaries and the endometrium are either normal or they may contain less tumour than that which is there in the tube. In our case, all the four criteria were fulfilled. In patients who have extensive pelvic tumours, the PFTCs are classified as ovarian in origin, because ovarian cancer is more common than PFTC. PFTCs have a higher rate of retroperitoneal and distant metastases than EOCs have [6]. PFTC spreads by means of a contiguous invasion, a transluminal migration, and a haematogenous dissemination. The PFTCs are richly permeated through the infundibulopelvic lymphatics and they drain into the para-aortic lymph nodes. Considering the strong tendency for a lymphatic spread of the tumour, a systematic pelvic and a para-aortic lymph node sampling is preferred. A lymph node sampling is a mandatory procedure of the surgical staging [11].
The International Federation of Gynecology and Obstetrics (FIGO) EOC staging system has been adapted, to apply to PFTC. Surgery is the treatment of choice for PFTC. The treatment approach is similar to that of ovarian carcinoma, and it includes a total abdominal hysterectomy and a bilateral salpingo-oophorectomy [12]. An aggressive cytoreductive surgery with the removal of as much tumour as possible, is warranted in patients with advanced disease. A postoperative radiotherapy is no longer recommended due to its low efficacy and high rate of serious complications. Based on its propensity for a distant microscopic distant spread and recurrence, chemotherapy seems to have a strong rationale as an adjuvant treatment for the patients with early-stage disease [6].
A single agent chemotherapy does not seem to be effective, while a platinum-based combination chemotherapy is the most commonly used adjuvant therapy, which is similar to that which is used for EOC patients. The reported overall responses rates are 53—92% [6]. The patients with stage IA and IB disease may not require the adjuvant therapy. However, though our patient was in Stage IA, a single drug chemotherapy was given, due to its propensity for a distant microscopic spread. Most of the recurrences are reported in the first 2—3 years [6]. There was no evidence of recurrence in our case, after 1 year of regular follow up. Generally, the reported 5-year survival rate is about 65% or higher [1].
CONCLUSION
PFTC is a rare tumour which accounts for <1% of all the female genital tract cancers. Early clinical manifestations and prompt investigations often lead to the diagnosis of PFTC at an early stage than EOC. Surgery is the treatment of choice, and it should consist of a total abdominal hysterectomy with bilateral salpingooophorectomy, omentectomy, and lymph node dissection from the pelvic and the para-aortic regions. In view of the early lymphatic spread, the role of the routine lymph node removal is mandatory in PFTC. PFTC is similar to EOC in the surgical staging, and management. More extensive clinical research must be performed, in order to have definite aetiologic, diagnostic, and management modalities, and prognostic markers.
[1]. Sedlis A, Carcinoma of the fallopian tubeSurg Clin North Am 1978 58:121-29. [Google Scholar]
[2]. Aziz S, Kuperstein G, Rosen B, Cole D, Nedelcu R, McLaughlin J, A genetic epidemiological study of carcinoma of the fallopian tubeGynecol Oncol 2001 80:341-45. [Google Scholar]
[3]. Nordin AJ, Primary carcinoma of the fallopian tube: a 20-year literature reviewObstet Gynecol Surv 1994 49:349-61. [Google Scholar]
[4]. Lacy MQ, Hartmann LC, Keeney GL, Cha SC, Wieand HS, Podratz KC, c-erbB-2 and p53 expression in fallopian tube carcinomaCancer 1995 75:2891-96. [Google Scholar]
[5]. Ajithkumar TV, Minimole AL, John MM, Ashokkumar OS, Primary fallopian tube carcinomaObstet Gynecol Surv 2005 60:247-52. [Google Scholar]
[6]. Peters WA 3rd, Andersen WA, Hopkins MP, Kumar NB, Morley GW, Prognostic features of carcinoma of the fallopian tubeObstet Gynecol 1988 71:757-62. [Google Scholar]
[7]. Niloff JM, Knapp RC, Schaetzl E, Reynolds C, Bast RC Jr, CA125 antigen levels in obstetric and gynecologic patientsObstet Gynecol 1984 64:703-07. [Google Scholar]
[8]. Ayas S, Karateke A, Aköz I, Kir G, Yenidede I, Primary serous carcinoma of the fallopian tube with synchronous cervical epidermoid carcinoma in situ: a case reportEur J Gynaecol Oncol 2007 28:501-02. [Google Scholar]
[9]. Sarangthem B, Laishram S, Sharma B, Konjegbam R, Debnath K, Primary bilateral tubal adenocarcinoma associated with uterine leiomyomasIndian J Pathol Microbiol 2008 51:32-33. [Google Scholar]
[10]. Hu CY, Taymor ML, Hertig AT, Primary carcinoma of the fallopian tubeAm J Obstet Gynecol 1950 59:58-67. [Google Scholar]
[11]. Gadducci A, Landoni F, Sartori E, Maggino T, Zola P, Gabriele A, Analysis of treatment failures and survival of patients with fallopian tube carcinoma: a cooperation task force (CTF) studyGynecol Oncol 2001 81:150-59. [Google Scholar]
[12]. Klinika ZA, Ginekologiju I, Akuserstvo Klinicki Centar Vojvodine, Novi Sad. Primary fallopian tube carcinomaMed Pregl 2009 62:31-36. [Google Scholar]