Primary Genito-Urinary Tuberculosis with Bilateral Urolithiasis and Renal Failure-An Unusual Case
Sandeep Gupta1, Santhosh R2, Kangjam Sholay Meitei3, Sinam Rajendra Singh4
1 Senior Resident, Post doctoral (Mch) Trainee, Department of Urology, RIMS, Imphal, India.
2 Junior Resident, Post Graduate Trainee, Department of surgery, RIMS, Imphal, India.
3 Senior Resident, Post Doctoral (Mch) Trainee, Department of Urology, RIMS, Imphal, India.
4 Professor & Head, Department of Urology, Regional Institute of Medical Sciences, Lamphelpat, Imphal, Manipur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandeep Gupta, Senior Resident, Department of Urology, RIMS, Imphal-795004, Manipur, India.
Phone: 07308940144
E-mail: drsandeepgupta2009@yahoo.in
Urolithiasis leading to renal failure is a very common occurrence. But if the patient is co-infected with genitourinary tuberculosis, then it becomes all the more unusual and challenging, especially if the patient is immunocompetent. This patient, who presented to us with bilateral urolithiasis and features of renal failure, underwent left nephrectomy after thorough investigations. The biopsy revealed features of renal tuberculosis. The patient was put on anti-tubercular therapy (ATT) and later, he underwent right ureteroscopic lithotripsy. He completed his course of ATT and is on regular follow-up. His serum creatinine also stabilised with regular hemodialysis. The main aim of this case report is to bring to light this unusual and interesting presentation of bilateral urolithiasis with genito-urinary TB presenting as renal failure, which was successfully managed.
Primary Genito-urinary Tuberculosis, Urolithiasis, Renal failure
CASE REPORT
The most common form of nonpulmonary tuberculosis, after lymphadenopathy, is genitourinary disease, which accounts for 27% (range, 14 to 41%) of the nonpulmonary cases [1]. On the other hand, urolithiasis is one of the most common afflictions of modern society. Renal disease which is caused by environmental mycobacteria in non-immunosuppressed individuals is exceedingly rare [2]. It is not uncommon to see a patient of genito-urinary tuberculosis or urolithiasis present with renal failure, but if the patient has both urolithiasis and tuberculosis concomitantly, then it becomes all the more challenging to determine the cause of the renal failure and to manage it successfully. Hence, we would like to bring to light this interesting case that we recently encountered.
A 30 years old male presented to us with the complaints of a decreased urine output and facial puffiness with pedal oedema. He had visited another hospital for the same complaints few months back and he was also admitted there for a few days. He also gave a history of significant weight loss of about 10 kgs in the past 3 months and fever on and off. On checking his previous medical records, it was revealed that he was suffering from left renal calculi and a right upper ureteric calculus, for which an emergency bilateral double-J stenting was done in that hospital, as he had presented with bilateral gross hydronephrosis and a deranged renal function test. He did not give a history of any known co-morbid conditions or of any form of immunodeficiency.
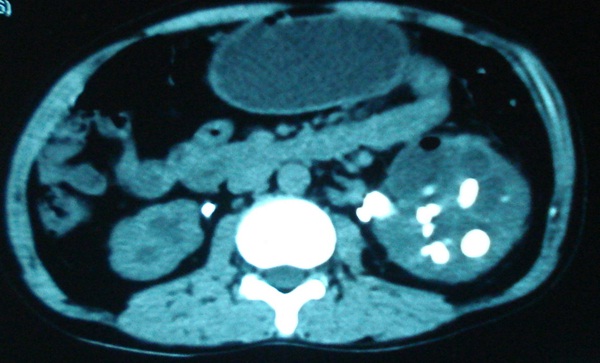
His serum creatinine at the time of presentation to us was 2.6mg% and urea was 64 mg%. A non-contrast CT-scan revealed multiple left renal calculi, a right upper ureteric calculus with bilateral gross hydronephrosis and a bilateral D-J stent in situ [Table/Fig-1]. The left renal parenchyma was thinned out. A urine routine examination revealed sterile pyuria with acidic urine. His chest X-Ray was normal. An ELISA test which was done for HIV was negative. The rest of the investigations did not reveal anything significant.
NCCT scan showing left multiple calculi and right upper ureteric calculus with bilateral hydronephrosis
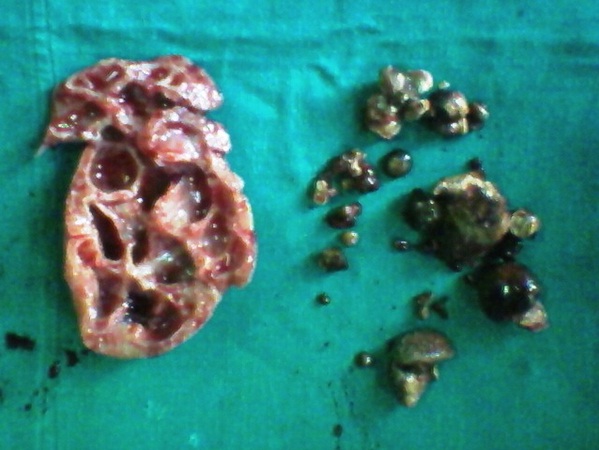
The patient underwent left nephrectomy after a thorough workup, as it was clear that his left kidney was not salvageable. The excised specimen [Table/Fig-2] was sent for a histopathological examination. The biopsy report showed caseating granulomatous pyelonephritis with Langhans giant cells, which were suggestive of renal tuberculosis.
Left nephrectomy specimen with the multiple calculi
A thorough workup was done, to look for any evidence of active tuberculous foci elsewhere in his body, also in his genito-urinary system. His urine was sent for acid fast bacilli (AFB) staining and culture, which showed negative results. Post operatively, his serum creatinine started to rise and he underwent 2 sessions of haemodialysis. After consultation with the other concerned specialities, he was put on anti-tubercular therapy (ATT) for 6 months with a proper dose adjustment.
Two weeks later, he underwent a ureteroscopic lithotripsy for the right ureteric calculus and finally, about one month after being admitted, he was discharged. But by then, chronic renal failure had set in and his nadir serum creatinine had stabilized to around 3mg%. He now has to undergo maintenance haemodialysis regularly. He completed his course of ATT and is symptomatically much better. He is on regular follow-up with our department also.
DISCUSSION
Till date, there are only very few literature reports on cases of bilateral urolithiasis with renal tuberculosis, which finally had led to chronic renal failure. Hence, it becomes all the more challenging to manage such patients and to give them acceptable lifestyles. Also, it is not common for immunocompetent individuals to suffer from genito-urinary tuberculosis. Renal TB should be suspected and treated if the tubercle bacillus is identified microscopically in a urine specimen [3]. However, in Indian studies, the TB culture is positive in only 30-40% of the urine samples [4]. Tuberculosis; although it is an uncommon cause of progressive renal failure, is an important one, because unlike many renal conditions, it is potentially preventable and easily treatable. As per the latest WHO estimate, the prevalence of TB in India is 249/100,000 population/year and among this, 19% are extrapulmonary (WHO 2012 estimates) [5]. Amongst all the GUTB cases, the kidney alone and the kidney with the urinary bladder or the ureter, is affected in more than 70% of the cases [6]. Evidence, as to the extent to which tuberculosis is a cause of end-stage renal failure worldwide, is scanty. But the recent data has suggested that renal TB can cause renal failure in 7.4% of the affected patients [7]. The cause of the renal failure can be either renal parenchymal destruction which is secondary to an infection or which is caused by obstructive uropathy. Obstructive uropathy, again, is an important precipitating factor for renal calculi. Overall, renal or ureteric stones have been reported in up to 19% of the cases [6]. The above mentioned data has been presented by us in a simplified manner in the form of a table [Table/Fig-3].
Statistics of Tuberculosis in India
| TB prevalence in India (2012 WHO estimates) | Extra pulmonary TB | Genito-urinary TB | Renal TB | Association of calculi with renal TB | Association of CRF with renal TB |
|---|
| 249/lac population | 19% of total TB | 27% of extra-pulmonary | 70% of GUTB | 19% | 7.4% |
Whereas, most of the world’s tuberculosis is in the developing countries and the registries of the patients with end-stage renal failure are mainly in the developed world, as are the diagnostic methods, for arriving at a renal diagnosis. For these reasons, there is only little information on the contribution that tuberculosis makes to the burden of renal disease. In 1991, the data which was obtained from the European Dialysis and Transplant Association registry revealed that 195 of 30,064 new patients (0.65%) had renal failure which was caused by renal tuberculosis, an incidence which was similar to those of previous years [8]. It is usually caused by the reactivation of the old, dormant disease, although cases have also occurred in younger, HIV-positive patients [9]. GUTB is extremely uncommon in immunocompetent individuals. In an autopsy study which was done in India, 24 of 35 kidneys from patients who died of AIDS, showed an evidence of infection, which included 17 cases of tuberculosis [10]. In a similar study which was done in Mexico City, renal disease was demonstrable in 87 of 138 (63%) autopsies which were done on AIDS patients: infection was the cause of the renal disease in 36 cases; it was caused by M. tuberculosis in 19 cases [11]. The kidney is usually infected by a haematogenous spread of bacilli from a focus of the infection in the lung. In most of the cases, at the time of presentation, there is no evidence of active pulmonary disease, although there may be a clinical or a radiologic evidence of a past infection, suggesting that a renal involvement occurs as a result of a reactivation after a period of dormancy [12, 13]. Clinically, renal tuberculosis usually presents unilaterally, but post mortem studies which were undertaken in the first half of the 20th century have indicated that the disease is frequently bilateral [14, 15]. On the other hand, it is well known that long standing urolithiasis with obstructive uropathy invariably leads to a renal failure. A prolonged obstruction leads to repeated episodes of pyonephrosis, finally leading to renal failure. But, whether the concomitant presence of both obstructive uropathy and GUTB leads to a more rapid deterioration of the renal functions, is still not established. Neither is there any evidence to prove that one condition can act as a catalyst for the other.
CONCLUSION
Tuberculosis is a common disease worldwide, and so is urolithiasis. They are all the more common in our country. Both have many implications for the urologist as well as for the nephrologist. In developing nations such as ours, sterile acidic pyuria should be thoroughly investigated. Also, an early relief from the obstructive uropathy is the key to the preservation of the renal functions and the prevention of a subsequent need for a haemodialysis, which is still a luxury for a vast majority of the renal failure patients in our country. A team approach is the key to a successful management of such unusual cases.
[1]. Das P, Ahuja A, Gupta SD, Incidence, etiopathogenesis and pathological aspects of genitourinary tuberculosis in India: A journey revisitedIndian J Urol 2008 24:356-61. [Google Scholar]
[2]. Eastwood JB, Dilly SA, Grange JM, Tuberculosis, leprosy and other mycobacterial diseasesIn: Infections of the Kidney and Urinary Tract, edited by Cattell WR 1996 OxfordOxford University Press:291-318. [Google Scholar]
[3]. Takahashi S, Hashimoto K, Miyamoto S, Takeyama K, Takagi Y, Tsukamoto T, Clinical relevance of nucleic acid amplification test for patients with urinary tuberculosis during antituberculosis treatmentJ Infect Chemother 2005 11:300-02. [Google Scholar]
[4]. Ernst JD, Trevejo-Nuez G, Banaiee N, Genomics and the evolution, pathogenesis, and diagnosis of tuberculosisJ Clin Invest 2007 117:1738-45. [Google Scholar]
[5]. World Health Organization. Global tuberculosis control report, 2012. Available from: http://www.who.int/tb/publications/global_report/2012/en/index.html [Google Scholar]
[6]. Eastwood JB, Corbishley CM, Grange J, Tuberculosis and the kidneyJ Am Soc Nephrol 2001 12:1307-14. [Google Scholar]
[7]. Figueiredo AA, Lucon AM, Urogenital tuberculosis: update and review of 8,961 cases from the world literatureRev Urol 2008 10:207-17. [Google Scholar]
[8]. Eastwood JB, Zaidi M, Maxwell JD, Wing AJ, Pazianas M, Tuberculosis as primary renal diagnosis in end-stage uraemiaJ Nephrol 1994 7:290-93. [Google Scholar]
[9]. Dankner WM, Waecker NJ, Essey MA, Moser K, Thompson M, Davis CE, Mycobacterium bovis infections in San Diego: A clinico-epidemiological study of 73 patients and a historical review of a forgotten pathogenMedicine 1993 72:11-37. [Google Scholar]
[10]. Lanjewar DN, Ansari MA, Shetty CR, Maheshwary MB, Jain P, Renal lesions associated with AIDS—An autopsy studyIndian J Pathol Microbiol 1999 42:63-68. [Google Scholar]
[11]. Soriano-Rosas J, Avila-Casado MC, Carrera-Gonzalez E, Chavez-Mercado L, Cruz-Ortiz H, Rojo J, AIDS-associated nephropathy: 5-year retrospective morphologic analysis of 87 casesPathol Res Pract 1998 194:567-70. [Google Scholar]
[12]. Christensen WI, Genitourinary tuberculosis: Review of 102 casesMedicine 1974 53:377-90. [Google Scholar]
[13]. Narayana AS, Overview of renal tuberculosisUrology 1982 19:231-37. [Google Scholar]
[14]. Kretschmer HL, Tuberculosis of the kidney, a critical review based on a series of 221 casesN Engl J Med 1930 202:660-67. [Google Scholar]
[15]. Greenberger ME, Wershub LP, Auerbach O, The incidence of renal tuberculosis in five hundred autopsies for pulmonary and extrapulmonary tuberculosisJAMA 1935 104:726-30. [Google Scholar]