Vivax Malaria Presenting with Myelitis: A Rare Complication
Avijit Moulick1, Somnath Maitra2, Biswasnath Sharma Sarkar3, Anirban Jana4, Sujoy Sarkar5
1 Assistant Professor, Department of Medicine, Calcutta National Medical College, Kolkata, India.
2 RMO-cum-Clinical Tutor, Department of Medicine, Calcutta National Medical College, Kolkata, India.
3 Associate Professor, Department of Medicine, Bankura Sammilani Medical College, West Bengal, India.
4 Senior Resident, Department of Medicine, Calcutta National Medical College, Kolkata, India.
5 Post graduate trainee, Department of Medicine, Calcutta National Medical College, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Avijit Moulick, Assistant Professor, Department of Medicine, Flat F2. 1/14 extn Chittaranjan Colony. City: Kolkata, PIN/Zip, 700032 State: West Bengal. India.
Phone: 91-9943062385
E-mail: dramoulick@gmail.com
Neurological complications may occur with the Plasmodium falciparum infection. However, the association of neurological manifestations with vivax malaria remains doubtful. Of late, there are isolated case reports/studies which have implicated P. vivax in the pathogenesis of severe malaria which is characterized by the features of different organ dysfunctions, which were previously thought to be caused by P. falciparum alone. Though several case studies have mentioned the association of the P. vivax infection with cerebral malaria, a causal correlation has yet to be established. Dorsal cord myelitis (which leads to paraplegia) during the febrile illness, is rarely described in association with vivax malaria, though there are reports on the Post Malaria Neurological Syndrome (PMNS) and acute disseminated encephalomyelitis following vivax malaria. We are reporting a case of P. Vivax malaria which presented with myelitis, which responded well to the antimalarial treatment.
Neurological complication, P. vivax malaria, Dorsal cord myelitis
INTRODUCTION
Neurological manifestations are uncommon in vivax malaria and there are only a few case records on vivax malaria which presents with neurological complications. Although there are a few case reports which have implicated P. vivax as a cause of cerebral malaria, a spinal cord involvement is extremely rare and it has hardly been described in the literature. The only recognized spinal cord dysfunction is a syndrome of Acute Disseminated Encephalomyelitis (ADEM) that develops one to three weeks following malaria and it is considered to be of immune origin. This is more commonly reported with the P. falciparum infection and the symptoms were partially similar to those of infectious meningoencephalitis or even cerebral malaria. An isolated spinal cord pathology without any cerebral dysfunction has rarely been described in the literature. We are reporting on a young male patient who was suffering from vivax malaria, who developed dorsal cord myelitis during the febrile illness, that was not associated with cerebral or any other organ dysfunction.
CASE HISTORY
An 18 years male patient was admitted with high grade fever of 3 days duration, which was associated with chills and rigor and it was relieved with antipyretic intake. It was associated with headache and nausea, but without any weakness, bladder or bowel involvement. There was no history of cough, joint pain or skin rash. He did not have any high risk behaviour or any significant past illness.He developed sudden onset weakness of both the lower limbs on the 5th day of onset of the fever (on the 2nd day of hospitalization). Both the lower limbs were affected simultaneously, without any definite history of a backache. He had sensory impairment below the level of the umbilicus and also, develope durinary retention. The neurodeficit developed over a period of 8-10 hours. Initially, the patient received intravenous fluid, ceftriaxone and paracetamol.
On examination, he was found to be conscious and he had a normal higher mental function and no meningeal sign. The power of both his lower limbs was grade 1/5 (MRC), with a reduced tone and absent deep tendon reflexes. The plantar response was absent bilaterally. An impaired pain and touch sensation was present below the D10 (dorsal 10) dermatome. The position sense and the vibration sense were preserved. The other system examinations were normal.
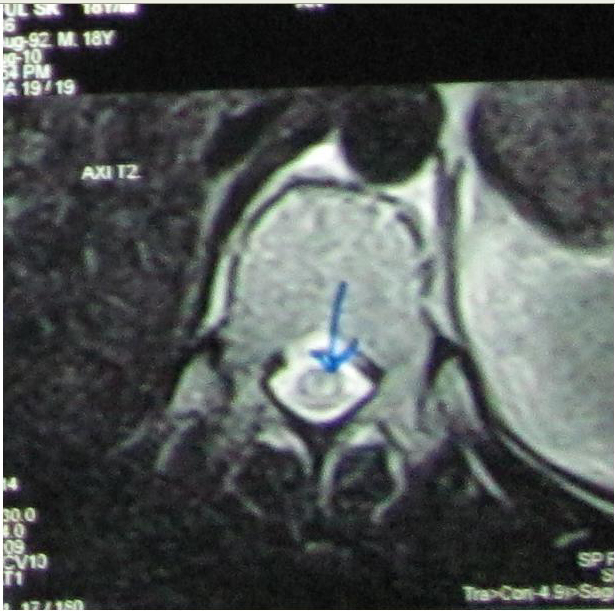
Investigations which were done on the 5th day of the fever revealed Hb%-12.5gm/dl with normal blood counts and ESR, Bilirubin-1.1mg/dl(0.3-1.3), SGOT-28U/L (12-38), SGPT-30U/L (7-41) and alkaline phosphatase-90 u/l(30-102). The fasting blood glucose was 78mg/dl(70-100), serum urea was 24mg/dl (15-40), creatinine was 1.1mg/dl(0.6-1.2) and CPK was132 u/l(50-290). The CSF analysis was normal. Plasmodium vivax trophozoites were detected in the the MP slide test. The rapid diagnostic test for malaria (OptiMAL test, DiaMed AG, Switzerland) was positive for Plasmodium vivax and it was negative for P. falciparum. CT scan of the brain was normal. The blood G-6PD level was 8.2 IU/g Hb(5-13). MRI scans of the dorsal spine which were done on the 6th day of the fever, revealed a linear hyperintense signal in the spinal cord in the T2 weighted sequences, from the D8 to the D11 level [Table/Fig-1 and 2]. The antinuclear factor and ELISA for the HIV I and II antibodies were negative. VDRL was nonreactive. The PA view of the chest X-Ray and the urine RE were normal. An abdominal ultrasound revealed mild splenomegaly. The Salmonella typhi IgM antibody was negative. A provisional diagnosis of myelitis of the dorsal cord, probably of a malarial aetiology, was made. Chloroquine was administered, along with primaquine. The patient became afebrile on the next day. Clinically, the patient’s neurodeficit improved and within 3 days, he started to walk. A repeat testing for malaria (blood smear) which was done on the 10th day, was negative. There was no residual neurological abnormality after the 11th day of the fever onset and during the OPD follow up over the next 12 months.
MRI of dorsal spine done on 6th day of fever revealed, in sagittal images; a linear hyperintense signal in the spinal cord in T2 weighted sequences, from D8 to D11 level

MRI of dorsal spine revealed, in axial images, a hyperintense signal(arrow) in the spinal cord in T2 weighted sequences, from D8 to D11 level
DISCUSSION
The organ dysfunction which is seen in falciparum malaria is ordinarily not seen in the P. vivax infections. If a patient with the P. vivax infection exhibits severe malaria, the infection is likely to be mixed. When patients have a mixed infection, P. vivax may lessen the effect of P. falciparum and cause the disease to become less severe [1].
The neurological complications which occur in the course of the Plasmodium falciparum infections are called cerebral malaria which is characterized by unarousable coma, which results from the diffuse encephalopathy. One to three weeks after the malaria onset (which is more commonly falciparum), an Acute Disseminated Encephalomyelitis (ADEM) has been described, which can mimic the symptoms of cerebral malaria and infectious meningoencephalitis and it is considered to be immune mediated [2].
Neurological complications are very rare in vivax malaria and there has been only a few case reports on vivax malaria which was associated with neurological abnormalities, which excluded PMNS (which has been defined as the acute onset of a neurological or a neuropsychiatric syndrome in a patient who had recently recovered from malaria and had a negative blood film at the time of onset of the neurological symptoms), which also was much more common in severe malaria [3]. In Papua, the P. vivax associated coma was rare; it occurred 23 times less frequently than that which was seen with falciparum malaria, and was associated with a high proportion of non-malarial causes and mixed infections which were detected using PCR [4]. Vest MT et al., reported a 41 years old man who was previously diagnosed with P. vivax malaria, who developed the features of myelitis after a 9-months, symptom free interval. Neuroimaging revealed a T2 hyperintense lesion in the cervical cord, which they considered as an incidental and an unrelated finding [5]. Vivax malaria which presented with psychosis has also been reported [6]. Koibuchi T et al., diagnosed ADEM which followed P. vivax malaria, from the clinical course and the MRI images [7].Kochar DK et al., reported 11 cases of severe P. vivax malaria in Bikaner (western India), which included cerebral malaria (3/11) [8].
There are rare case reports of spinal cord involvement in malaria [Table/Fig-3] and most of them are either falciparum or the mixed infection. Only a single report of vivax malaria with a cord lesion is available in the literature till date. The onset was acute and the recovery from myelitis was complete in most of the cases. Glucocorticoids were used additionally over the antimalarial drugs for most of them.
Clinical features of patients of myelitis of malarial origin
| Sl. No | Title | Age (yr) sex | Onset | Manifestation | Outcome |
|---|
| 1 | ADEM following falciparum malaria caused by VZV reactivation [2]. | 20 M | Acute | Encephalo myelitis like presentation | Responded to antimalarial, meropenem and acyclovir. Recovered after 2 weeks, cephalgia persisted for 6 months |
| 2 | ADEM after mixed malaria infection with MRI closely simulating multiple sclerosis [9]. | Adult female | Acute | Acute onset of bladder retention and paraparesis during recovery | ?Recovery |
| 3 | ADEM after treatment of p. vivax malaria [10]. | 1.5 F | Acute | Fever, loss of consciousness, hemiparesis | Recovered after steroid therapy on 6 months of follow up |
| 4 | ADEM following falciparum malaria [11]. | 20 M | Acute | Headache, paresthesia below nipples, backache, difficulty in holding urine, irrelevant speech | Recovered after 1 week of prednisolone therapy, but paraesthesia recovered after 2 months |
The essential pathologic feature of severe malaria is the sequestration of infected erythrocytes in the deep vascular beds of the vital organs and this occurs only with the P. falciparum infection. The vivax malaria induced neurological complications is a rare entity. Even rarer is the incidence of true myelitis (which is evident from the neuroimaging) which manifests during the presenting illness of the malarial fever. A complete response to the antimalarial drugs (both febrile illness and neurodeficit) suggests the aetiological role of the malaria parasite itself rather than an immunologic phenomenon.
Due to the paucity of laboratory facilities in the peripheral areas of the tropical and the sub tropical regions where malaria is endemic, the evidence regarding the aetiological role of P. vivax in severe malaria is still scanty. Large prospective studies are required to address this issue. Therefore, the clinicians must be prepared to encounter the so called severe malaria in the proven P. vivax infections, as well as to exclude other probable aetiologies.
[1]. Luxemburger C, Ricci F, Raimond D, Bathet S, The epidemiology of severe malaria in an area of low transmission in ThailandTrans R Soc Trop. Med. Hyg 1997 91:256-62. [Google Scholar]
[2]. Lademann M, Gabelin P, Lafrenz M, Acute disseminated encephalomyelitis following plasmodium falciparum malaria caused by varicella zoster virus reactivation:Am. J. Trop. Med. Hyg 2005 72(4):478-84. [Google Scholar]
[3]. Nguyen TH, Day NP, Ly VC, Post-malaria neurological syndromeLancet 1996 348(9032):917-21. [Google Scholar]
[4]. Lampah DA, Yeo TW, Hardianto SO, Coma associated with microscopy- diagnosed plasmodium vivax: a prospective study in Papua, IndonesiaPLoSNegl Trop Dis 2011 5:e1032 [Google Scholar]
[5]. Ozen M, Gungor S, Atambay M, Cerebral malaria owing to Plasmodium vivax: case reportAnn Trop Paediatr Jun 2006 26(2):141-44. [Google Scholar]
[6]. Tilluckdharry CC, Chadee DD, Doon R, A case of vivax malaria presenting with psychosisWest Indian Med J Mar 1996 45(1):39-40. [Google Scholar]
[7]. Koibuchi T, Nakamura T, Miura T, Acute disseminated encephalomyelitis following Plasmodium vivax malariaJ Infect Chemother 2003 9(3):254-56. [Google Scholar]
[8]. Kochar DK, Saxena V, Singh N, Plasmodium vivax malariaEmerg Infect Dis 2005 11:132-34. [Google Scholar]
[9]. Mani S, Mondal SS, Guha G, Acute disseminated encephalomyelitis after mixed malaria infection with MRI closely simulating multiple sclerosisNeurologist 2011 Sep 17(5):276-78. [Google Scholar]
[10]. Goyal JP, Shah VP, Parmar S, Acute disseminated encephalomyelitis after treatment of p. vivax malariaJ Vector Borne Dis Jun 2012 49:119-21. [Google Scholar]
[11]. Suresh V, Srinivas PS, Bhagavati A, Acute disseminated encephalomyelitis following p .falciparum malariaJ Indian Acad Clin Med 2012 13(3):233-35. [Google Scholar]