An injury to the Anterior Cruciate Ligament (ACL) can be devastating; it generally occurs in younger patients and a misdiagnosis, delayed diagnosis, recurrence, injury and an improper surgical technique, may leave a teenage athlete with a knee that is destined to develop premature arthritis [1]. The arthroscopy techniques have been advanced and refined to assist in the reconstruction of anterior and posterior cruciate ligaments [2]. The arthroscopic reconstruction of ACL, is a favoured technical option for restoring the joint stability [3]. Once the decision is made to arthroscopically reconstruct ACL, the various treatment options include a Bone Patellar Tendon Bone graft (BPTB), semitendinosis or semitendinosis with gracilis, a quadriceps tendon and an allograft.
ACL reconstructions with the use of bone patellar tendon bone grafts can be done by single and double incision techniques. The complications which are associated with patellar tendon autografts are their associated harvest site morbidities which include patellar tendinosis, quadriceps weakness, persistent tendon defects, patellar fractures, patellar tendon ruptures, the patello -femoral pain syndrome, patellar entrapments, arthrofibrosis and kneeling pain [4].
The above mentioned complications are seen in both the single and double incision techniques of the bone patellar tendon bone grafts of the ACL reconstructions. One rare complication which is observed following an ACL reconstruction with a BPTB graft is a heterotopic ossification. Few studies, however, have revealed heterotopic bone formations with BPTB grafts [5, 6].
We undertook this study to assess the incidence of heterotopic ossifications in our patients who were treated with BPTB grafts by the double incision technique and the effectiveness of the preventive measures which were taken to decrease the incidence of the heterotopic ossifications. The preventive measures for heterotopic ossifications where copious lavage of the femoral canal following reaming, hemostasis, nibbling of excessive femoral bone plug as seen in study conducted by Ogilvie-Harris DJ, Sekyi-Otu A [7]. We aimed to study the incidence of heterotopic ossifications after reconstructions of ACL with BPTB grafts by the double incision technique and to study the effectiveness of various preventive measures in decreasing this complication.
MATERIAL AND METHODS
We conducted a prospective study in our institution on 285 patients from Jan 2006 to Feb 2012, on whom ACL reconstructions were done with BPTB grafts by the double incision technique and they were assessed for the incidence of heterotopic ossifications at the femoral tunnel sites.
The patients were randomly divided into Group-1 and Group-2. Group-1 included the patients who had received preventive measures which were taken to avoid heterotrophic ossifications, such as copious lavage of the femoral canal following reaming, haemostasis, nibbling of the excessive femoral bone plug were not undertaken. The Group-2 patients had received no preventive measures. The patients who were included in the study were aged between 20-40 years, who had isolated ACLs or associated meniscal injuries, in whom no previous knee surgeries were done and those who presented to us 4-10 weeks following their injuries. The patients with meniscal injuries were included in this study, since it did not affect the outcome of our study, as the treatment of the meniscal injuries is intraarticular and as heterotophic ossifications are extraarticular. The patients who were aged more than 40 years or those who had other ligament injuries, with weights of >90kg and with a history of previous knee surgeries, were excluded from the study.
The operations were done by the same set of surgeons and all the patients had to undergo a similar post operative physiotherapy protocol. As soon as the patients presented to us in the outpatients department, they were assessed clinically and radiographically by X-rays and MRI scans of the knees, along with the assessment for other associated injuries. Once the diagnoses of the isolated ACLs or of those with associated meniscal injuries were confirmed, the patients were put on braces and once the acute inflammatory signs like swelling and pain had subsided, the patients’ knees were put through ROM exercises to restore the complete mobility, which included extension before the operative intervention was undertaken. All the required preoperative blood investigations were done. When the patient fitness was obtained, the patients were electively posted for ACL reconstructions with BPTB grafts by the double incision technique. Preparation of the operative limbs was done just before the patients were shifted to the operation theatre. Intravenous antibiotics (3rd generation cephalosporins) were given just before the patients were shifted to the operation theatre, at the time of anaesthesia.
Intraoperatively, the patient was placed in the supine position, with the lateral port just proximal to the operated knee and a tourniquet was applied around the proximal thigh. With the knee kept in flexion, the BPTB graft was harvested via an incision of almost 6-7cm, which extended from the inferior pole of the patella to the tibial tuberosity. The paratenon was divided longitudinally. A central third BTPB graft was harvested, which was 10mm wide, with a 10mm x 25mm tibial bone block and a 9-10mm x 20mm patellar bone block. The bone block was cut in a triangular fashion at the tibial level, to decrease the bone stress and the anterior knee pain. A no. 2 nylon suture was passed through the hole as a pulling suture.
The tibial bone tendon junction was marked with sterile methylene blue to aid its appropriate placement in the femoral tunnel. The patellar tendon defect was sutured with a no. 3 vicryl suture and the paratenon was closed with a running suture. Through the anteromedial and the anterolateral portals, the knee was visualized. The outflow was through the arthroscopic and no separate cannula was inserted. The articular and the meniscal injuries were addressed first. Any remaining fibres of the torn ACLs were debrided with a motorized shaver.
A 10mm rugine was used to debride the medial wall of the lateral condyle first, near the posterior capsule, to identify the site of insertion of the ACL. An appropriate notch plasty was done. With the knee flexed to 90 degrees, the femoral drill guide was inserted through the anteromedial portal. The tip of the guide was placed immediately behind the foot print of the native ACL. The landmarks for an exact placement was the guide between the notch roof and the lateral notch wall and the superior border of the cartilage of the posterior part of the lateral femoral condyle, at the 11 O’ clock position for the right knee and at the 1 o’clock position for the left knee. The outside of the femoral guide lies over the lateral cortex of the femur. A 2cm longitudinal skin incision was made slightly superior to the lateral epicondyle, which extended through the iliotibial band, up to the bone. The guide pin was drilled from the proximal to the distal in an oblique direction.
An outside-in femoral tunnel (approximately 25 to 35mms) was drilled by using a cannulated reamer; the size of the same was similar to the diameter of the graft. The anterior end of the tunnel was at the isometric point of the ACL insertion of the femur. A 55 degree drill guide was used for the tibial tunnel, through the anteromedial portal. The tip of the drill guide was 7mm anterior to the PCL, on a line which joined the inner edge of the anterior horn of the lateral meniscus and the medial tibial spine. Drilling was done through the anteromedial tibia with a cannulated drill, which was of the same size of the graft after the drill was correctly positioned.
With a suture passer, the graft was passed into the knee by passing a nylon loop suture through the joint. The suture at the end of the graft was passed into the loop suture, so that the surgeon could pull on the loop suture out of the tibial or the femoral tunnel, thus allowing the suture or the graft to go out of the tunnel. The methylene blue marked tendon bone junction was flushed with an intra-articular portion of the tunnel. The BPTB was passed with a cortical surface which was posterior in the femoral tunnel, to keep the tendon portion posterior. The cancellous portion was made to point laterally in the tibial tunnel, to produce a 90 degree fibre rotation of the ACL. A femoral fixation was done by using interference screws, with the knees in 110 degrees of flexion from the upper lateral femoral cortex to the tunnel. The tibial interference screw was fixed with the knee in extension, after pre-tensioning the graft by maintaining traction on the suture, after putting the knee through a cycle of flexion and extension. An intraarticular suction drain was placed. The deeper wound was closed with 3-0 vicryl and the skin was closed with 3-0 nylon. Sterile compression dressings were applied. The knee was immobilized in a long knee brace.
Postoperatively, three doses of IV antibiotics (3rd generation cephalosporins) were given at 12, 24, and 36 hours after the surgery and analgesics for pain were also advised. A post operative physiotherapy protocol was instituted i.e. isometric knee strengthening exercises on the same day of the surgery. The range of motion and partial weight bearing with crutches were started three to four days after the surgery and they were gradually progressed to achieve less than a 5° extension loss and a flexion of 90°, two weeks after the surgery. A knee flexion of more than 90° and full weight bearing mobilization were progressed from two to four weeks after the surgery. Walking without crutches was started after one month. Jogging was started after three months when the patient regained 60% of the knee extension of the opposite knee. Sports activity was started after six months. The patients were assessed clinically and radiologically at 4, 8 and 12 weeks and 3 months, to study the incidence of the heterotophic ossifications post-operatively.
RESULTS
The total number of patients and the incidence of the heterotopic ossifications have been depicted in [Table/Fig-1]. Overall, the incidence of the heterotopic ossifications in our study series was 2.1%, in 285 cases which were studied. The incidence of the heterotopic ossifications was 2.58% in Group-1. The incidence of the heterotopic ossifications was 1.54% in Group-2. The mean duration of the diagnosis was 7.8+/1.2 weeks in Group-1 and it was 8.2+/0.2 weeks in group 2, [Table/Fig-2].
| Group 1 | Group 2 |
|---|
| Age (years) | 31.45±8.5 | 33.19±6.7 |
| Surgical duration (minutes) | 75±21 | 70±16 |
| Weight (kgs) | 55±14 | 52±10 |
| Mean duration of (weeks) | 7.8±1.2 | 8.2±0.2 |
Incidence of heterotropic ossification
| Group | Number of patients | Number of patients with heterotopic ossification | Incidence of heterotopic ossification (%) |
|---|
| Group 1 | 155 | 4 | 2.58 |
| Group 2 | 130 | 2 | 1.54 |
| Total number of patients | 285 | 6 | 2.1 |
We found from our study series, that the incidence of the heterotopic ossifications [Table/Fig-3] was significantly reduced if preventive measures in the form of a copious lavage of the femoral canal with normal saline, following reaming of the tunnel; haemostasis and nibbling of the excessive femoral bone plug, were done.
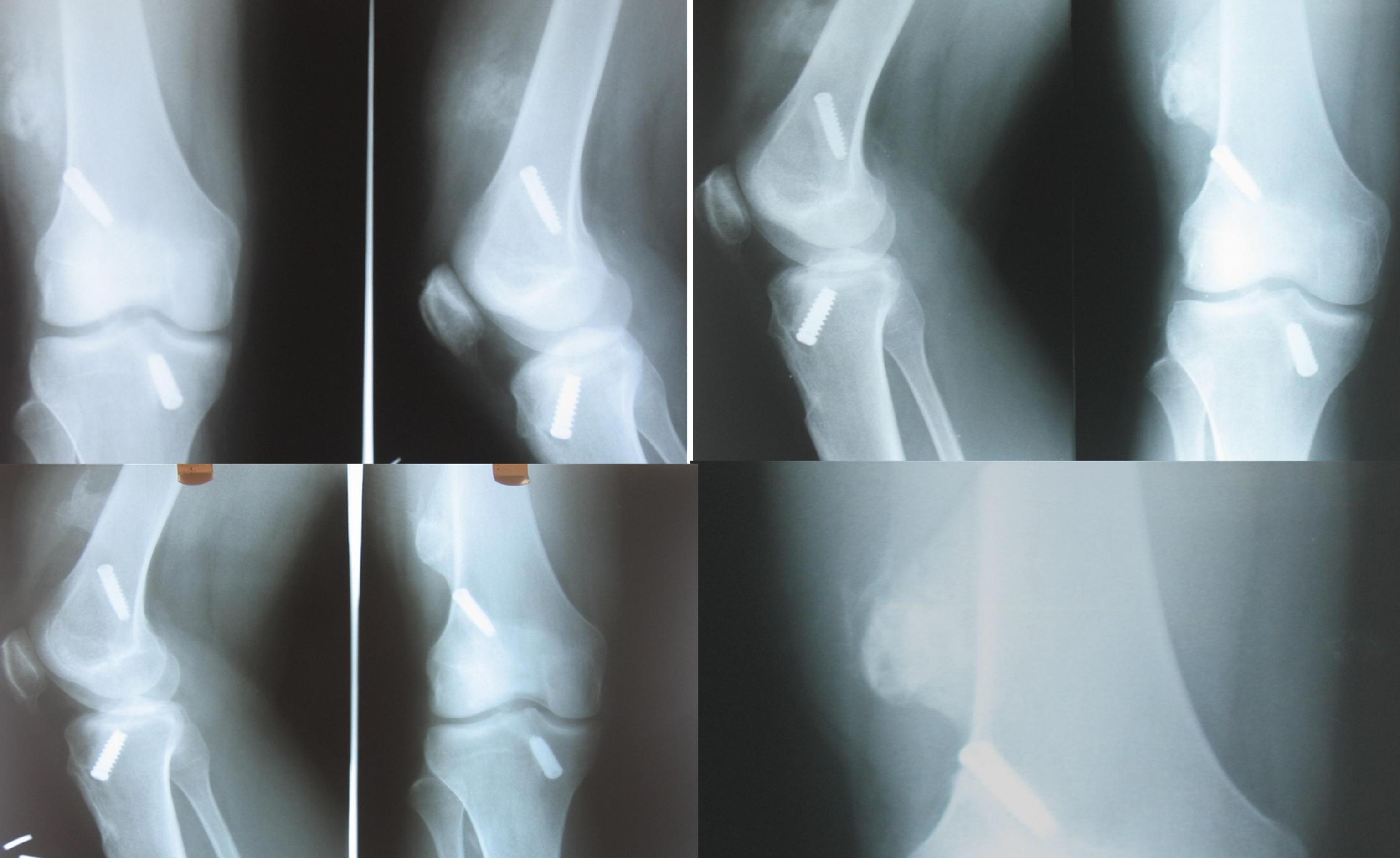
Heterotopic ossification after the ACL repair. Ossified bony mass visualised at lower end of the femur, attached the cortex
DISCUSSION
Currently, BPTB grafts and hamstring tendons are the preferred materials in the surgical management of ACL injuries. Success rates of above 90% have been reported for ACL reconstructions with the use of middle third BPTB grafts [8, 9]. However ACL reconstructions with the use of BPTBs are associated with many problematic outcomes. In the literature, patellar fractures, patellar tendinitis or ruptures, the patellar infra syndrome, patellar sensitivity, a difficulty in sitting on the knees, shortening of the patellar tendon, loss of the terminal extension and patella-femoral pain have been listed as the most common complaints [9–12]. Calcification of the patellar tendon can be seen in some disorders such as jumper’s knee [13] and the Sinding Larsen-Johansson disease [14] or as a sequel of the Osgood Schlatter disease [15, 16]. It may form secondary to a tendinitis or trauma [17]. The most common occurrences of heterotopic ossifications have been seen in the thigh and arm muscles, mainly in the quadriceps femoris, the brachialis and the adductor muscles of the thigh [18, 19]. In the literature, there have been few reported cases of heterotopic ossifications with ligament reconstructions about the knee [20, 21]. In one case, a patient developed a posterolateral capsular heterotopic ossification as a late complication following a PCL reconstruction [20]. In another case, an infrapatellar heterotopic ossification developed following an ACL reconstruction [21], the proposed aetiology being repeated micro trauma, a chronic impingement which caused inflammation, hypertrophy and fibrosis, with the end result of a cartilaginous transformation and an ossification.
Calcification of the patellar tendon as a complication of an ACL surgery has been mentioned in few reports [6, 22]. Lerat et al., [22] observed superior patellar tendon calcification in their cases but none of them where extensive. In their procedure, they filled the tibial and patellar defects with bone debris from the drilling. They did not perform surgical removals in any patients, as all were without pain.
Specchiulli et al., [6] performed 75 ACL reconstructions and some of the patients showed a slight radiographic evidence of intratendinous calcifications at the latest follow up. The most important cause of a heterotopic ossification following a surgical trauma is inadvertently scattered bone debris in the operative working field. Another possible pathogenesis could be an aggressive post-operative rehabilitation which could result in microtears in the tendon, which could lead to bleeding [10, 12].
In our study series, the same procedure and postoperative rehabilitation were performed in all our ACL reconstructions, to rule out the above cause. We think that bone debris with fragments and haematomas can result in progressive bone formations with time, in the bone bed and the tendon.
In our study series, the incidence of the complication of a heterotopic ossification at the femoral tendon site was 2.58% in Group-1 and it was 1.54% in Group-2. Even if this complication is rare, we suggest a meticulous harvesting and preparation of the graft material to avoid unnecessary future surgeries.
Ogilvie-Harris DJ and Sekyi-Otu A, in their study, found an incidence of a heterotophic ossification of less than 1%. The mean duration of their diagnosis was 6 weeks and the incidence reduced significantly after using preventive measures [7]. They advised excision of the mass for a better rehabilitation. In our study, the incidence of heterotophic ossifications was nearly comparable to that in the study of Ogilvie-Harris DJ and Sekyi-Otu A. In our study series, we did not excise the hetrotophic mass, as it did not cause a significant functional impairment.
The purpose of our study was to highlight this rare occurrence of a heterotopic ossification following an ACL reconstruction with a BPTB graft at the femoral tunnel site by the double incision technique.
CONCLUSION
A heterotophic ossification is a rare complication at the femoral tunnel site after an anterior cruciate ligament reconstruction is done with a bone patellar tendon bone graft by the double incision technique. The incidence reduces significantly on using preventing measures like, saline lavage, excess bone nibbling and achieving a thorough haemostasis. Although a heterotopic ossification following an ACL reconstruction with a patellar tendon autograft is a rarely seen complication, it is important because of its ensuing morbidity.