SLE Developing in a Follow-Up Patient of Kikuchi’s Disease: A Rare Disorder
Anupam Patra1, Sujit Kumar Bhattacharya2
1 Post Graduate Trainee, Respiratory Medicine, Nilratan Sircar Medical College, Kolkata, India.
2 Assistant Professor, Respiratory Medicine, Nilratan Sircar Medical College, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Anupam Patra, 2/15 A, Bijoygarh,Jadavpur,Kolkata-700032, West Bengal, India.
Phone: 9836139511
E-mail: dranupam.patra@gmail.com
Kikuchi’s disease or the Kikuchi-Fujimoto Disease (KFD) is a very rare, self-limiting, benign form of histiocytic necrotizing lymphadenitis, which is mostly seen in young females. We are presenting a case of Systemic Lupus Erythematosus (SLE) which occurred after 2 years in a patient of Kikuchi’s disease during a follow-up examination.
Kikuchi’s disease, Systemic Lupus Erythematosus
INTRODUCTION
Kikuchi’s disease, which is also known as Kikuchi-Fujimoto disease (KFD), is a rare, self-limiting, benign form of histiocytic necrotizing lymphadenitis [1, 2]. Kikuchi first described the disease in 1972 in Japan. The cause of the disease is unknown. Viral and autoimmune diseases are sometimes associated with this disease. There are only few case reports on the association of Systemic Lupus Erythematosus (SLE) in a patient of Kikuchi’s disease and SLE mostly develops simultaneously. We are presenting a case of SLE which developed almost 2 years after the diagnosis of Kikuchi’s disease.
CASE REPORT
A 30 years old female presented to our department with multiple swellings in the neck, along with fever and polyarthritis of 3 week’s duration. She had no history of loss of the body weight, photosensitivity and skin rashes. There was no past history of tuberculosis or of any contact with tuberculosis patients.
On examination, she was found to be conscious, febrile and non toxic. She had multiple, tender, enlarged, bilateral, cervical lymph nodes of varying sizes, the larger ones being about 3cm×4 cm on the left side. There were no skin rashes or generalized lymphadenopathy. Her blood pressure was 110/76 mm of Hg and her pulse rate was 96/min. The examinations of her other systems were within normal limits. Her skin and throat examinations revealed no abnormalities. The routine blood examinations like haemoglobin 12 gm%, WBC count -8400/cmm, ESR-28mm/1st hour, blood glucose, urea, creatinine, sodium, potassium and LFT were normal. Her blood and urine cultures were negative. The sputum for Acid Fast Bacilli (AFB) and the Mantoux test were also negative. Her chest X- Ray and ultrasonography of her abdomen did not reveal any abnormalities. The sera for the antinuclear antibody (ANA) and the anti-ds DNA antibody were negative. The blood for HIV was also negative.
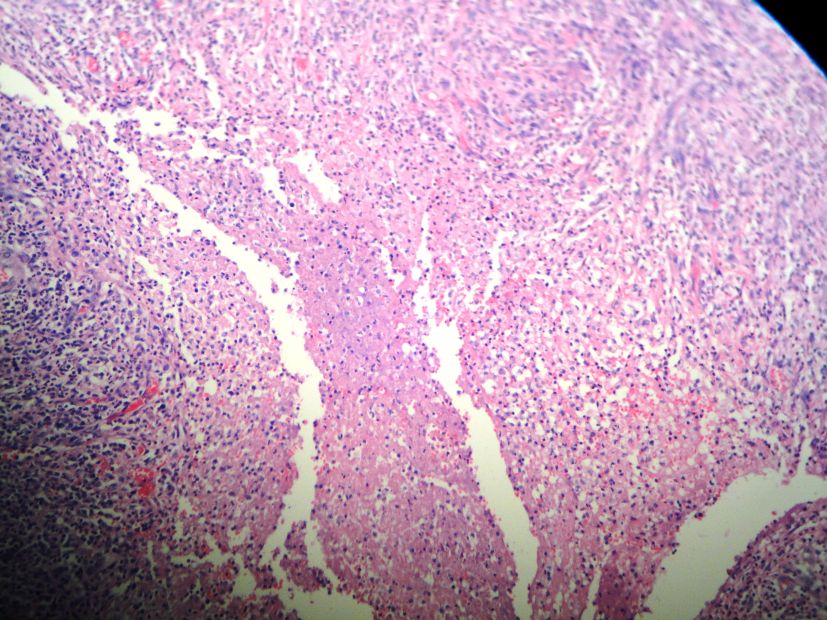
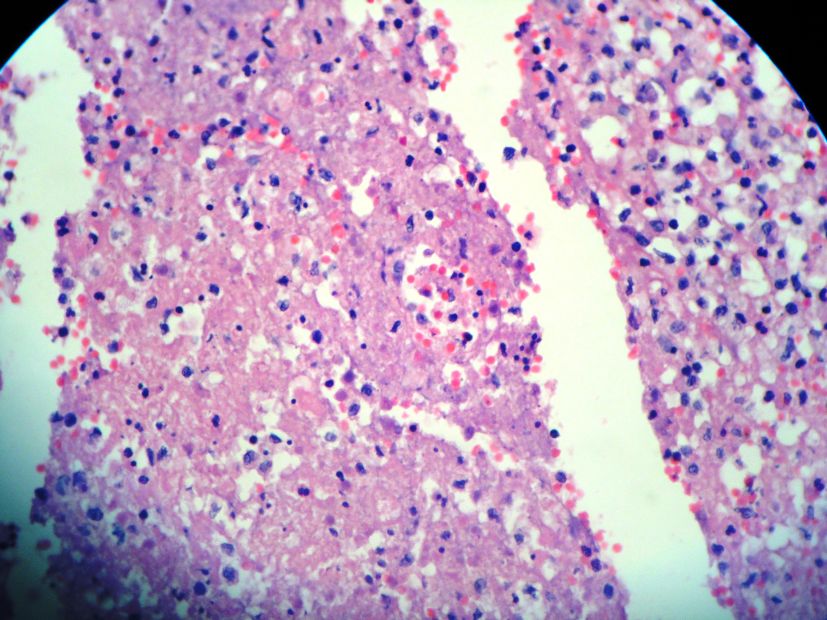
Fine Needle Aspiration Cytology (FNAC) of the left posterior cervical node showed features which were suggestive of reactive lymphadenitis and the patient was put on oral antibiotics. But in spite of one week’s treatment with antibiotics, the patient did not improve clinically and we planned for a lymph node biopsy. The histological features showed well-defined focal paracortical Bhattacharyanecrosis with a zonal histiocytic proliferation. The lymphocytes which surrounded the karyorrhectic debris and the neutrophils were conspicuously absent [Table/Fig-1 & 2]. The staining for AFB was negative. So, on the basis of the biopsy findings, a diagnosis of the Kikuchi-Fujimoto disease was considered. The patient improved clinically with nonsteroidal anti-inflammatory drugs and the lymph nodes regressed in 2 months.
Cervial lymph node biopsy section showing patchy areas of paracortical necrosis, proliferation of histiocytes, increase number of apoptotic cells, cellular debris and nuclear dust (karyorrhexis) (H&E, x100)
Lymph node biopsy section showing prominence of apoptotic cells, cellular debris and nuclear dust (karyorrhexis) (H&E, x200)
After almost 2 years of follow up, the patient again came to us with malar rash, along with inflammatory polyarthritis and fever. At that time, her immunological profile was consistent with SLE [ANA positive 1:640 (Hep2), anti-dsDNA antibody positive, and hypocomplementaemia (C3- 0.55 g/l, C4- 0.19 g/l)]. She was commenced on immunosuppression and low-dose aspirin. She remains in clinical remission.
DISCUSSION
Kikuchi and Fujimoto independently first reported the Kikuchi-Fujimoto disease or histiocytic necrotising lymphadenitis in Japan in 1972. It is considered as a self-limiting benign lymphadenitis, which especially involves the cervical nodes, which is of an unknown cause [3].
The exact aetiology of Kikuchi’s disease is not known. Viral agents such as the Epstein Barr virus (EBV), the Human immunodeficiency Virus (HIV), the Herpes simplex virus, the Dengue virus, the Human T lymphotrophic virus 1 (HTLV1) and the Parvovirus B19 have been suggested as the possible aetiological agents, but none have been confirmed so far. Toxoplasma and other bacterial agents like Yersinia enterocolitica, Bartonella and Brucella have also been implemented [4].
An autoimmune mechanism has also been proposed, because KFD is seen in conjunction with systemic lupus erythematosus (SLE). In reviews, many have described the association of KFD, which is diagnosed concomitantly with or following the diagnosis of SLE [5–7]. Here, SLE developed during a follow up examination of KFD, 2 years after the diagnosis. Clinically, Kikuchi’s disease may mimic Systemic Lupus Erythematosus (SLE) or lymphoma (especially T cell non- Hodgkin’s lymphoma). Kikuchi’s syndrome shares a sex and age predisposition as well as histologic features with Systemic Lupus Erythematosus (SLE). The tubuloreticular structures in the lymphocytes and the endothelial cells in patients with SLE have been observed to be similar to those which are seen in Kikuchi’s disease. One ultrastructural study proposed that Kikuchi’s syndrome reflects a self-limited, SLE-like autoimmune condition which is caused by virus-infected transformed lymphocytes [8]. In reviews, some patients who were initially diagnosed with Kikuchi’s disease were reported to have subsequently developed systemic lupus erythematosus, and an ANA test should be performed in patients with suspected Kikuchi’s syndrome in order to exclude this diagnosis [9,10]. Examination of the lymph node histopathology, in correlation with the clinical features, helps in differentiating SLE from KFD. KFD is characterized by cortical and paracortical necrotizing nodules, apoptotic debris, proliferation of histiocytes and immunoblasts, abundant CD8+ T cells, and an absence/paucity of neutrophils [8, 11].
When KFD is recognized, the possibility of other diseases which include SLE, should always be considered simultaneously or subsequently within months or even after years. So, all the patients of KFD should receive periodical clinical and serological follow-ups for several years to detect a possible evolution of SLE.
[1]. Kikuchi M, Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes: a clinicopathological studyActa Hematol Jpn 1972 35:379-80. [Google Scholar]
[2]. Fujimoto Y, Kozima Y, Yamaguchi K, Cervical subacute necrotizing lymphadenitis: a new clinicopathologic entityNaika 1972 20:920-27. [Google Scholar]
[3]. Kato A, Kono T, Ishii M, Wakasa K, Taniguchi S, Spontaneous clearance of psoriasis during the course of Kikuchi-Fujimoto diseaseJ Am Acad Dermatol 2002 47:S287-88. [Google Scholar]
[4]. Sousa Ade A, Soares JM, de Sa Santos MH, Martins MP, Salles JM, Kikuchi-Fujimoto disease: three case reportsSao Paulo Med J 2010 128(4):232-35. [Google Scholar]
[5]. Meyer O, Kahn MF, Grossin M, Parvovirus B19 infection can induce histiocytic necrotizing lymphadenitis (Kikuchi’s disease) associated with systemic lupus erythematosusLupus 1991 1:37-41. [Google Scholar]
[6]. Tumiati B, Bellelli A, Portioli I Prandi, Kikuchi’s disease in systemic lupus erythematosus: an independent or dependent event?Clin Rheumatol 1991 10:90-93. [Google Scholar]
[7]. Louis N, Hanley M, Davidson NM, Kikuchi-Fujimoto disease: a report of two cases and an overviewThe Journal of Laryngology Otology 1994 108:1001-04. [Google Scholar]
[8]. Imamura M, Ueno H, Matsuura A, An ultrastructural study of subacute necrotizing lymphadenitisAm J Pathol 1982 107:292 [Google Scholar]
[9]. Dorfman RF, Berry GJ, Kikuchi’s histiocytic necrotizing lymphadenitis: an analysis of 108 cases with emphasis on differential diagnosisSemin Diagn Pathol 1988 5:329 [Google Scholar]
[10]. Asano S, Akaike Y, Jinnouchi H, Necrotizing lymphadenitis: a review of clinicopathological, immunohistochemical and ultrastructural studiesHematol Oncol 1990 8:251 [Google Scholar]
[11]. Ramahi KM, Karrar A, Ali MA, Kikuchi disease and its association with systemic lupus erythematosusLupus 1994 3:409-11. [Google Scholar]