Melioidosis with a Pericardial Effusion, which Relapsed as a Chest Wall Abscess: A Rare Presentation
Rashmi Teresa Mathai K.1, K. Sundara Bhat2, Mohammed Ashraf3, Mayank Sarawag4, Kumar K.P.5
1 Senior Resident, Father Muller Medical College, Kankanady, Mangalore-575002, Karnataka, India.
2 Professor, Father Muller Medical College, Kankanady, Mangalore-575002, Karnataka, India.
3 Associate Professor, Father Muller Medical College, Kankanady, Mangalore-575002, Karnataka, India.
4 Assistant Professor, Father Muller Medical College, Kankanady, Mangalore-575002, Karnataka, India.
5 Postgraduate student, Father Muller Medical College, Kankanady, Mangalore-575002, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rashmi Teresa Mathai K., Senior Resident, Department of General Medicine Father Muller Medical College Kankanady, Mangalore Karnataka-575002, India.
Phone: +919663050783
E-mail: drrashmimathai@gmail.com
Melioidosis, which is caused by a soil saprophyte, Burkholderia pseudomallei, is most prevalent in the south–west coast of India. Although it is frequently seen in immunocompromised patients, melioidosis can occur in apparently normal individuals. Melioidosis can involve almost any organ. A relapse of melioidosis is usually associated with a poor adherence to the eradication therapy, a multifocal involvement and bacteraemia. A relapsing melioidosis is usually known to follow a similar pattern of organ involvement in the first and second episodes of the infection. We are discussing here, a rare case of melioidosis in a 38-year-old construction-worker, with no risk factors, who presented initially with a pericardial effusion. It relapsed 6 months after he completed the prescribed eradication therapy for 3 months, as an anterior chest wall abscess. The author recommends a high index of suspicion for the relapsed melioidosis cases, inspite of the primary episode being non-bacteraemic and compliant with the recommended therapy, in order to avoid further complications.
Melioidosis, Relapse, Pericardial effusion, Chest wall abscess
INTRODUCTION
Melioidosis is a community-acquired infection which is widely endemic in south-east Asia and northern Australia, especially during the rainy seasons. Burkholderia pseudomallei, the aetiologic agent of human melioidosis, a widely distributed soil saprophyte, is transmitted by a percutaneous inoculation during an exposure to wet season soil. The patients with diabetes, renal insufficiency, alcoholism and chronic steroid use are the well-recognized predisposing factors [1]. However, 16% of the patients with melioidosis have no identifiable risk-factors [2]. The clinical manifestations are extremely wide ranging and, pneumonia, skin and soft tissue infection hepatosplenic abscesses and septic arthritis occur secondary to a bacterial dissemination. The sputum or abscess pus of the patients with suspected melioidosis should undergo gram staining, which may reveal gram negative bacilli with a bipolar staining and the characteristic ‘safety pin’ appearance. Culture is the mainstay of the diagnosis, with Ashdown’s medium (which contains gentamicin or colistin), which allows the selective growth of B. pseudomallei. The most important complication for the patients who survive the primary episode of melioidosis is recurrence. The pattern of the organ involvement in the primary episode and relapse are usually similar, due to the presence of a quiescent nidus of the infection and granuloma formation of the organism [3]. However, our case proved contrary to this well-accepted theory. We believe that this may be the first reported case of a relapsed melioidosis which presented at a site which was different from that of the primary episode.
CASE REPORT
A 38-years-old construction worker from Mangalore, Karnataka, was diagnosed with a Burkholderia pseudomallei pericardial effusion, 10 months earlier and he was treated with a 2-week intensive course of intravenous ceftazidime in the hospital, followed by eradication therapy with doxycycline and cotrimoxazole for 3 months.
The patient was compliant with the prescribed drug regimen and he was asymptomatic for 6 months. He presented now with a 2-3 week painful swelling on the anterior chest wall. There were no associated symptoms of fever, cough, expectoration or weight loss. The patient gave no history of diabetes, renal disease, chronic lung disease or excessive alcohol consumption. He had normal vital signs. A subcutaneous swelling of 2x2 cm was noted over the anterior chest wall, near the right third costochondral junction [Table/Fig-1]. The swelling was soft and fluctuant and it was not associated with tenderness, warmth or redness. The systemic examination was unremarkable. Clinically, a diagnosis of a cold abscess was made. Chest ultrasonography revealed a well defined collection which measured 2.7 x 2.2 cm, on the anterior aspect of the right third costochondral junction, which was limited to the chest wall.
chest wall abscess near the right 3rd costochondral junction

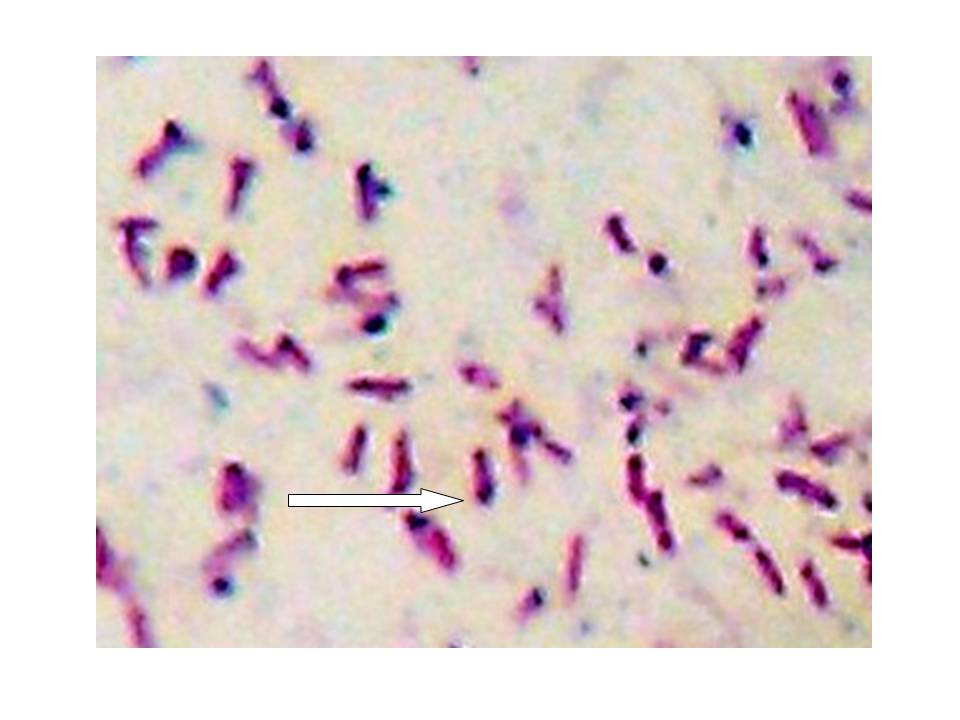
Pus was aspirated from the abscess and it was analyzed by gram staining, culture sensitivity and Acid-Fast Bacilli (AFB) staining. Gram staining showed gram-negative bacilli with the typical bipolar staining ‘safety pin appearance’ and a moderate number of pus cells [Table/Fig-2]. The AFB staining was negative. The culture of the aspirate grew Burkholderia pseudomallei after 72 hours of incubation. The routine blood investigations were within normal limits and the blood culture was sterile after 72 hours of incubation. The patient was thus diagnosed to have relapsed meliodosis, which presented as a chest wall abscess.
Grams stain showing gram negative bacilli with ‘safety pin’ apperance
Oral doxycycline (100mg twice a day), trimethoprim-sulphamethoxazole (320/1600 mg twice a day) and folic acid (5mg/day) were prescribed for 3 months. He was advised to come for a regular monthly follow-up.
DISCUSSION
The studies on recurrent melioidosis have shown it to be either a relapse or a reinfection. The clinical risk factors like the duration and compliance of the therapy, the initial intravenous antibiotics and the severity of the infection, play a role in determining the chances of a recurrence [4]. A multifocal infection, bacteraemia and disseminated melioidosis during the primary episode, are the documented risk factors for a relapse [5]. The recrudescence of the original infecting isolate is assumed to cause a relapse. A relapse may clinically be defined as a new presentation with an acute culture-confirmed melioidosis, after the resolution of the symptoms and the completion of at least the intensive intravenous phase of the antibiotic therapy for the initial meliodosis presentation [6]. A relapse is identified by the same genotype in paired isolates, whereas a re-infection involves a new strain. Practically, making this distinction is difficult, as a majority of the medical centres in India do not have the facilities for genotyping. As per a simple scoring system which was devised by Limmathurotsakul et al., a relapse was found to be associated with a previous inadequate treatment and a shorter time to the clinical features of the recurrence. They also concluded that the site of relapse was usually the same as that of the primary episode and that such cases were associated with 4% antibiotic resistance rates; however, the recommended treatment remains the same. A reinfection was associated with a higher incidence of renal insufficiency and presentation during the rainy seasons [7]. There are reports which have suggested higher relapse rates with drug-regimens which use amoxicillin-clavulanic acid, fluoroquinolones or the doxycycline monotherapy [8,9].In contrast, our patient, had a pericardial effusion in the primary episode, where Burkholderia pseudomallei was isolated only from the pericardial fluid, and not from blood. The pericardial effusion in melioidosis has also been reported in pneumonia which is secondary to a haematogenous spread of the bacterium to the lung or following an inhalation [10]. However, our patient did not have pneumonia as well, in the primary episode. Also, he was treated with a 2-week intravenous course of ceftazidime and a 12-weeks eradication course of doxycycline and cotrimoxazole [11], as per the recommendations. Whether the current episode was a relapse or a re-infection with a new strain, is difficult to say, as genotyping facilities were not available. However, as per the clinical scoring system, our patient was defined as a relapsed case. Though the initial episode of melioidosis presented as a pericardial effusion without bacteraemia, it relapsed as a subcutaneous chest wall abscess, which was contrary to the findings of Limmathurotsakul [7].
Melioidosis which presents as a skin and soft-tissue abscess in the first episode, has been reported to relapse with a similar presentation. This is because B. pseudomallei is presumed to form a quiescent nidus of the infection and granulomas in various organs after an apparent cure, and a persistence at the initial site(s) has been reported [12]. We believe that our case may be the first reported one, where, melioidosis with a pericardial effusion had relapsed as an anterior chest wall abscess. Innate and acquired host factors may be crucial in deciding the organ involvement. Also, there may be a higher chance of bacterial seeding in the already damaged tissues. Thus, a variety of factors may play a role in determining the site of relapse.
CONCLUSION
Though there is a paucity of information on the geographical distribution and the incidence of melioidosis in Karnataka, India, there has been a sudden explosion of cases of melioidosis in relatively normal young patients. Melioidosis, being termed as the ‘great mimicker’, the clinicians should have a high index of suspicion to accurately diagnose it, as well as to provide an early appropriate antibiotic treatment to prevent the single most important complication – a relapse. Patient education and motivation should be given paramount importance, as a relapse is usually associated with a poor adherence and inadequate treatment. Adopting this strategy will play a major role in decreasing the emergence of resistant strains of the organism and hence, the incidence of primary as well as recurrent infections of melioidosis.
CONSENT
An informed consent was obtained from the patient for the publication of this case report.
[1]. How SH, Liam CK, Melioidosis. A potentially life threatening infectionMed J Malaysia 2006 61:386-94. [Google Scholar]
[2]. Currie BJ, Fisher DA, Howard DM, Burrow JN, Selvanayagam S, Snelling PL, The epidemiology of melioidosis in Australia and Papua New GuineaActa Trop 2000 74:121-27. [Google Scholar]
[3]. Limmathurotsakul D, Chaowagul W, Day NP, Peacock SJ, Patterns of organ involvement in recurrent melioidosisAm J Trop Med Hyg 2009 81:335-37. [Google Scholar]
[4]. Chaowagul W, Suputtamongkol Y, Dance DA, Rajchanuvong A, Pattara-arechachai J, White NJ, Relapse in melioidosis: incidence and risk factorsJ Infect Dis 1993 168:1181-85. [Google Scholar]
[5]. Limmathurotsakul D, Chaowagul W, Chierakul W, Stepniewska K, Maharjan B, Wuthiekanun V, Risk factors for recurrent melioidosis in northeast ThailandClin Infect Dis 2006 43:979-86. [Google Scholar]
[6]. Currie BJ, Fischer DA, Anstey NM, Jacups SP, Melioidosis: Acute and chronic diseaseTrans R Soc Trop Med Hyg 2000 94:301-04. [Google Scholar]
[7]. Limmathurotsakul D, Chaowagul W, Chantratita N, Wuthiekanun V, Biaklang M, Tumapa S, A simple scoring system to differentiate between relapse and reinfection in patients with recurrent melioidosisPLoS Negl Trop Dis 2008 2:e327 [Google Scholar]
[8]. Chaowagul W, Simpson AJ, Suputtamongkol Y, Smith MD, Angus BJ, White NJ, A comparison of chloramphenicol, trimethoprimsulfamethoxazole, and doxycycline with doxycycline alone as maintenance therapy for melioidosisClin Infect Dis 1999 29:375-80. [Google Scholar]
[9]. Chetchotisakd P, Chaowagul W, Mootsikapun P, Budhsarawong D, Thinkamrop B, Maintenance therapy of melioidosis with ciprofloxacin plus azithromycin compared with cotrimoxazole plus doxycyclineAm J Trop Med Hyg 2001 64:24-27. [Google Scholar]
[10]. Schultze D, Müller B, Bruderer T, Dollenmaier G, Riehm JM, Boggian K, A traveler presenting with severe melioidosis complicated by a pericardial effusion: a case reportBMC Infect Dis 2012 12:242 [Google Scholar]
[11]. Cheng AC, McBryde ES, Wuthiekanun V, Chierakul W, Amornchai P, Day NP, Dosing regimens of cotrimoxazole (trimethoprimsulfamethoxazole) for melioidosisAntimicrob Agents Chemother 2009 53:4193-99. [Google Scholar]
[12]. Wong KT, Puthucheary SD, Vadivelu J, The histopathology of human melioidosisHistopathology 1995 26:51-55. [Google Scholar]