A spontaneous, intramural, intestinal haematoma is a rare complication of the anticoagulant therapy. We are reporting here, a rare case of a 63-years-old male, who presented with intestinal obstruction which was caused by an intramural and a submucosal colonic haematoma, which had resulted from warfarin administration. This patient rapidly improved after taking conservative treatment. A history of anticoagulant use with a prolonged INR value in patients who present with abdominal pain, should alert the physicians or surgeons to search for this entity. It is extremely important to recognize this syndrome at its early stages, to avoid an unnecessary operation, since the outcome is usually excellent after a conservative treatment.
Intramural haematoma, Anticoagulant, Warfarin, Colon
INTRODUCTION
A partial or a complete bowel obstruction which is secondary to an intramural haematoma is a relatively unusual condition [1–3]. Various aetiologies such as blunt trauma, anticoagulant therapy, Henoch-Schonlein purpura, blood dyscrasias or a complication of diagnostic or therapeutic endoscopies, have been described in the medical literature [2–6]. An intramural haematoma of the intestines, which arises as a result of a prolonged use of anticoagulants, is rather uncommon [5–7]. The literature review has suggested that the duodenum and the small intestine are the common locations for the Anti-Coagulant Induced Haematomas (AIH), while the involvement of the colon and the rectum is rare [4–7]. We are reporting a rare case of a sub-acute colonic obstruction which was caused by an intramural and a submucosal haematoma in the colon, which was secondary to the warfarin anti-coagulant therapy.
CASE REPORT
A 63-year-old male presented to the casualty with a painful abdominal distension and vomiting and bleeding per rectum, of two days duration. He had a progressive abdominal distension over the preceding one-week period, with a history of blood in the stools (haematochesia) since 2 days. The vomiting was bilious and it contained partially digested food material. There was no history of obstipation and melaena. Three weeks ago, he was diagnosed with rheumatic heart disease with mitral stenosis and mitral regurgitation and had been on treatment with warfarin 4 mg, torsemide 10 mg and diltiazam 60 mg.
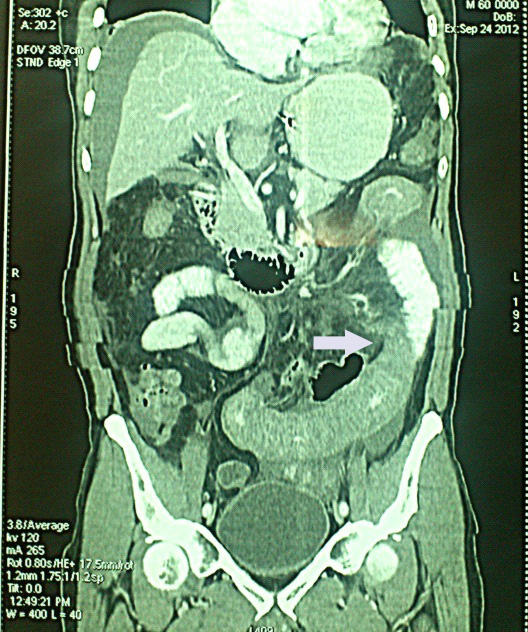
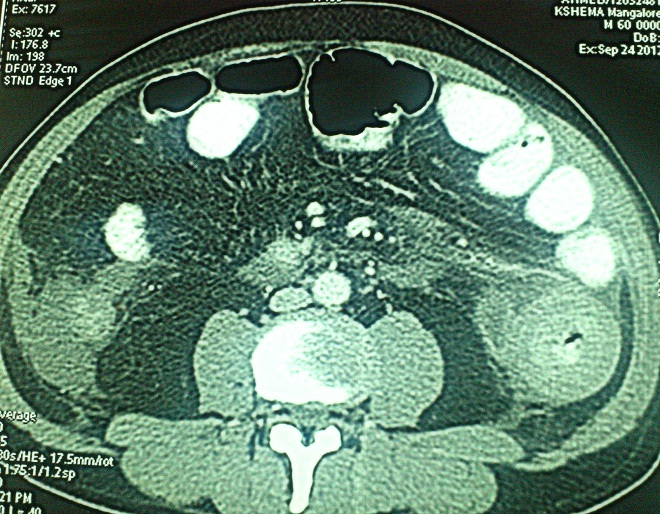
On admission, his vital signs were found to be stable. His per abdomen examination showed a mild to moderate distension with tenderness in the left lower abdomen. Bowel sounds were absent. The complete haemogram and the biochemical parameters were within normal limits. The prothrombin time [PT] was increased (patient - 3 minutes, control-14 seconds). The Activated Partial Thromboplastin Time [APTT] was normal. A plain abdominal X- ray showed a distended large bowel loop, which was compatible with the clinical ileus. Ultrasound of the abdomen showed a long segment bowel wall thickening, with minimal free fluid in the pelvis and the abdomen. Computerized tomography of the abdomen showed a circumferential long segment smooth wall thickening in the sigmoid colon and the rectum. [Tabbe/Fig-1 and 2]- shown in arrows) Colonoscopy which was done on the same day, showed a multiple submucosal haematoma in the rectosigmoid segment [Table/Fig-3].
Computerised Tomography of abdomen showed circumferential long segment smooth wall thickening seen in the sigmoid colon and rectum(Coronal section, shown with arrow)
Computerised Tomography of abdomen showed circumferential long segment smooth wall thickening seen in the colon. (Axial section, shown with arrows)
Colonoscopy showing multiple submucosal haematoma in the rectosigmoid segment

He was treated conservatively with bowel rest, a nasogastric tube drainage, intravenous fluid hydration, and a prophylactic antibiotic therapy. Warfarin was stopped and he was monitored continuously, along with Vitamin K injections, every day for five days. The repeat PT was-15.2 seconds (control-13.9 seconds). The intestinal obstruction was completely resolved. After 2 months of follow up, the patient was free from the bowel symptoms and he was restarted on the warfarin therapy (2mg).
DISCUSSION
Oral anticoagulants are widely used in many conditions such as deep vein thrombosis, persistent atrial fibrillation, etc. The most serious complication which is associated with the use of warfarin is bleeding due to excess anticoagulation, which occurs in about 7.6% of the patients [1,4–6]. However, a spontaneous, intramural/submucosal, intestinal haematoma is uncommon. Small bowel haematomas have been reported as one case per 2,500 anticoagulated patients per year, but intramural colonic haematomas have been described less in the literature [4–7].
The development of a spontaneous AIH has been reported as early as 10 days after the initiation of the anticoagulation therapy [5–7]. The spontaneous, intramural, large-bowel haematomas are expected to occur more commonly with the heparin therapy. Most of the patients present with spontaneous, intramural, small-bowel haematomas after having their symptoms for several days [4,6,7].
A successful treatment of AIH needs cessation of the anticoagulant therapy in the first instance, and an attempt to correct the patient’s coagulation parameters with the administration of fresh-frozen plasma and vitamin K [5–7] The coagulation parameters of AIH are mostly well corrected within 72 hours of taking this therapy. Making a precise diagnosis of AIH before doing an exploratory laparotomy is often quite difficult and it requires a high index of clinical suspicion [4–6]. A barium enema shows the “picketfence” sign and the “coiled-spring” sign. Abdominal CT also reveals similar signs, but these signs are not specific for the cases of intramural haematomas [6]. The haemorrhage is usually located in the submucosal layer of the bowel and it originates from a small vessel that produces a slow bleeding [6,7]. The triad of the warfarin toxicity, a circumferential bowel wall thickening and an intestinal obstruction are characteristic of the spontaneous intramural haematomas [4,6].
In our study, the diagnosis was evident from the CT scan and colonoscopy. The diagnosis of spontaneous, intramural, large-bowel haematomas is determined from the CT findings of the large-bowel wall thickenings and obstruction in patients who had received excessive anticoagulation and who had presented with abdominal pain. Imaging studies which were done in the past, have documented healing of the intestine within 2 months [2,3,6]. In our study, a resolution was noted on colonoscopy, as early as 1 week after the therapy. A prompt and an early recognition of nontraumatic, spontaneous, intramural, large-bowel haematomas by surgeons is crucial, as that may prevent unnecessary exploratory surgeries. If the patient is stable, a colonoscopic biopsy may differentiate between a haematoma and a neoplasm when diagnosis is unclear. Although this is rare, it is reasonable that surgeons consider AIH as a differential diagnosis for a colonic mass in patients who are on anticoagulants [4–7].
A conservative treatment is advised as the optimal therapy for an AIH in the first instance [1,5,6]. Furthermore, some authors have suggested, that a surgical treatment should be preserved for those patients who have a doubtful diagnosis or for those who exhibit a deteriorating condition or an unrelenting intestinal obstruction or for the patients who exhibit signs of bowel necrosis or peritonitis. If an AIH is confirmed during a laparotomy, a more conservative procedure for the obstruction, like a diversion stoma, may be an another choice.
A complete resolution of the haematoma usually occurs within 3 weeks after its onset, which varies from 10 days to 2 months [2–4]. The factor which determines its prognosis is the extension of the haematoma [3] A high mortality rate is found in the patients with an extensive haematoma, such as the involvement of more than half the length of the small bowel. The reintroduction of the anticoagulant therapy after the resolution of a haematoma, can be done individually with a careful risk and benefit evaluation, since the incidence of recurrent intramural haematomas has been reported to be 3 in 5 cases after restarting on the anticoagulant therapy [2,3].
To conclude, a spontaneous, intramural, haematoma is an uncommon complication in the patients who are on excessive anticoagulation with warfarin. A history of anticoagulant use, with a prolonged INR value in the patients with abdominal pain, should alert the physicians or surgeons to search for this entity. It is extremely important to recognize this syndrome at its early stages, to avoid unnecessary surgeries, since the outcome is usually excellent after a conservative treatment.
[1]. Kwon C-II, Ko KH, Kim HY, Hong SP, Hwang SG, Park PW, Bowel Obstruction Caused by an Intramural Duodenal Hematoma: A Case Report of Endoscopic Incision and DrainageJ Korean Med Sci 2009 24:179-83. [Google Scholar]
[2]. TerKonda SP, Nichols FC III, Sarr MG, Spontaneous perforating hematoma of the rectum. Report of a caseDis Colon Rectum 1992 35:270-72. [Google Scholar]
[3]. Chaiteerakij R, Treeprasertsuk S, Mahachai V, Kullavanijaya P, Anticoagulant-Induced Intramural Intestinal Hematoma: Report of Three Cases and Literature ReviewJ Med Assoc Thai 2008 91(8):1285-90. [Google Scholar]
[4]. Krysa J, Shahabdeen M, South LM, A case of acute large bowel obstruction, presenting in a patient taking warfarinEmerg Med J 2003 20:e8 [Google Scholar]
[5]. Polat C, Dervisoglu A, Guven H, Kaya E, Malazgirt Z, Danaci M, Ozkan K, Anticoagulant-induced intramural intestinal hematomaAm J Emerg Med 2003 21:208-11. [Google Scholar]
[6]. Chin CC, Yeh CY, Kuo YH, Huang WS, Yeh CH, Wang JY, Colon Obstruction due to Anticoagulant Induced Intramural HematomaJ Soc Colon Rectal Surgeon (Taiwan) 2007 18:111-15. [Google Scholar]
[7]. Fischer J, Samson P, Robertson MG, Anticoagulant-induced intramural haematoma of the caecum mimicking a colonic tumourJ NZMA 2010 123(1315):75-77. [Google Scholar]