Bilateral Primary Fallopian Tube Carcinoma with the Classical Clinical Features: A Case Report
Neetha Vyas M1, Supriya Rai2, Lakshmi Manjeera3, Darshith Shetty4
1 Assistant Professor, K.S. Hegde Medical Academy, Nite University, Karnataka, India.
2 Professor, K.S. Hegde Medical Academy, Nite University, Karnataka, India.
3 Associate Professor, K.S. Hegde Medical Academy, Nite University, Karnataka, India.
4 Assistant Professor, K.S. Hegde Medical Academy, Nite University, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neetha Vyas M., ‘Ashraya’, 1st main, 3rd Cross, Subashnagar, Mangalore-575001, Karnataka, India.
Phone: +91 9900001287
E-mail: nvyas_21@yahoo.com
Bilateral primary fallopian tube carcinoma is a rare diagnosis in our gynaecological practice. Very often, the diagnosis is mistaken for an ovarian carcinoma or a tubo-ovarian mass. A correct, preoperative diagnosis is made only in 4% of the cases. This is due to the nonspecific symptoms. The Latzko’s triad of a watery vaginal discharge, a colicky lower abdominal pain and a pelvic mass is typical of a fallopian tube carcinoma, but this triad is noted only in less than 15% of the patients. Here, we are reporting such a case where the patient presented with all the classical features of a primary fallopian tube carcinoma. This case is also being reported for it’s extreme rarity.
Primary fallopian tube cancer, Adenocarcinoma, Clinical features
INTRODUCTION
Primary fallopian tube carcinoma has an incidence of an average of 0.3% of all the gynaecological cancers [1]. Bilateral fallopian tube cancer is reported to occur only in 20% of the cases [2]. A bilateral primary fallopian tube tumour has to be differentiated from a secondary tumour. Metastasis to the tubes is a bilateral process in 80% of the cases, with ovarian, endometrial or gastrointestinal cancer usually being the primary lesion [3].
CASE REPORT
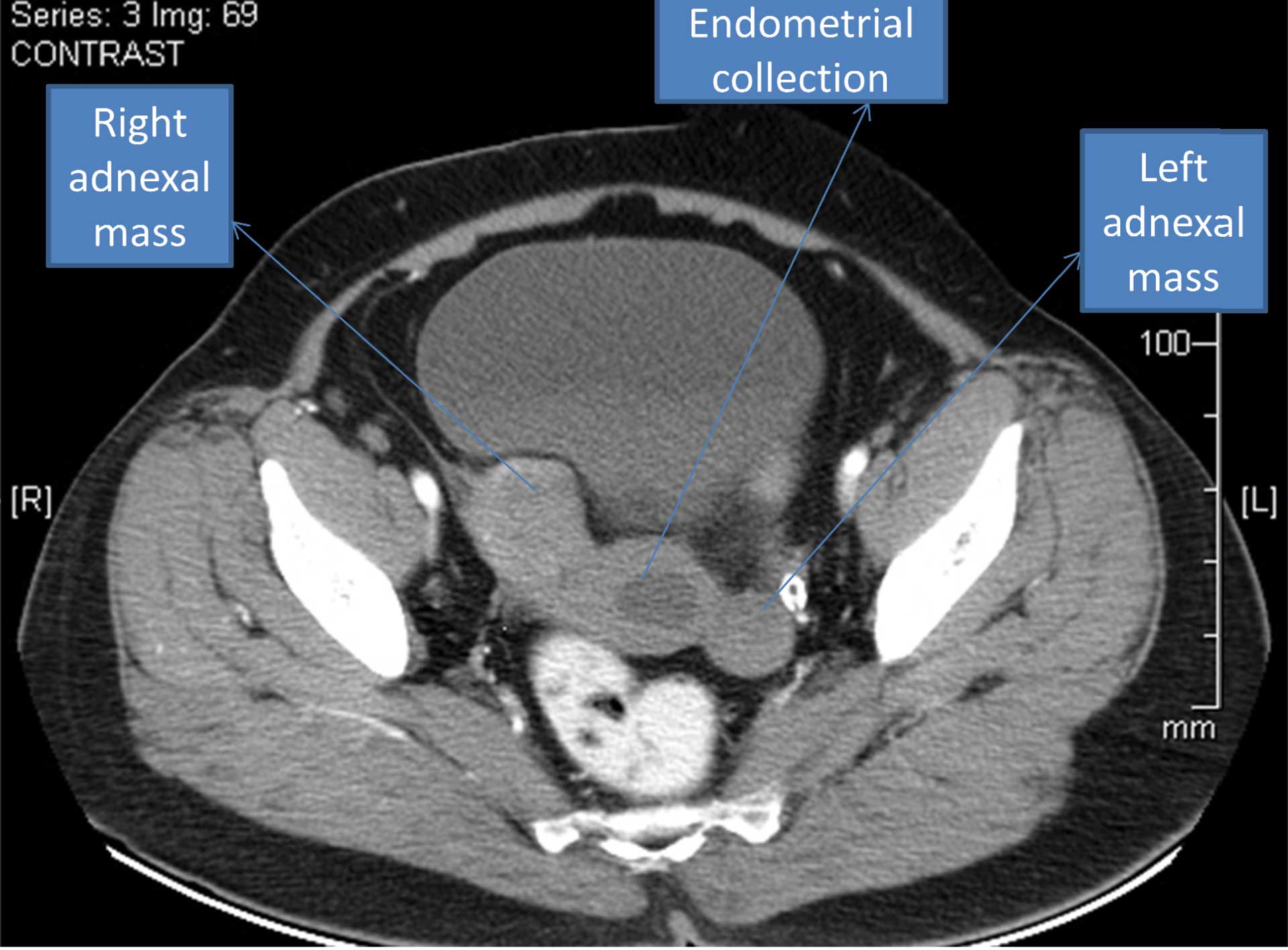
A postmenopausal parous woman presented to us with a one year old history of a watery discharge per vagina, an intermittent bloody discharge and lower abdominal pain. She had attained menopause 10 years back and her current age was 55 years. On abdominal examination, right iliac fossa tenderness was seen, but no mass was felt. The vaginal examination showed a serous discharge to be pooling in the vagina. A bimanual examination showed the uterus to be normal in size and a tender right adnexal mass was seen, which was palpable. Pap smear showed a normal cytology. Abdominal sonography showed a normal sized uterus with collection in the cavity. A well defined, right adnexal lesion of size, 4.5x5.4cm with solid and cystic components and a left adnexal hypoechoic lesion of size, 4.4x2cm were noted. There was no ascites. Doppler showed an increased vascularity. Contrast CT revealed an endometrial cavity collection with complex lesions in both the adnexa. The right adnexal mass measured 5.7x3.8cm, with solid and cystic components and the left adnexal mass measured 3.7x2.4cm, with a peripheral calcific density [Table/Fig-1]. Bilateral ovaries were not visualized. No ascites and enlarged lymph nodes were seen. The probable diagnosis which was made on the basis of the CT report was an ovarian malignancy. Her Ca-125 level was 564.
Contrast CT showing endometrial cavity collection with bilateral adnexal mass
The fluid which was obtained from the vagina was sent for cytology, which showed malignant cells. Though the probable diagnosis which was made on the basis of the CT scan was an ovarian malignancy, clinically, a suspicion of a fallopian tube carcinoma was made, due to the presence of the classical triad of a watery discharge, pelvic pain and a pelvic mass. A staging laprotomy with a total abdominal hysterectomy with a bilateral salphingo-oophrectomy and lymph node dissection was done. Intraoperatively, a bilateral tubal mass was found and both the ovaries were found to be separate from the mass. No peritoneal deposits or ascites were noted.
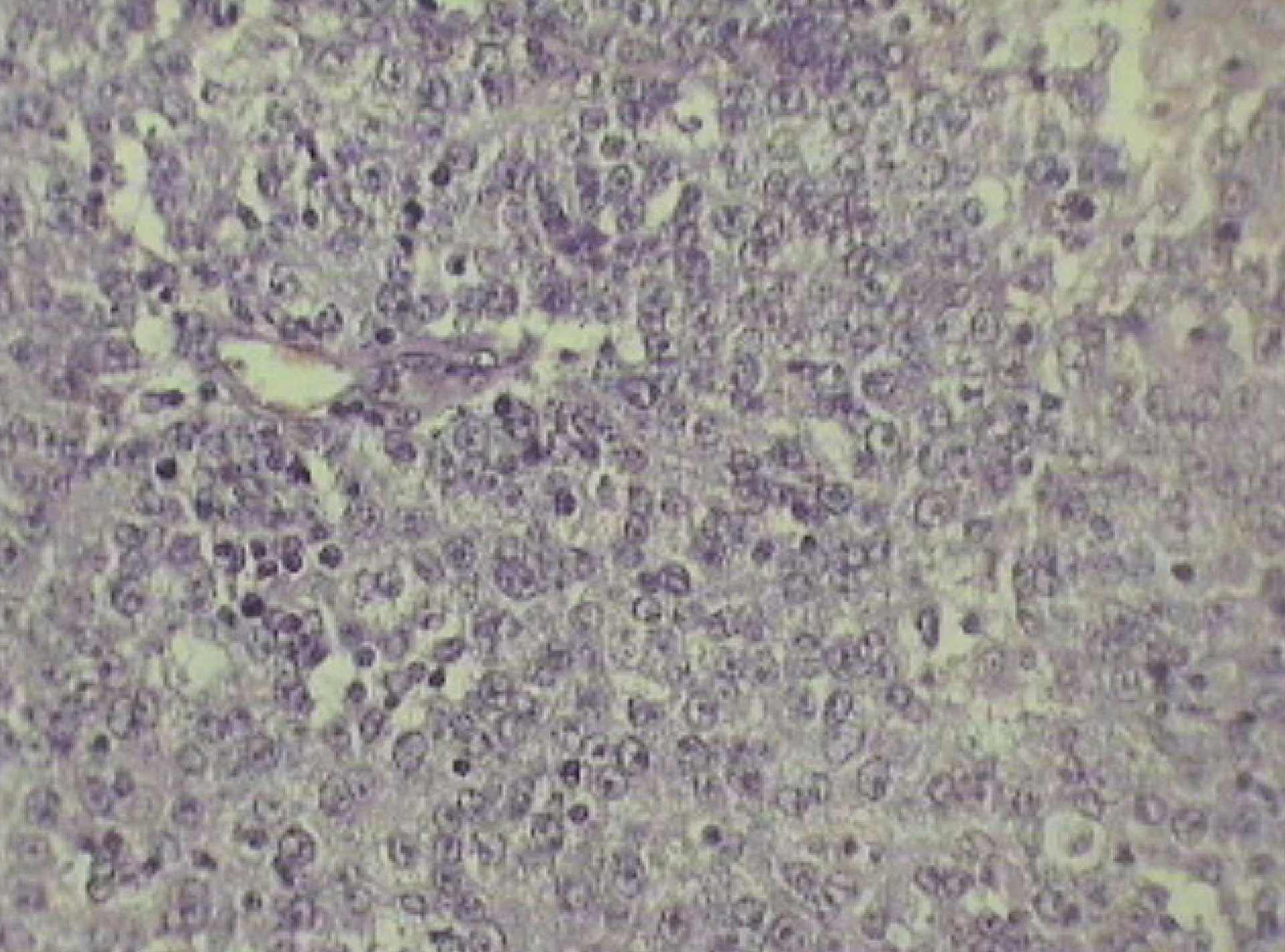
Histopathology revealed a right tubal papillary serous adenocarcinoma [Table/Fig-2] which was found to infiltrate the right ovary and a left tubal serous adenocarcinoma [Table/Fig-3 and 4]. The left ovary was normal. The omentum and the lymph nodes were free. The peritoneal washings showed no malignant cells. On the basis of these findings, a stage IIA primary fallopian tube cancer was confirmed. She received an adjuvant chemotherapy with carboplatin and paclitaxel.
Higher magnification of right fallopian tube with serous adenocarcinoma (H & E X100)

Cut section of left fallopian tube with the tumor

Higher magnification of fallopian tube with serous adenocarcinoma showing prominent papillarity (H & E X400)
DISCUSSION
Primary bilateral fallopian tube carcinoma is very rare. It is common in postmenopausal women in their fifth or sixth decades. Most of the patients are asymptomatic or they tend to present with non specific or insidious symptoms. In most of these patients, infertility and chronic pelvic disease are commonly associated. These factors were not seen in our patient. The clinical triad which was described by Latzko in 1916, of a vaginal watery discharge, a colicky lower abdominal pain and a pelvic mass, is rarely reported and all these features are usually present in less than 15% of the cases [4]. All these features were seen in our patient, which is a rarity. The pathognomonic feature is hydropstubae profluens. The intermittent colicky lower abdominal pain, which is due to the distension of the fallopian tube, with the fluid and pain, is relieved by the passage of a watery discharge per vagina. A study which analyzed 27 primary fallopian tube carcinomas, reported that only 11% of the patients had the characteristic features of a watery vaginal discharge, a colicky lower abdominal pain and a pelvic mass. They also suggested that this malignancy should be considered in the differential diagnosis of the perimenopausal and the postmenopausal women who presented with complex adnexal masses, an unexplained uterine bleeding, abnormal glandular cells on the cervico-vaginal smears and complicated pelvic inflammatory disease [5].
Although the classic triad of symptoms is said to be pathognomonic, the correct preoperative diagnosis is made in only 4% of the cases [6]. Often, the diagnosis is mistaken for ovarian cancer or a tubo-ovarian mass. The vaginal cytology findings are positive in only 10-20% of the patients. The imaging modalities like ultrasound and the CT/MRI features of tubal cancer are difficult to differentiate from those of ovarian cancer, unless the ovaries are separately visualized from the sausage shaped tubal mass.There was a case which was reported by Chisa H et al., regarding the use of sequential MRI in the preoperative diagnosis of bilateral primary fallopian tube carcinomas [7].
Clinically and histologically, it is difficult to differentiate a primary fallopian tube cancer from an ovarian cancer. Serous adenocarcinoma is the common histological feature in primary fallopian tube cancer. The other features are endometroid, transitional cell, clear cell and undifferentiated. Though differentiating a primary fallopian tube cancer from an ovarian cancer is relatively difficult, fortunately, the management remains the same. Primary fallopian tube cancer is typically managed by surgical staging, debulking and adjuvant chemotherapy. Currently, there is only minimal literature regarding the optimal treatment for primary fallopian tube cancer, due to the less controlled trials, as the incidence of this condition is rare. The preferred chemotherapeutic regimen consists of the platinum – taxane regimen [8]. But the 5 year survival rate of fallopian tube cancer, on an average, is poorer at 50% as compared to that of ovarian cancer, which is at 77% [9].
This case is being reported for it’s rare incidence and the typical clinical features which the patient presented with. Though the imaging modalities suspected an ovarian malignancy, due to the presence of the classical clinical features, it was thought to be a fallopian tube malignancy. A definitive diagnosis is usually made post operatively.
[1]. PNG Lawton F, Fallopian tube carcinoma – A reviewAnn Acad Med Singapore 1998 27:693-97. [Google Scholar]
[2]. Markman M, Zaino RJ, Fleming PA, Barakat RR, Carcinoma of the fallopian tube. In: Hoskins WJ, Perez CA, Young RC (eds)Principles and Practice of Gynecologic Oncology 2000 PhiladelphiaLippincott Williams and Wilkins:1099-112. [Google Scholar]
[3]. Honoré LH, Pathology of the fallopian tube and broad ligament. In: Fox H, Wells M.Haines and Taylor Obstetrical and Gynecologic Pathology 2003 5thNew YorkChurchill Livingstone:605-15. [Google Scholar]
[4]. Lawson F, Lees C, Kelleher C, Primary cancer of fallopian tube. In: Studd J. EditionProgress in Obstet and Gynecol 1996 UKChurchill Livingstone:393-401. [Google Scholar]
[5]. Chumnan K, Prapaporn Primary carcinoma of fallopian tube: A clinicopathologic analysis of 27 patientsJ Med Assoc Thai 2005 88:1338-43. [Google Scholar]
[6]. Riska A, Lemien A, Updating on primary fallopian tube carcinomaActa Obstet Gynecol Scand 2007 85:1419-26. [Google Scholar]
[7]. Hoskawa Chisa, Tsubakimoto Mitsuo, Yuichi I, Tetuso N, Bilateral primary fallopian tube carcinoma: findings on sequential MRIAJR 2006 186:1046-50. [Google Scholar]
[8]. Pectasides D, Pectasides E, Econompoulus T, Fallopian tube carcinoma: a reviewOncologist 2006 11:902-12. [Google Scholar]
[9]. Rose P, Piver M.S, Tsuleada Y, Fallopian tube cancer – The Rosewell Park experienceCancer 1990 66:2661-67. [Google Scholar]