A pseudotumour is a rare presentation of bronchopulmonary tuberculosis which occurs in immunocompetent patients, which can simulate malignancy, both clinically and radiologically, and may cause delay in its diagnosis and treatment. The incidence of bronchopulmonary pseudotumours was found to vary from 2-4%, as was seen in various studies. A mycobacterial pseudotumour of the pleura is a rare entity. We are reporting a case of a pleura based tubercular pseudotumour in a 59 years old patient who presented with a four month history of the nonspecific symptoms of cough and chest pain. The radiological investigations showed that a pleural based mass lesion was occupying the right lower hemithorax. The initial biopsy was suggestive of a hyalinizing variant of an inflammatory pseudotumour. The follow-up surgical resected mass was consistent with the features of a tubercular granuloma. The clinical presentation and the histopathological findings have been presented, with a brief review of the literature. Due to its varied and unusual presentation, bronchopulmonary tuberculosis should always be kept in mind when a patient with a similar clinical and a radiological picture is being evaluated.
Tuberculosis, Malignancy, Pseudotumour, Pleura
INTRODUCTION
An inflammatory pseudotumour which was originally described as occurring in the lungs, is a relatively rare entity and the result of aetiologically diverse processes, being either the histological expression of an infective or a reactive/reparative process. Pseudotumours are rare presentations of Mycobacterium tuberculosis or of a non tuberculous mycobacterial infection, which particularly affect immunosuppressed individuals with or without Acquired Immunodeficiency Syndrome (AIDS). These have been reported in various extrapulmonary anatomic locations such as the lymph nodes, spleen, appendix, liver, kidney, breast, pancreas, etc. [1–3]. Tubercular pseudotumours can occur in immunocompetent patients or following a transplant, which can mimic lung cancer [4]. Over a period of 11 years, 12 cases of tuberculous pseudotumours were reported among 341 cases of pulmonary tuberculosis (3.5%), with a mean age of 45 years and a consistent history of smoking. The patients usually present with nonspecific symptoms such as cough and chest pain. Making a positive diagnosis of a tubercular pseudotumour is difficult, because the clinical and the radiological presentations may closely mimic those of lung cancer, especially as the cases are usually smear negative, leading to a very late diagnosis [5]. The incidence of the pleura based pseudotumours is rare and they are limited to case reports only [6]. Pleural pseudotumours with a tuberculous aetiology are extremely rare [7]. The confirmation of the tuberculous aetiology can be made by bacteriological culture, the polymerase chain reaction technique and by doing a histopathological examination of transbronchial, pleural biopsy or surgical specimens. The present article was aimed at highlighting the diagnostic dilemmas which were associated with the pleural tuberculous pseudotumour in a 59 year male, with a brief review of the literature.
CASE HISTORY
A fifty-nine year nonsmoker male presented with a 4 month history of productive cough and right lower chest discomfort. He had a history of fever, generalized weakness, and weight loss. He was nondiabetic, normotensive, nonalcoholic, and had no prior history of pulmonary tuberculosis. His physical examination revealed conjunctival pallor and decreased breath sounds in the right lower lung field. His routine laboratory evaluation revealed haemoglobin -108 gram /L and a total leukocyte count of 11x109/L, with a neutrophil prominence and an erythrocyte sedimentation rate of 20 mm/hour. The initial microbiological studies for pyrexia of unknown origin, such as sputum for Acid Fast Bacilli (AFB) and microbiological cultures for Brucella, Salmonella, and Leptospira, were negative. The viral markers were also negative. His chest X-ray showed a pleural based mass lesion with calcification and irregular infiltrative margins, which was suggestive of a malignancy. A thoracic non contrast computed tomogram demonstrated a mass lesion which involved the pleura and extended into the soft tissue plane in the right hemithorax with mediastinal adenopathy, which was suggestive of a mesothelioma or lung carcinoma, with chest wall involvement.
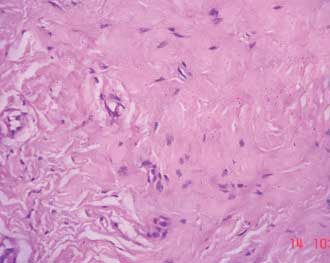
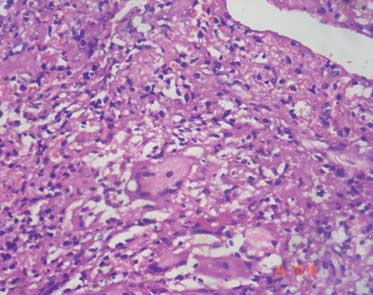
A histopathological examination of the initial biopsy of the mass showed a relatively paucicellular lesion which was comprised of hyalinized stroma, collagen bundles which were admixed with sparse fibroblasts, stellate shaped myofibroblasts and mononuclear inflammatory cells. There was no evidence of cellular atypia or mitosis. These findings were suggestive of an inflammatory pseudotumour (hyalinizing variant) [Table/Fig-1]. Following the biopsy report, a right posterior lateral thorocotomy was done under general anaesthesia. Intra operatively, the intercostal muscles was fibrosed. There was calcification and fibrosis of the parietal and the visceral pleura, with pus collection. The empyema was decorticated. The surgical resected specimen consisted of multiple grey brown tissue bits and bony hard bits, along with purulent material, which altogether measured 11x7x0.5 centimetres. The histopathological examination revealed extensive areas of caseating necrosis with epithelioid granulomas and Langhan giant cells, which were consistent with the features of tuberculosis [Table/Fig-2]. However, the Ziehl Neelsen stain for tissue AFB was negative. By correlating the radiological and the histopathological findings, the diagnosis of a tuberculous pseudotumour of the pleura was made. The microbiological culture of the purulent material which was sent at the time of the surgery, revealed no growth of organisms after 48 hours of aerobic incubation, whereas the staining for AFB of the purulent material was positive, thus confirming the aetiology.
Photomicrograph of the section from the initial biopsy specimen showing relatively paucicellular lesion comprised of hyalinized stroma, collagen bundles admixed with sparse fibroblasts, stellate shaped myofibroblast and mononuclear inflammatory cells. There was no evidence of cellular atypia or mitosis noted. These findings were suggestive of an inflammatory pseudotumor (hyalinizing variant). (Haematoxylin & Eosin, 400X)
Photomicrograph of sections from open biopsy material showing areas of caseating necrosis, epithelioid granulomas, and Langhan giant cells consistent with tuberculosis (Haematoxylin & Eosin, 400X).
After the definitive diagnosis of a tubercular pseudotumour of the pleura was made, the patient was started on anti-tubercular therapy. The follow-up examination of the patient after 1 month was uneventful, with clinical improvement and partial regression of the pleural based lesion.
DISCUSSION
The infectious agents that are known to induce the morphological changes of a pseudotumour include M. tuberculosis, M.avium intracellulare, M.kansasii, Herpes virus-8, Epstein-Barr virus, Actinomyces, Histoplasma, etc. Until 2007, only 26 cases of mycobacterial pseudotumours were reported in the world literature, which most often involved the lymphnodes [1]. The incidence of bronchopulmonary tuberculous pseudotumours is less, even rarer in the pleura. In contrast to the findings of a recent study which was done by Chaouch et al., [5] our patient was a nonsmoker without any history of immunosuppression. The occurrence of this unique histologic response to M. tuberculosis might be partly attributed to the individual (genetic) immunological makeup [4].
A calcifying fibrous pseudotumour of the pleura is a distinctly rare entity of unknown aetiology and it occurs in children and young adults [6]. However, tuberculosis which produces a bilateral pleural thickening or which mimicks a pseudotumour, has been described by Le Guillou et al., [7]. The present case had a unilateral pleura based lesion with focal calcification and extension into the adjacent parenchyma, which was found to simulate a malignancy radiologically. The initial biopsy was suggestive of a hyalinizing variant of an inflammatory pseudotumour, which was confirmed to be due to tuberculosis on further evaluation. There are different histological variants of inflammatory myofibroblastic tumours, depending upon their cellularity and the inflammation. Tumours with a predominant myxoid stroma may be seen, while others may show hyalinized stroma. In some tumours, spindle shaped cells with storiform or fascicular patterns are seen. A variant with a prominent lymphoplasmacytic infiltrate has also been noted. Some lesions may also show large cells with nuclear atypia, which may resemble ganglion cells or Reed-Sternberg cells [8].
The unusual radiological patterns which are seen in pulmonary tuberculosis can be mistaken for those of a neoplasm. Even a bronchogenic carcinoma can mimic or may be masked by the coexisting pulmonary tuberculosis, especially if it is present in the same lobe. The radiological features of coexistent pulmonary tuberculosis and carcinoma are similar to those of a bronchogenic carcinoma without tuberculosis [9]. In a study which was done by Cherian et al., the most common, unusual, radiologic pattern of pulmonary tuberculosis was mass like densities which predominantly involved the lower lung region. These were not associated with fibro-productive satellite lesions or calcification or cavitation, and thus they simulated a malignancy [10]. The lack of awareness on the unusual radiologic patterns can be problematic in differentiating tuberculosis from a malignancy, as was seen in our case.
The mycobacterial pseudotumours in the pleura should be distinguished from the Inflammatory Myofibroblastic Tumours (IMTs), as the latter can have an aggressive clinical course, local recurrence, malignant transformation or true metastasis. The IMTs are characterized by a non-random chromosomal translocation which involves chromosome 2p23, that results in over expression of the anaplastic large cell lymphoma kinase (ALK) gene in upto 60% of the cases. These tumours are characterized by the proliferation of the spindle shaped fibroblasts and the plump myofibroblasts, and they are associated with the infiltration with plasma cells, lymphocytes, or eosinophils. In contrast, the tuberculous pseudotumours exhibit a less cellular proliferation of the spindle shaped histiocytes and/or the dendritic cells, along with a more heterogenous inflammatory component [1]. The presence of epithelioid granulomas with or without caseating necrosis confirms the exact nature of these lesions, even in the absence of demonstrable organisms, as was seen in the present case.
CONCLUSION
The present case emphasized the unusual presentation of a pleura based tuberculous pseudotumour, which can mimic a malignancy. It is of great importance that clinicians be aware of this unusual manifestation of a mycobacterial infection, to ensure an appropriate diagnostic work-up and initiation of a definitive therapy.
[1]. Androulakia A, Papathomasa TG, Liapisa G, Papacomstantinoub I, Gazoulic M, Inflammatory pseudotumour associated with Mycobacterium tuberculosis infectionInternat J Infect Dis 2008 12:607-10. [Google Scholar]
[2]. del Agua C, Felipo F, Paricio J, Equizabal C, Delgado M, Tuberculosis of the breast as a pseudotumoral imageBreast 2006 12:180 [Google Scholar]
[3]. Turan M, Sen M, Koyuncu A, Aydin C, Elaldi N, Pancreatic pseudotumor due to peripancreatic tuberculous lymphadenitisPancreatol 2002 2:561-64. [Google Scholar]
[4]. Sekosan M, Cleto M, Senseng C, Farolan M, Sekosan J, Spindle cell pseudotumors in the lungs due to Mycobacterium tuberculosis in a transplant patientAm J Surg Pathol 1994 18:1065-68. [Google Scholar]
[5]. Chaouch N, Saad S, Zarrouk M, Racil H, Cheikh RS, Diagnostic difficulty in bronchopulmonary tuberculous pseudotumorRev Mal Respir 2011 28:9-13. [Google Scholar]
[6]. Jiang K, Nie J, Wang J, Li J, Multiple Calcifying Fibrous Pseudotumor of the Bilateral PleuraJpn J Clin Oncol 2011 41:130-33. [Google Scholar]
[7]. Le Guillou F, Hubscher P, Cuvelier A, Quieffin J, Guyonnaud CD, Bilateral pleural thickening pseudo-tumour due to tuberculosisRev Mal Respir 2002 19:515-17. [Google Scholar]
[8]. Weiss SW, Goldblum JR, Enzinger and Weiss’s soft tissue tumors 2008 5thPhiladelphia, USAMosby Elsevier:284-89. [Google Scholar]
[9]. Kim YI, Goo JM, Kim HY, Song JW, Im JG, Coexisting bronchogenic carcinoma and pulmonary tuberculosis in the same lobe: radiologic findings and clinical significanceKorean J Radiol 2001 2:138-44. [Google Scholar]
[10]. Cherian MJ, Dahniya MH, Al-Marzouk NF, Abel A, Bader S, Pulmonary tuberculosis presenting as mass lesions and simulating neoplasms in adultsAustralas Radiol 1998 42:303-08. [Google Scholar]