Intracystic Papillary Carcinoma of the Breast in Males: A Case Report and Review of the Literature
Hariprasad S1, Prajna Hariprasad2, Teerthanath Srinivas3
1 Assistant Professor, Department of Surgery, Raja Rajeswari Medical College, Bangalore, India.
2 Assistant Professor, Department of Obstetrics & Gynaecology, Kasturba Medical College, Mangalore, Karnataka, India.
3 Professor, Department of pathology, KS. Hegde Medical Academy, Mangalore, Karnataka, India.
NAME, ADRES, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hariprasad. S, Assistant professor, Department of Surgery, Raja Rajeswari Medical College, Bangalore, Karnataka, India.
Phone: 9448529402 Email: steerthanath@yahoo.com
Carcinoma of the male breast is a relatively rare disease that accounts for less than 1% of all the cases of cancer in men. Intracystic Papillary Carcinoma (IPC) is an extremely rare disease of the male breast, with a few case reports. The prognosis is excellent for the patients who are diagnosed with IPC, regardless of whether the tumour is in-situ or of an invasive type. We are reporting the case of a 50 year old man who presented with a painless cystic lump in the left breast. Ultrasonography revealed an intracystic tumour. Fine needle aspiration suggested a papillary tumour. The patient underwent simple mastectomy without a sentinel lymph node biopsy. The final pathologic examination revealed an intracystic papillary carcinoma of a low nuclear grade without an invasion.
Intracystic papillary carcinoma, Male breast cancer
INTRODUCTION
The breast cancer in males is relatively uncommon, accounting for less than 1% of all the breast cancers and less than 1.5% of all the malignancies in men. The incidence of male breast cancer has remained stable over the past four decades. Intracystic papillary carcinoma of the breast is a rare entity and it is known to account for between 0.5% and 1% of all the breast cancers [1]. The clinical presentation of papillary carcinoma in males is generally a painless, firm to cystic, subareolar mass. Grossly and microscopically, it is similar to its female counterpart and it can be in situ or of an invasive type [2]. We are reporting this case of an intra cystic papillary carcinoma of the breast in a male patient, along with the review of literature.
CASE REPORT
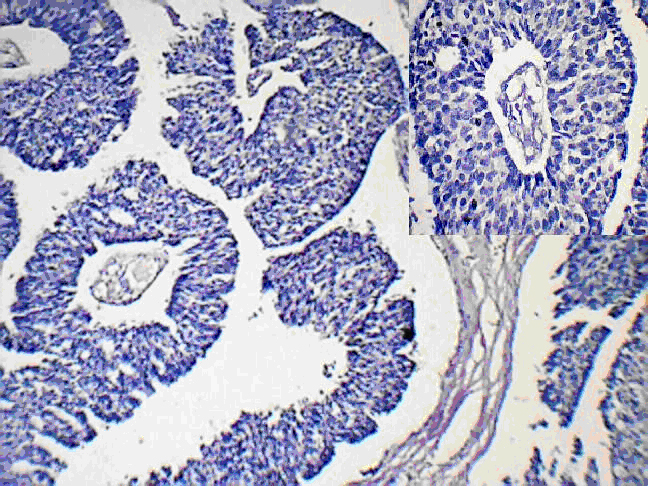
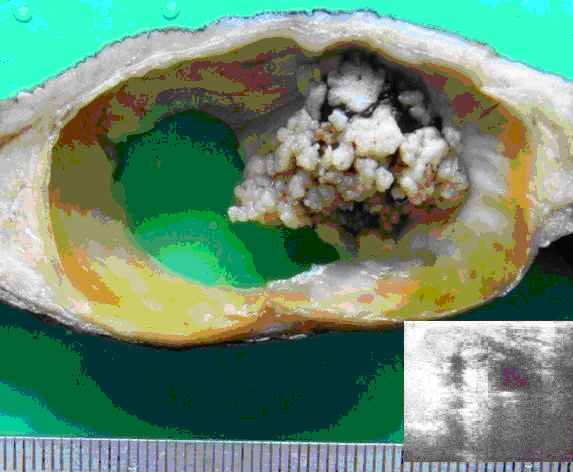
A 50 yr old man presented with a mass in the left breast which was there since 3 yrs. He had noticed a rapid increase in its size since the past 1 year, following a trivial trauma. The local examination revealed a subareolar cystic mass in the left breast, which measured 9x5cm and the overlying skin was uninvolved. The axillary nodes were not involved. The right breast appeared to be normal. Ultrasonography of the lesion suggested that it was an intracystic tumour. The radiological examination of the chest and the abdomen did not reveal any evidence of distant metastases. Fine needle aspiration cytology revealed a papillary carcinoma. A simple mastectomy of the left breast was done without a sentinel lymph node biopsy. The gross examination of the breast revealed that it measured 14 x 9 x 3 cms. The cut section showed a circumscribed cyst which measured 6 cms in diameter and which contained a brownish fluid. The cyst wall exhibited grey white papillary excrescences which protruded into the lumen [Table/Fig-1]. There was no nipple retraction or peude orange or ulceration of the overlying skin. Microscopically, the tumour showed a papillary lesion which was composed of numerous delicate, branching, papillary fronds which were lined by epithelial cells which showed stratification.
Cystic breast tumour with papillary excrescences. (Arrow pointing to papillary tumour). [Inset: Ultrasonography of the Cystic breast tumour]
These cells exhibited moderate pleomorphism and hyper chromatic nuclei, with a high nuclear cytoplasmic ratio [Table/Fig-2].
Fibrovascular stroma forming slender, branching papillary fronds lined by neoplastic epithelial cells (H and E, ×100) [Inset: section of a papillae with arrow pointing fibrovascular core]
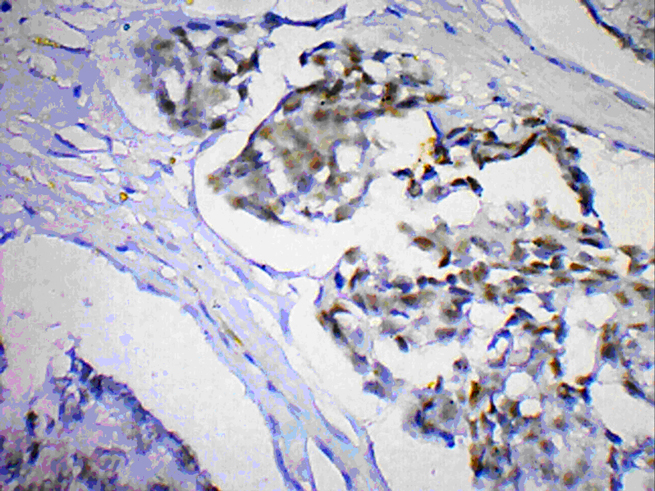
Mitotic figures were variably present. There was no tumour invasion beyond the cyst wall. The nipple and the surgical resected margins were free from tumour. The tumour cells were immunopositive for the oestrogen receptor and the progesterone receptor. Based on the above findings, a final diagnosis of a noninvasive intracystic papillary carcinoma (grade II) was made. Chemotherapy or radio therapy was not given. The patient had no recurrence of the tumour even after two years of regular follow up.
DISCUSSION
The incidence of male breast cancer varies by its geographical location. In most of the western countries, male breast cancers account for approximately 1% of the cases of breast carcinoma [1]. It is more frequent in African Americans than in the white Americans. The Japanese have a lower incidence rate as compared to the Chinese, African, Egyptian, and the Jewish populations. These geographic variations may be due to definable factors such as hyperoestrogenism and chronic liver diseases which are secondary to cancers or parasites [3].
Intracystic papillary carcinoma of the breast is a rare disease entity, which is most commonly encountered in elderly patients with a mean age of 70 years. The prevalence of male breast cancer increases with age [2]. Approximately 15-20% of the male patients with breast cancer have a positive family history [1]. The most common clinical finding in 75-90% of the patients is a painless mass, which is centrally located in 70-90% of the cases. IPC is usually located in the retroareolar or the central area, it arises in the larger, more centrally placed ducts, and the tumour development and its secretion cause the cystic dilatation [4]. Ultrasonography of the IPC lesions typically reveals a hypo-echoic area (which represents the cyst) with soft tissue echoes projecting from the wall of the cyst (intracystic tumour).
The aetiology of male breast cancer remains poorly understood, but an imbalance in the oestrogen-testosterone ratio has been definitely implicated. Oestrogen has a profound effect on the male breast tissue and it is able to stimulate the formation of the acini and the true lobules which are identical to those of the female breast [5]. The other aetiological factors include radiation exposure, drugs, head trauma (by increasing the prolactin production), local chest trauma, and smoking [1, 3]. An elevated risk has been seen in patients with undescended tests, congenital inguinal hernia, orchidectomy, orchitis, testicular injury and infertility. The other possible risk factors include obesity and cirrhosis, which result in a hyperoestrogenic state [3]. BRCA1 and BRCA2 can cause breast cancer in females, but only a BRCA2 mutation can confer a significant risk in men [1]. Tsuda et al., reported that a loss of heterozygosity on chromosome l6q was a useful marker for intracystic papillary carcinoma, since intraductal papilloma showed no loss of heterozygosity [6].
The papillary lesions comprise a wide spectrum in terms of their clinical presentation, behaviour, morphologic features and malignant potential. The papillary lesions in the breast have a wide spectrum of lesions that include benign papilloma, the papillary variants of Ductal Carcinoma In Situ (DCIS), and invasive papillary carcinoma. Traditionally, IPC was considered to be a variant of DCIS. Recent studies have suggested that IPC should be considered as a low risk invasive carcinoma [2]. Kraus and Neubecker established criteria to distinguish the benign papillomas from the papillary carcinomas [7]. Subsequently, the papillary carcinomas can be divided into the invasive and the noninvasive types. The further subdivision papillary carcinomas into 2 types was made by Carter et al., [8].
IPC has been divided into three types:
pure (with / without invasion),
with an associated intraductal carcinoma, and
with an associated, usual type of invasive ductal carcinoma.
Recently, Hill et al., by using myoepithelial cell staining, suggested a spectrum of its progression from an in- situ disease to an invasive disease. This “gold standard” method has a relatively high sensitivity and it denotes the invasiveness of the tumour cells in malignant, papillary breast lesions [7, 9]. In men, the predominant histologic subtypes of invasive carcinoma are infiltrating ductal carcinoma, which accounts for more than 80% of all the tumours, and papillary carcinoma, which makes up about 5% of all the tumours. Lobular carcinoma is much less common in men than in women and it represents only 1% of all the cases [1]. The rarer subtypes such as the medullary, tubular, mucinous and the squamous carcinomas, have all been reported in men. IPC may show four cellular patterns: cribriform, compact columnar epithelial, stratified spindle cell and a transitional cell form which resembles the urothelium, or a combination of two or more of these patterns may be seen. The tumours with high nuclear grades, histologic grades and large surface areas are more likely to metastasize to the lymph node or to recur locally. Some studies have reported the axillary lymph node metastasis and distant metastasis of IPC to be in the range of 0% to 11% for the axillary lymph node metastasis and 0% to 4% for the distant metastasis [2]. The carcinomas of the male breast have higher rates of oestrogen and progesterone receptor positivity than are found in women, but similar percentages may be expressed for HER2 and p53 in men and women. Our case was also HER2 positive [Table/Fig-3]. A review of literature revealed that between 18% and 58% of the male breast cancers tested positive for P53 [1].
Nuclei in the neoplastic papillae are immunoreactive for estrogen receptor (immunoperoxidase, ×100).
Solorzano et al., suggested that the standard treatment of IPC should be based on the associated pathology [10]. There is no definite guideline for the treatment of IPC, however, a radical surgical excision with a clear resection margin is the important mainstay of the treatment. Mastectomy is usually unessential, unless it is required, because IPC has an excellent prognosis, a low local recurrence, and a rare distant metastasis [9]. Anyway’s long-term follow-up is necessary after the surgical treatment. There has been no clear indication for an adjuvant endocrine therapy, even among the patients with oestrogen-receptor-positive tumours. Lefkowitz et al., reported a 10-year disease-free survival rate of 91% [4].
CONCLUSION
To conclude, invasive papillary breast carcinoma of males remains an uncommon disease. A triple assessment (i.e. a clinical examination and a radiological and a histological assessment) with a high level of clinical suspicion is necessary to diagnose intracystic papillary carcinoma in men, due to its rarity. Furthermore, genetic testing and risk-reducing mastectomy should also be considered in the cases with a strong family history for male breast cancer. Much research is needed to characterize further, the molecular and the biological properties of male breast carcinomas and their prognostic significance, so as to devise optimal treatment strategies.
[1]. Shah Parveen, Robbani Irfan, Shah Omar, Clinicopathological study of male breast carcinoma: 24 years of experienceAnn Saudi Med 2009 29:288-93. [Google Scholar]
[2]. Lee Se Kyung, Choi Jae Hyuck, Lim Hye In, Kim Wan Wook, Kim Sangmin, Cho Eun Yoon, Experience with Intracystic Papillary Carcinoma of the Breast at a Single Institute in KoreaJ Breast Cancer 2009 12:338-43. [Google Scholar]
[3]. Pant I, Joshi SC, Invasive papillary carcinoma of the male breast: Report of a rare case and review of the literatureJ Can Res Ther 2009 5:216-18. [Google Scholar]
[4]. Lefkowitz M, Usar CM, Lefkowitz W, Wargotz ES, Intraductal (intracystic) papillary carcinoma of the breast and its variants: A clinicopathological study of 77 casesHum Pathol 1994 25:802-09. [Google Scholar]
[5]. Shigeru Imoto, Takahiro Hasebe, Intracystic Papillary Carcinoma of the Breast in Male: Case Report and Review of the Japanese LiteratureJpn J Clin Oncol 1998 28:517-20. [Google Scholar]
[6]. Tsuda H, Uei Y, Fukutomi T, Hirohashi S, Different incidence of loss of heterozygosity on chromosome 16q between intraductal papilloma and intracystic papillary carcinoma of the breastJpn J Cancer Res 1994 85:992-96. [Google Scholar]
[7]. Kraus FT, Neubecker RD, The differential diagnosis of papillary tumors of the breastCancer 1962 15:444-55. [Google Scholar]
[8]. Fisher ER, Palekar AS, Redmond C, Barton B, Fisher B, Pathologic findings from the National Surgical Adjuvant Breast Project (protocol no. 4).VI. Invasive papillary cancerAm J Clin Pathol 1980 73:313-22. [Google Scholar]
[9]. Romics Laszlo, O’Brien M Emmet, Relihan Norma, O’Connell Fionnuala, Redmond H Paul, Intracystic papillary carcinoma in a male as a rare presentation of breast cancer: a case report and literature reviewJournal of Medical Case Reports 2009 3(13):1-4. [Google Scholar]
[10]. Solorzano CC, Middleton LP, Hunt KK, Mirza N, Meric F, Kuerer HM, Treatment and outcome of patients with intracystic papillary carcinoma of the breastAm J Surg 2002 184:364-68. [Google Scholar]