Myfibroma which was Associated with A Rudimentary Eyeball, which Masqueraded as an Ocular Palpebral Cyst
Hemlatha A. L.1, Sumana Sindhuram V.2, Asha U3
1 Professor and HOD, Department of Pathology Government Medical College, Mysore, Karnataka, India.
2 Assistant Professor, Department of Pathology Government Medical College, Mysore, Karnataka, India.
3 Consultant Pathologist, Private.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemalatha A. L., Professor and HOD, No. 156, 12th Cross, 2nd Main, Jayanagar, Mysore, Karnataka-570 014, India.
Phone: 08453399335
E-mail: hlingappa@rediffmail.com
Myofibroma, a benign neoplasm of the myofibroblasts, is most commonly encountered in the head and neck region, which includes the scalp, the forehead, the parotid region and the oral cavity. It is most rarely reported in the eyelids. Ocular myofibroma typically presents during childhood and it is rare in older patients. One such rare case which occurred in a 26 year old female with a clinical diagnosis of a palperbral orbital cyst, which was associated with a rudimentary eyeball, has been presented here.
Rudimentary eyeballs which are associated with other congenital anomalies of the central nervous system, the female genital system and the skeletal system, have been frequently reported, but the occurrence of myofibroma in a rudimentary eyeball, as was seen in the present case, is an exceptional feature and an extensive review of literature did not reveal any report of such an occurrence.
Ocular, Myofibroma, Myofibromatosis
INTRODUCTION
A myofibroma was initially described in 1951 by Williams Schrum. It is either solitary or multiple and it typically presents in childhood, but it is a rare possibility in adults.
A deep seated myofibroma with multifocal patterns of involvement is referred to as myofibromatosis.
Its common site of occurrence is the head and neck region, which includes the scalp, forehead, parotid region and the oral cavity. The trunk is the second most commonly affected site, followed by the lower and the upper extremities. There are reports on solitary intra-osseous myofibromas which mostly affected the craniofacial bones. The commonly involved organs are the lung, heart, the gastro intestinal system, pancreas and the central nervous system. The orbit is a very rare site of involvement [1].
CASE REPORT
A 26 year old female presented with a painful, gradually enlarging nodule over the left lower eyelid. Her ocular examination revealed a rudimentary eyeball in the left eye and a firm, solid, solitary nodule which measured 3 cms in diameter, over the left lower eyelid. Both the eyes showed gross microphthalmos. Her systemic examination
did not reveal any associated anomalies in the female genitalia, and in the central nervous system or the skeletal system. A clinical diagnosis of a rudimentary eyeball with a left orbital palpebral cyst on the lower eyelid, was offered.
Per-operative findings:
The nodule was found to be situated below the rudimentary eye ball. The local excision biopsy specimen was submitted for a histopathological Examination.
Gross examination:
It showed a lobulated, solid, globular mass which measured 3 x 1.5 x 1 cms.
Cut-section: The mass was grey-white with focal tiny cystic spaces which were filled with a mucoid material.
Microscopy:
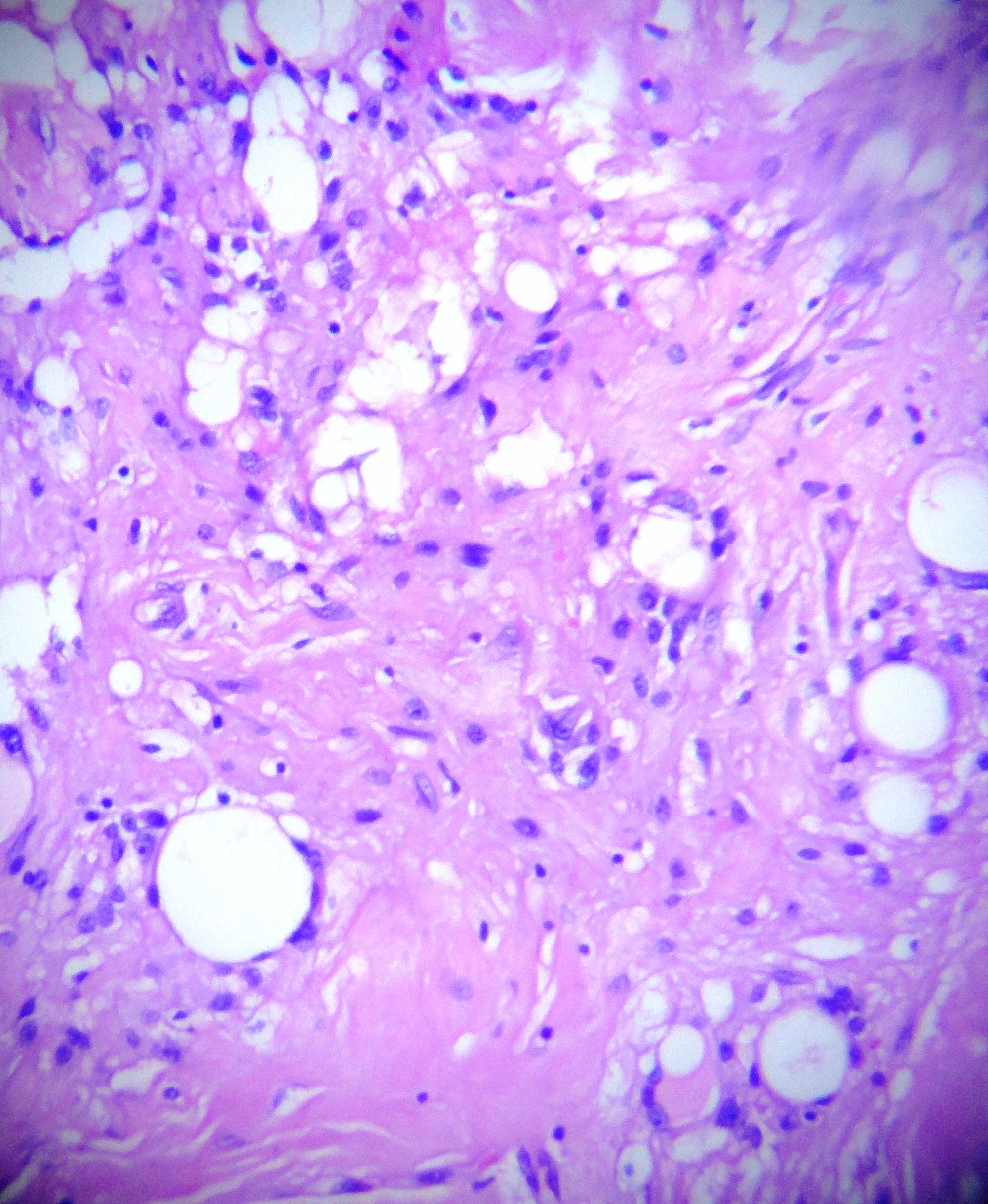
It showed a benign spindle cell tumour which was composed of spindle cells which were arranged in nodular, fascicular and whorling patterns [Table/Fig-1]. The tumour cells showed moderate amounts of eosinophilic cytoplasm and elongated oval to spindle blunt nuclei [Table/Fig-2]. The focal areas showed an admixture of mature adipose cells with large congested blood vessels which were arranged in hemangiopericytoma-like vascular patterns and hyalinized stromal fragments [Table/Fig-3]. Based on these findings, a histopathological diagnosis of a myofibrama was arrived at [Table/Fig-4], [Table/Fig-5].
Tumor cells in nodular pattern HE (x100)
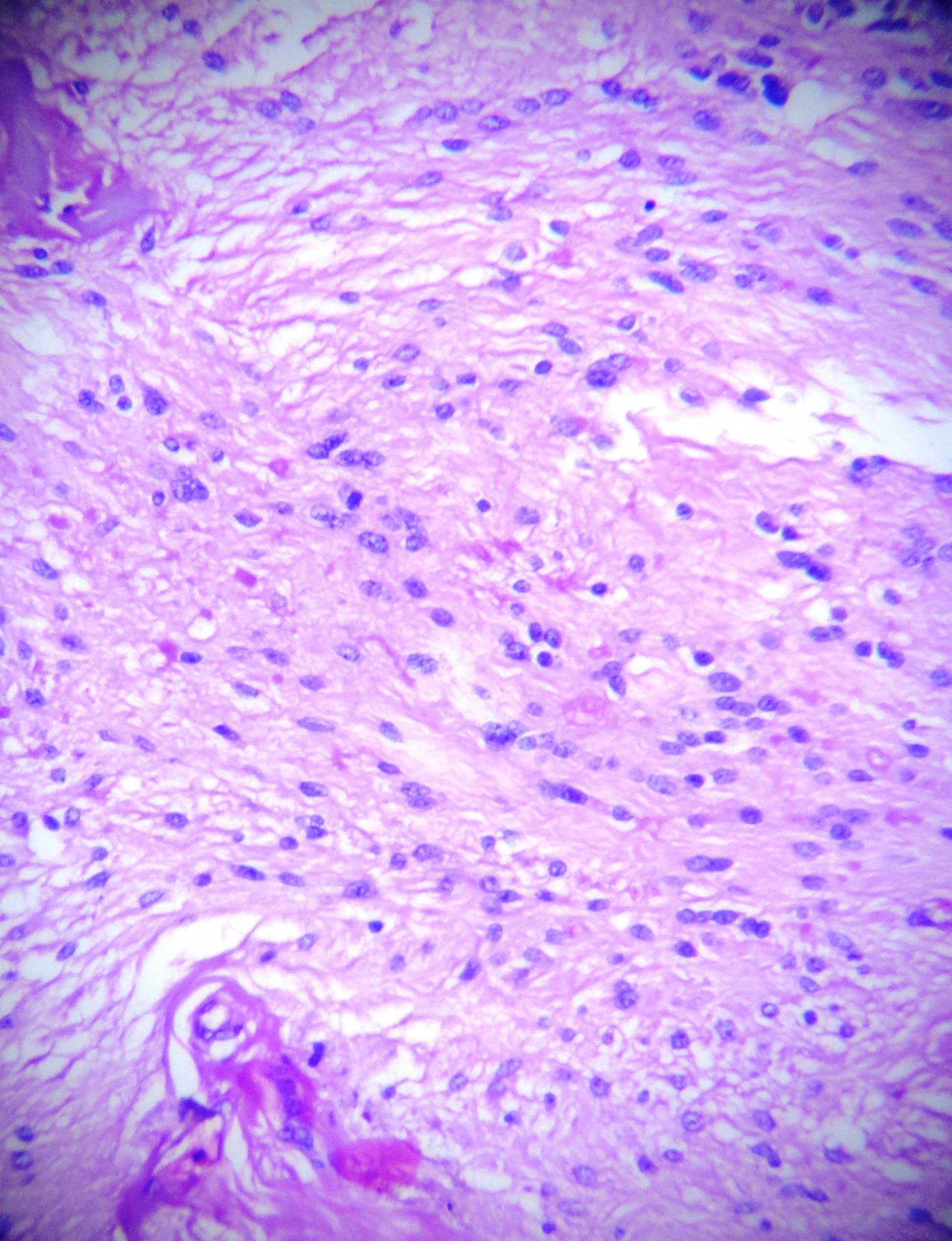
Tumor composed of single cells with elongated oval blunt nuclei in fascicles H&E (x400)
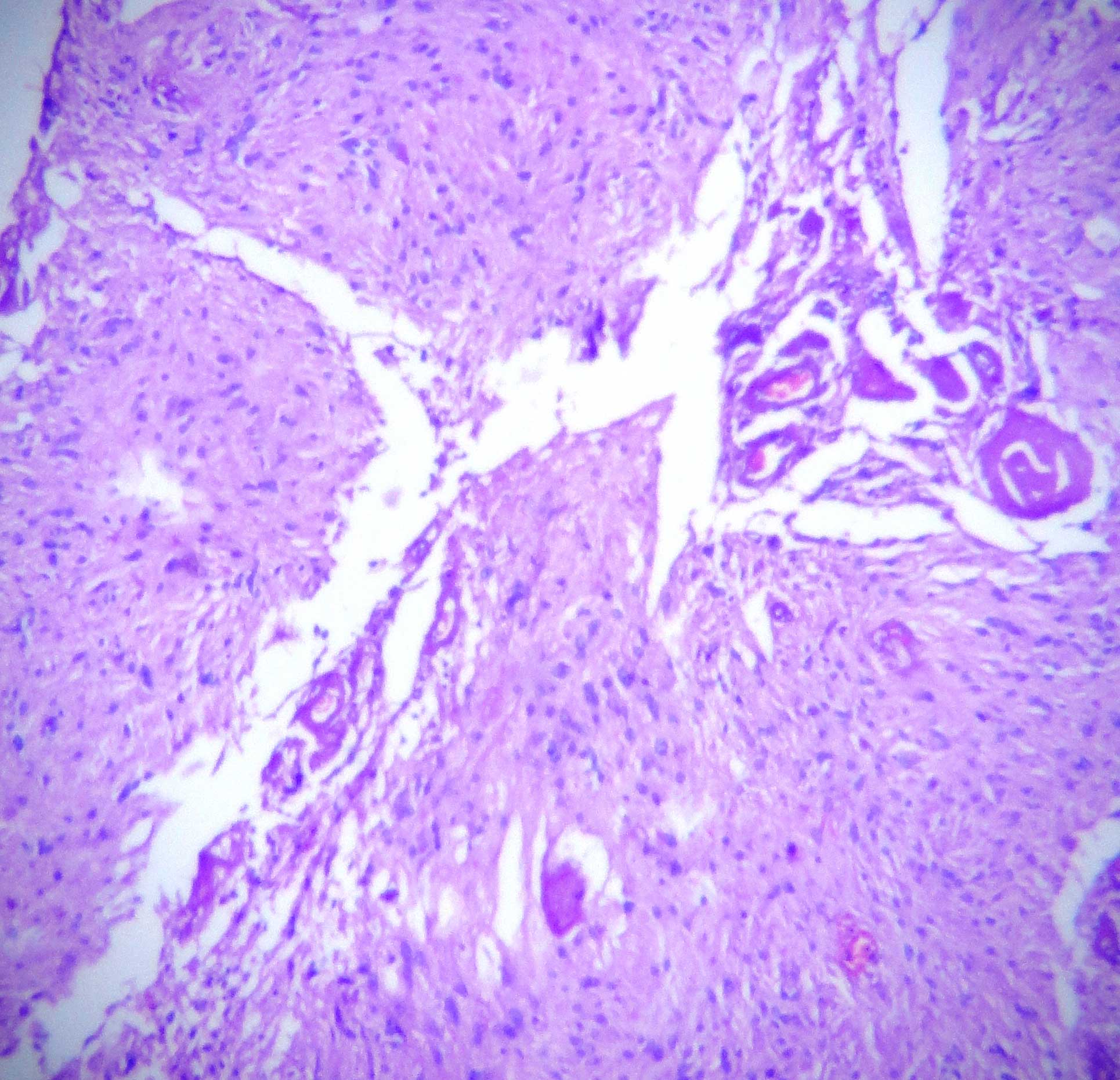
Mature adipocytes admixed with tumor cells (x400)
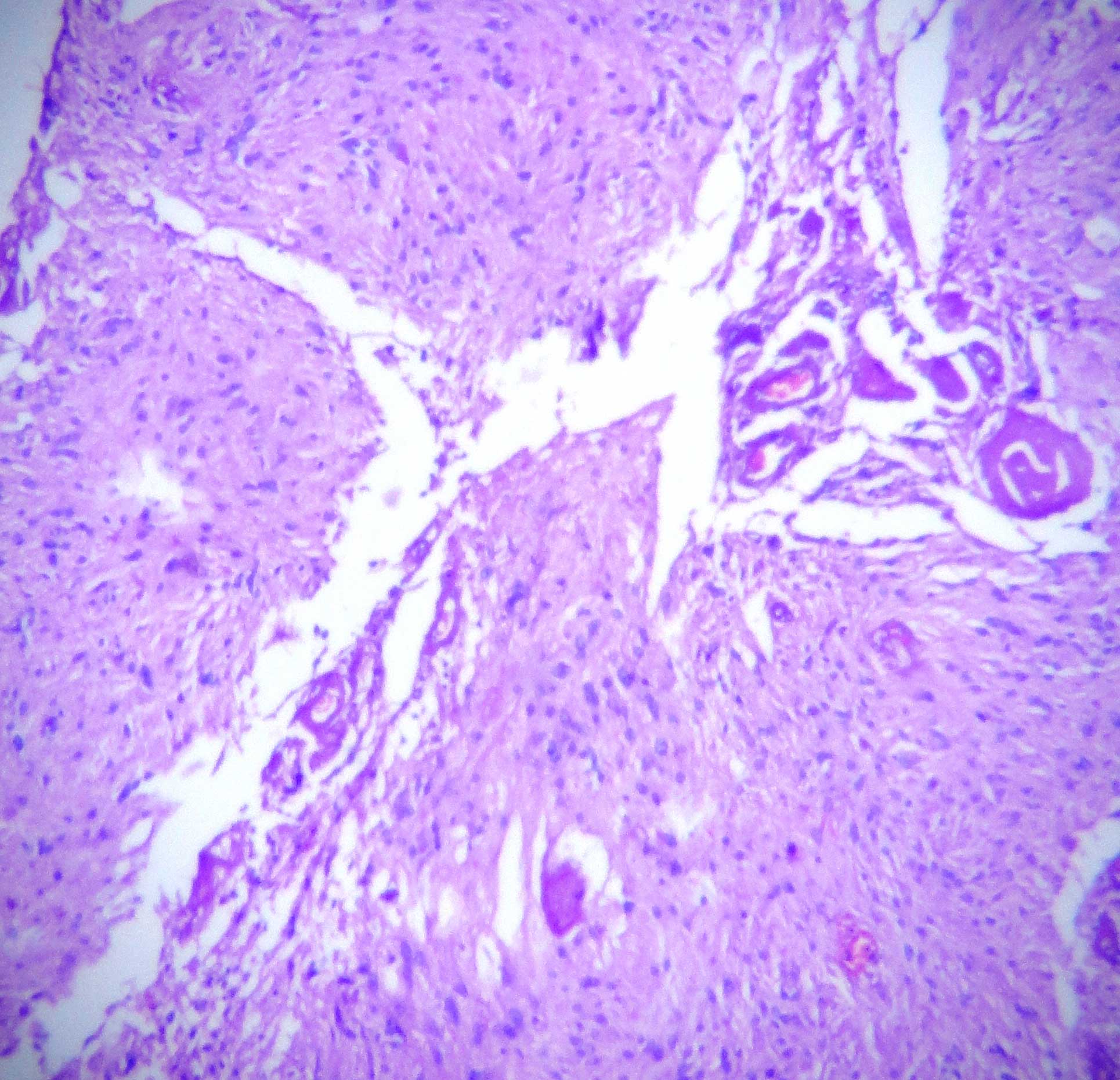
Large congested blood vessels in hemangiopericytomatous patterns amidst tumor cells HE (x400)
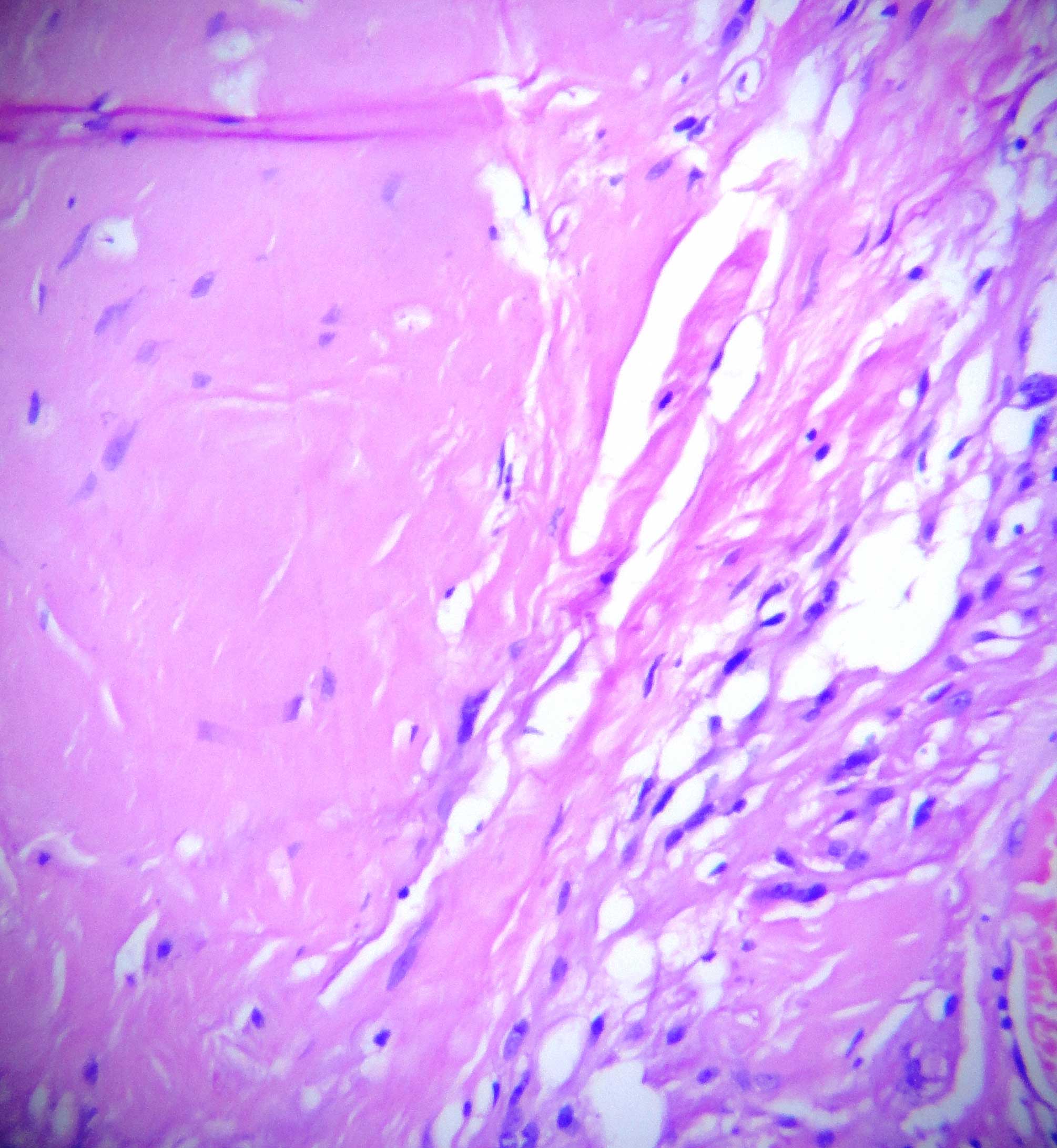
Hyalinized stromal fragment HE (x400)
Immuno histo chemistry:
It showed vimentin positivity and S100 negativity.
DISCUSSION
Myofibroma of the ocular region (which includes the orbits and the eyelids) is very rare. It is common in infants and childhood and its occurrence in the older age groups, as in the present case, is rare [2–6]. Albeit its occurrence at a rare site in an uncommon age group, as in the present case, a surgical pathologist needs to think about its existence when a spindle cell lesion with a nodular, fascicular or whorling growth patterns and areas of hyalinization, which are admixed with blood vessels, is seen.
Myofibroma and myofibromatosis are benign self limiting localized or generalized processes which consist mostly of myofibroblasts and pericytes [7–14]. Nodular fascitis is a close differential diagnosis, especially in adults, since the peripheral areas of myofibroma can resemble nodular fascitis. A myofibroma has a more prominent myxoid matrix and it may show hemangiopericytoma-like patterns. The other differential diagnoses include neurofibromas, fibrous histiocytomas and fibromatosis. The peripheral areas in a myofibroma resemble a neurofibroma but the myofibroblasts lack the S100 protein. A fibrous histiocytoma shows more pronounced storiform patterns. In fibromatosis, the lesion is less well circumscribed and it lacks the hemangiopericytoma – like vascular pattern [1].
Immunohistochemistry helps in ruling out the differential diagnosis and in clinching the diagnosis of a myofibroma [9].
If an isolated lesion is present, there is a chance of an excellent clinical outcome with a spontaneous involution [1].
Since an isolated lesion was present in our patient , it was removed by surgical excision. After a follow-up of six months, the patient was found to be symptom-free.
[1]. Weiss SW, Goldblum JR, Enzinger and Weiss’s Soft Tissue Tumors 2008 5thSt. Lousis, MoMosby [Google Scholar]
[2]. Shields CL, Husson M, Shields JA, Mercado G, Eagle RC Jr, Solitary intraaosseous infantile myofibroma of the orbital roofArch Ophthalmol 1998 116(11):1528-30. [Google Scholar]
[3]. Nam DH, Moon HS, Chung DH, Baek SH, Solitary infantile myofibroma of the orbital boneClin Experiment Ophthalmol 2005 33(5):549-52. [Google Scholar]
[4]. Choopong P, Nielsen PG, Perlman EM, Huang JJ, Dryja TP, Foster CS, Solitary myofibroma of the scleraCornea 2007 26(1):114-16. [Google Scholar]
[5]. Westfall AC, Mansoor A, Sullivan SA, Wilson DJ, Dailey RA, Orbital and periorbital myofibromas in childhood: two case reportsOphthalmology 2003 110(10):2000-05. [Google Scholar]
[6]. Kim SJ, Park HS, Seo SL, Lee YS, Chon DK, A Case of Solitary Adult Type Myofibroma in EyelidKorean J Dermatol 2003 41(2):272-27. [Google Scholar]
[7]. Weedon D, Skin Pathology 2002 2ndEdinburghChurchill Livingstone:927 [Google Scholar]
[8]. Silverberg SG, Silverberg’s Principles and Practice of Surgical Pathology and Cytopathology 2006 4thPhiladelphiaChurchill Livingstone:315-17. [Google Scholar]
[9]. Fletcher CDM, Diagnostic Histopathology of Tumors 2002 782ndLondonChurchill-Livingstone:1494 [Google Scholar]
[10]. Yanoff M, Fine BS, Ocular Pathology 2002 5thPhiladelphiaMosby:536 [Google Scholar]
[11]. Pilch BZ, Head and Neck Surgical Pathology 2001 PhiladelphiaLippincott Williams and Wilkins:404-05. [Google Scholar]
[12]. Farmer ER, Hood AF, Pathology of the Skin 2000 2ndNew YorkMcGraw-Hill:1170-73. [Google Scholar]
[13]. Rosai J, Ackerman LV, Rosai and Ackerman’s Surgical Pathology 2004 9thNew YorkCV Mosby:251-52. [Google Scholar]
[14]. Elder D, Elenitsas R, Bernett LJ Jr, Murphy FG, Lever’s Histopathology of the Skin 2005 21809thPhiladelphiaLippincott Williams and Wilkins:2251-52. [Google Scholar]