Moyo Moya Disease (MMD) is a rare, progressively stenotic condition of the intracranial arteries with various cerebrovascular manifestations. Ocular manifestations are seen very rarely and there are only few case reports of ocular perfusion anomalies. Central Retinal Artery Occlusion (CRAO) can be caused by atherosclerosis related thrombosis, carotid embolism, cardiac embolism, thrombophilic disorders, giant cell arteritis, etc. We are reporting a 26 years old patient with CRAO in the right eye, who was found to have the typical features of MMD on cerebral angiography. CRAO with MMD is a rare occurrence.
Moya moya disease, Central retinal artery occlusion, Cerebral angiography
INTRODUCTION
Moya Moya Disease (MMD) involves a progressive stenosis of the intracranial carotid arteries and its proximal branches, resulting in multiple cerebrovascular complications. An ocular involvement is rare, with very few case reports of varying ophthalmic manifestations [1–7]. Ocular perfusion related problems like retinal or choroidal vascular occlusions have rarely been reported [8–13]. We are reporting a case of a right sided Central Retinal Artery Occlusion (CRAO) with an angiographic evidence of MMD.
CASE REPORT
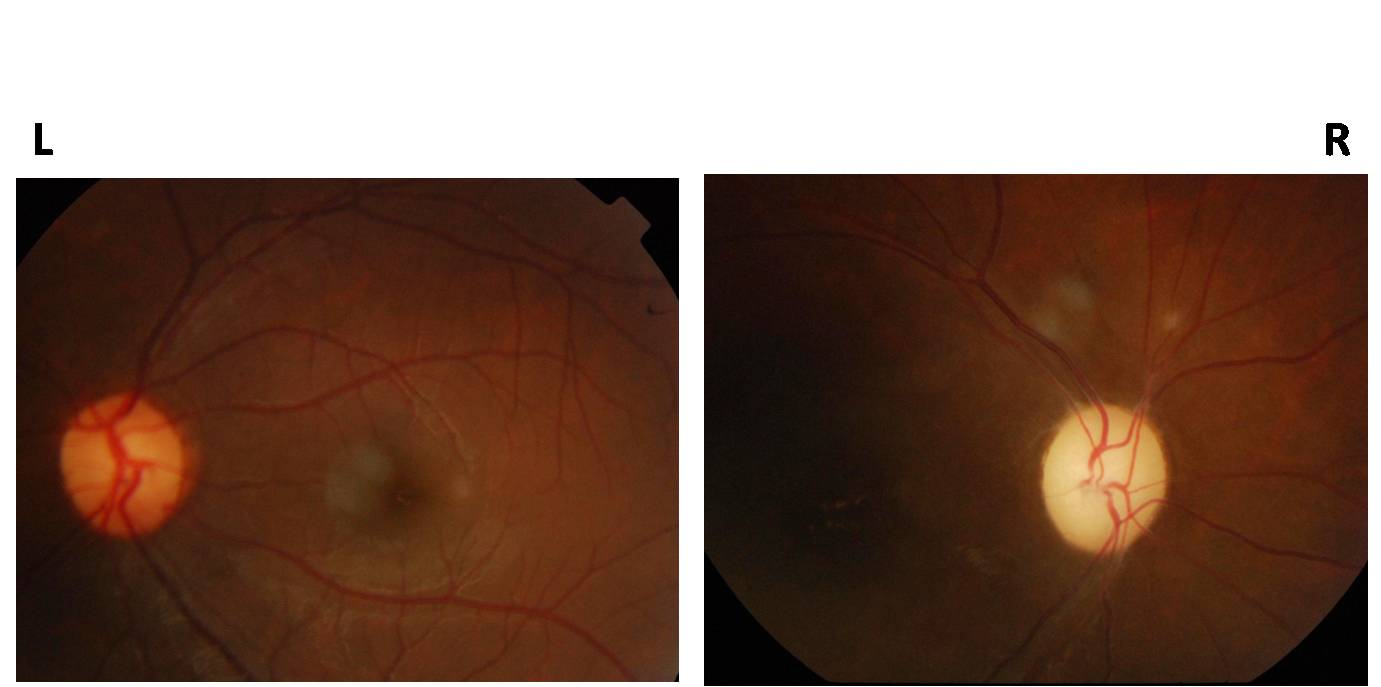
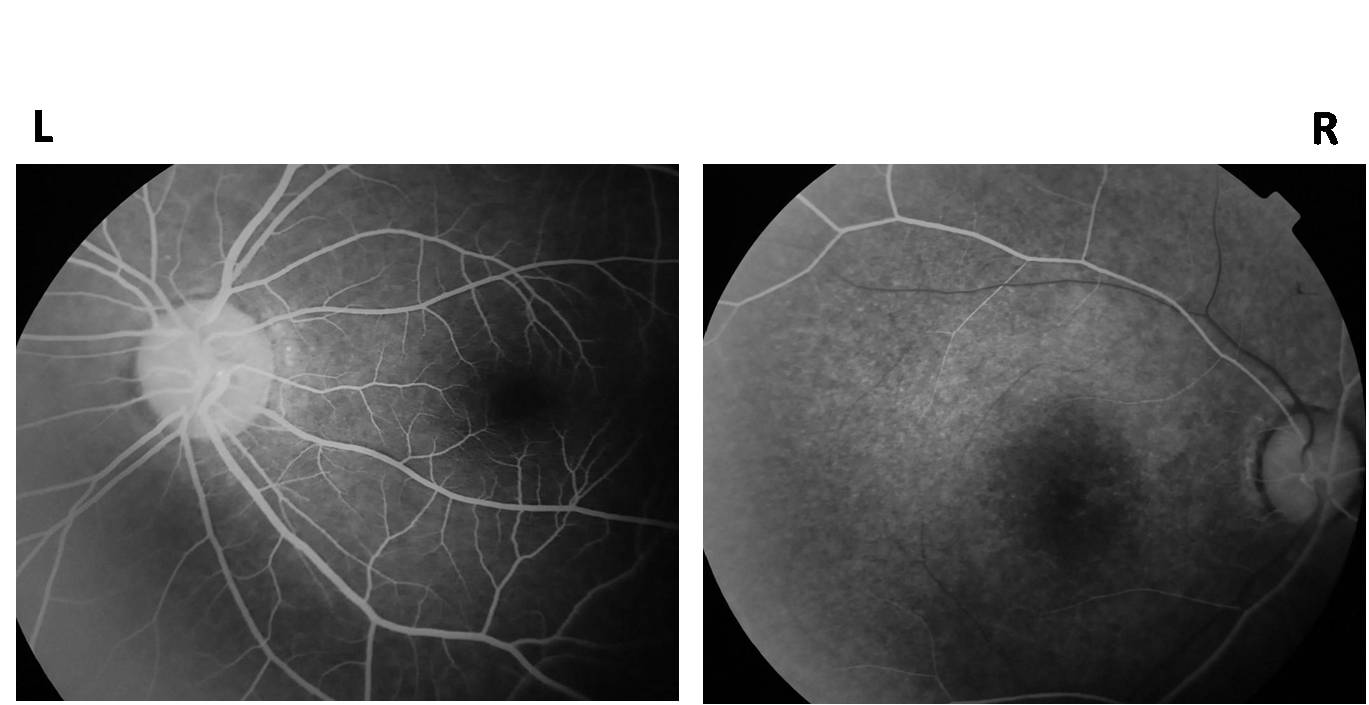
A 26 years old male presented with loss of vision in the right eye of 2 month’s duration, which was sudden in onset and for which he had received treatment elsewhere. On examination, he was found to have visual acuity of only the perception of light in the right eye, with an afferent pupillary defect. An examination of the right eye fundus showed a pale disc with arteriolar attenuation [Table/Fig-1]. The left eye was normal. Fundus Fluorescein Angiography (FFA) revealed a delayed retinal arterial filling in the right eye, as compared to the left eye [Table/Fig-2]. The presence of a normal choroidal fluorescence helped in establishing a diagnosis of right CRAO.
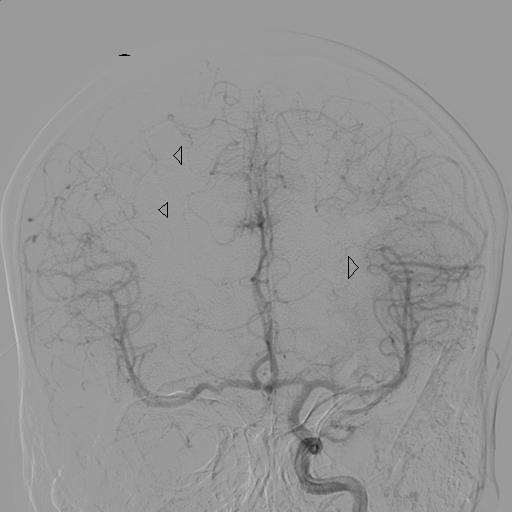
Carotid angiogram showing complete occlusion of right internal carotid artery at ostium. Arrow head pointing the ostium of right ICA.
Intracranial view appearing like a “puff of smoke”. Arrow heads pointing to the intracranial collaterals.
The general physical examination was otherwise normal, with no focal sensory or motor deficit.
His past records showed normal blood counts, erythrocyte sedimentation rate, random blood sugar levels, antinuclear antibody titres and non reactive Venereal Disease Research Laboratory (VDRL) values. His echocardiography was also normal. A cerebral angiography was performed, which showed total occlusion of the right internal carotid artery, with the intracranial views showing multiple collaterals which appeared like a “puff of smoke”, which suggested a diagnosis of MMD [Table/Fig-3 and 4].
Fundus photograph showing a pale optic disc with attenuated retinal vessels in right eye and normal left eye fundus

Fundus fluorescein angiography showing delayed retinal arterial filling in right eye (at 26 seconds after dye injection) compared to left eye (at 24 seconds after dye injection)
The patient was started on antiplatelet drugs (a combination of aspirin and clopidogrel) and has been on follow-up for the past 6 months, without any new ocular or cerebrovascular events.
DISCUSSION
Moya moya disease is commonly seen in the Japanese population [14] but it can also occur in other populations [15,16]. It can present as a paediatric or an adult form, each with varied clinical presentations. Children present with repeated ischaemic events and adults present with haemorrhagic events [17]. The disease causes progressive occlusion of the circle of Willis, with abnormal dilated collateral vessels on cerebral angiography, which look like “a puff of cigarette smoke” (moya moya) [18].
The ocular manifestations of MMD are rare but they are varied in presentation. Noda et al evaluated 4 MMD patients with the ocular symptoms of amaurosis fugax, a decreased visual acuity, hemianopia and diplopia, but found no significant ocular findings [1]. Some ocular malformations like morning glory disc anomaly [2], microphthalmos [2], optic nerve hypoplasia [2], retinochoroidal coloboma [2], iris hypoplasia [3] and Peter’s anomaly [4], have been reported in paediatric MMD. A child with ocular ischaemic syndrome was diagnosed over the follow-up, to have MMD [5].
Ocular perfusion anomalies in adult MMD have been reported only in 2 cases in the literature. Chen et al., reported a case of anterior ischaemic optic neuropathy in a patient who had undergone an internal to external carotid artery bypass with a normal cerebral perfusion [6]. Ushimura et al., reported a pregnant woman with MMD in the fourth month of her gestation, with a sudden ophthalmic artery occlusion [7]. A retinal artery occlusion with an evidence of recanalization was seen in a 12 year old girl who also had positivity of the dual antineutrophil cytoplasmic antibodies [2]. Few cases of hemi CRAO, chorioretinal retinal atrophic patches, acute CRAO and central retinal vein occlusion, which were associated with MMD, have been reported [9–12]. Goodwin et al., have reported a case of sickle cell disease which was associated with MMD [13]. Our case presented with the clinical features of CRAO / ophthalmic artery occlusion with a pale optic disc and attenuated retinal blood vessels. But FFA helped in diagnosing CRAO because of the presence of a delayed retinal vascular filling in the presence of a normal choroidal flush. CRAO is rare in patients who are younger than 50 years of age and in the younger patients, emboli from the heart is the major cause. The highlight of this case is that MMD, as a cause of CRAO, is rare and MMD being a disease which is predominantly seen in the Japanese population, the association of MMD with CRAO in an Indian patient makes it a rare occurrence.
[1]. Noda S, Hayasaka S, Setogawa T, Matsumoto S, Ocular symptoms of moya moya diseaseAm J Ophthalmol 1987 15(103):812-16. [Google Scholar]
[2]. Bakri SJ, Siker D, Masaryk T, Luciano MG, Traboulsi EI, Ocular malformations, moyamoya disease, and midline cranial defects: a distinct syndromeAm J Ophthalmol 1999 127:356-57. [Google Scholar]
[3]. Khan N, Schinzel A, Shuknecht B, Baumann F, Østergaard JR, Yonekawa Y, Moya moya angiopathy with dolichoectatic internal carotid arteries, patent ductus arteriosus and pupillary dysfunction: a new genetic syndrome?Eur Neurol 2004 51:72-77. [Google Scholar]
[4]. Smith M, Heran MK, Connolly MB, Heran HK, Friedman JM, Jett K, Cerebrovasculopathy in NF1 associated with ocular and scalp defectsAm J Med Genet A 2011 155A(2):380-85. [Google Scholar]
[5]. Barrall JL, Summers CG, Ocular ischemic syndrome in a child with moya moya disease and neurofibromatosisSurv Ophthalmol 1996 40:500-04. [Google Scholar]
[6]. Chen CS, Lee AW, Kelman S, Wityk R, Anterior ischemic optic neuropathy in moya moya disease: a first case reportEur J Neurol 2007 14:823-25. [Google Scholar]
[7]. Ushimura S, Mochizuki K, Ohashi M, Ito S, Hosokawa H, Sudden blindness in the fourth month of pregnancy led to diagnosis of moya moya diseaseOphthalmologica 1993 207:169-73. [Google Scholar]
[8]. Sakalli H, Baskin E, Alehan F, Agýldere M, Akova YA, Caner H, Dual anca positivity in a child with moyamoya-like cerebral vascular changes: an unusual presentation with sudden homonymous hemianopsiaRheumatol Int 2012 32:3295-98. [Google Scholar]
[9]. Akkoyun I, Baskin E, Caner H, Agildere MA, Boyvat F, Akova YA, Hemicentral retinal artery occlusion associated with moya moya syndromeOphthalmologe 2006 103:888-91. [Google Scholar]
[10]. Harissi-Dagher M, Sebag M, Dagher JH, Moumdjian R, Chorioretinal atrophy in a patient with moya moya disease. Case reportJ Neurosurg 2004 10:843-45. [Google Scholar]
[11]. Chace R, Hedges TR, Retinal artery occlusion due to moya moya diseaseJ Clin Neuroophthalmol 1984 4:31-34. [Google Scholar]
[12]. Slamovits TL, Klingele TG, Burde RM, Gado MH, Moya moya disease with central retinal vein occlusion. Case reportJ Clin Neuroophthalmol 1981 1:123-27. [Google Scholar]
[13]. Goodwin LP, Vaphiades MS, Johnson AP, Stroud CE, Bilateral Central Retinal Artery Occlusion Associated with Moya moya Syndrome in a Sickle Cell Disease PatientNeurophthalmolgy (informa healthcare) 2008 32:21-26. [Google Scholar]
[14]. Ikezaki K, Inamura T, Kawano T, Fukui M, Clinical features of probable moya moya disease in JapanClin Neurol Neurosurg 1997 99(suppl 2):S173-S177. [Google Scholar]
[15]. Chiu D, Shedden P, Bratina P, Grotta JC, Clinical features of moya moya disease in the United StatesStroke 1998 29:134751 [Google Scholar]
[16]. Yilmaz EY, Pritz MB, Bruno A, Lopez-Yunez A, Biller J, Moya moya: Indiana University Medical Center experienceArch Neurol 2001 58:1274-77. [Google Scholar]
[17]. Fukui M, Research Committee on Spontaneous Occlusion of the Circle of Willis (Moya moya of spontaneous occlusion of the circle of Willis (“moya moya” disease)Clin Neurol Neurosurg 1997 99(suppl 2):S238-S240. [Google Scholar]
[18]. Suzuki J, Takaku A, Cerebrovascular ‘moya moya’ disease: disease showing abnormal net-like vessels in base of brainArch Neurol 1969 20:288-99. [Google Scholar]