An Interesting Case of Dysphagia in a HIV Patient
Deepak Madi1, Basavaprabhu Achappa2, John T. Ramapuram3, Nithyananda Chowta4, Soundarya Mahalingaman5
1 Assistant Professor, Department of General Medicine, Kasturba Medical College, Mangalore (affiliated to Manipal University), India.
2 Associate Professor, Department of General Medicine, Kasturba Medical College, Mangalore (affiliated to Manipal University), India.
3 Professor and Unit Chief Department of General Medicine, Kasturba Medical College, Mangalore (affiliated to Manipal University), India.
4 Additional Professor, Department of General Medicine, Kasturba Medical College, Mangalore (affiliated to Manipal University), India.
5 Associate Professor, Department of Paediatrics, Kasturba Medical College, Mangalore (affiliated to Manipal University), India.
NAME, ADDRESS, E-MAIL ID OF THE CORESPONDING AUTHOR: Dr. Basavaprabhu Achappa, Associate Professor, Department of General Medicine, Kasturba Medical College,(affiliated to Manipal University) Attavar,Mangalore,575001
Phone: 998017048
E-mail: bachu1504@gmail.com
Oesophageal tuberculosis is a rare disease. Tuberculosis (TB) can cause dysphagia due to oesophageal ulcers, Tracheo-Oesophageal Fistulas (TOFs) and an extrinsic compression which is caused by the mediastinal lymph nodes. A 33-year-old gentleman was admitted to our hospital for the evaluation of fever, dysphagia and cough. His chest X-ray was suggestive of miliary tuberculosis. A CT scan of his chest revealed miliary tuberculosis, mediastinal lymphadenopathy and pneumomediastinum. His sputum AFB (acid-fast bacilli) test was positive. An upper gastrointestinal endoscopy revealed a large ulcer in the oesophagus with a fistulous opening which was suggestive of a tracheo-oesophageal fistula. A biopsy from the ulcer was positive for AFB. The test for HIV-1 was positive. A nasogastric feeding tube was placed and the Anti Tubercular Therapy ( ATT) was started. The main aim of this case report is to sensitize the clinicians about the fact that Tuberculosis can present with dysphagia, especially in HIV patients.
HIV, Dysphagia, Tuberculosis, Oesophageal ulcer, Tracheo-oesophageal fistula
INTRODUCTION
Oesophageal disease occurs in as many as 30% of the HIV patients at some point during the course of the infection [1]. Candida, cytomegalovirus, Herpes simplex virus and non-specific ulceration of the oesophagus can cause dysphagia in HIV patients. The ulcers which are caused by cytomegalovirus and idiopathic ulcers are the most common causes of the oesophageal ulceration in HIV patients [2]. Tuberculous involvement of the oesophagus is rare [3]. Studies have estimated that oesophageal tuberculosis constitutes about 0.3% of the gastrointestinal TB cases [4]. We are presenting an interesting case of oesophageal tuberculosis in an immunocompromised patient.
CASE REPORT
A 33-year-old male was admitted to our hospital for the evaluation of fever, dysphagia and cough. He gave a history of low grade fever of 1 month’s duration. He complained of dysphagia for past 10 days. He also gave a history of cough for past 5 days. The cough was associated with a choking sensation. Choking and cough began immediately, following the ingestion of liquid or solid food. He also gave a history of breathlessness and anorexia. A history of alcohol consumption was present.
On examination, he was found to have cervical lymphadenopathy. His respiratory system examination revealed bilateral crepititions.
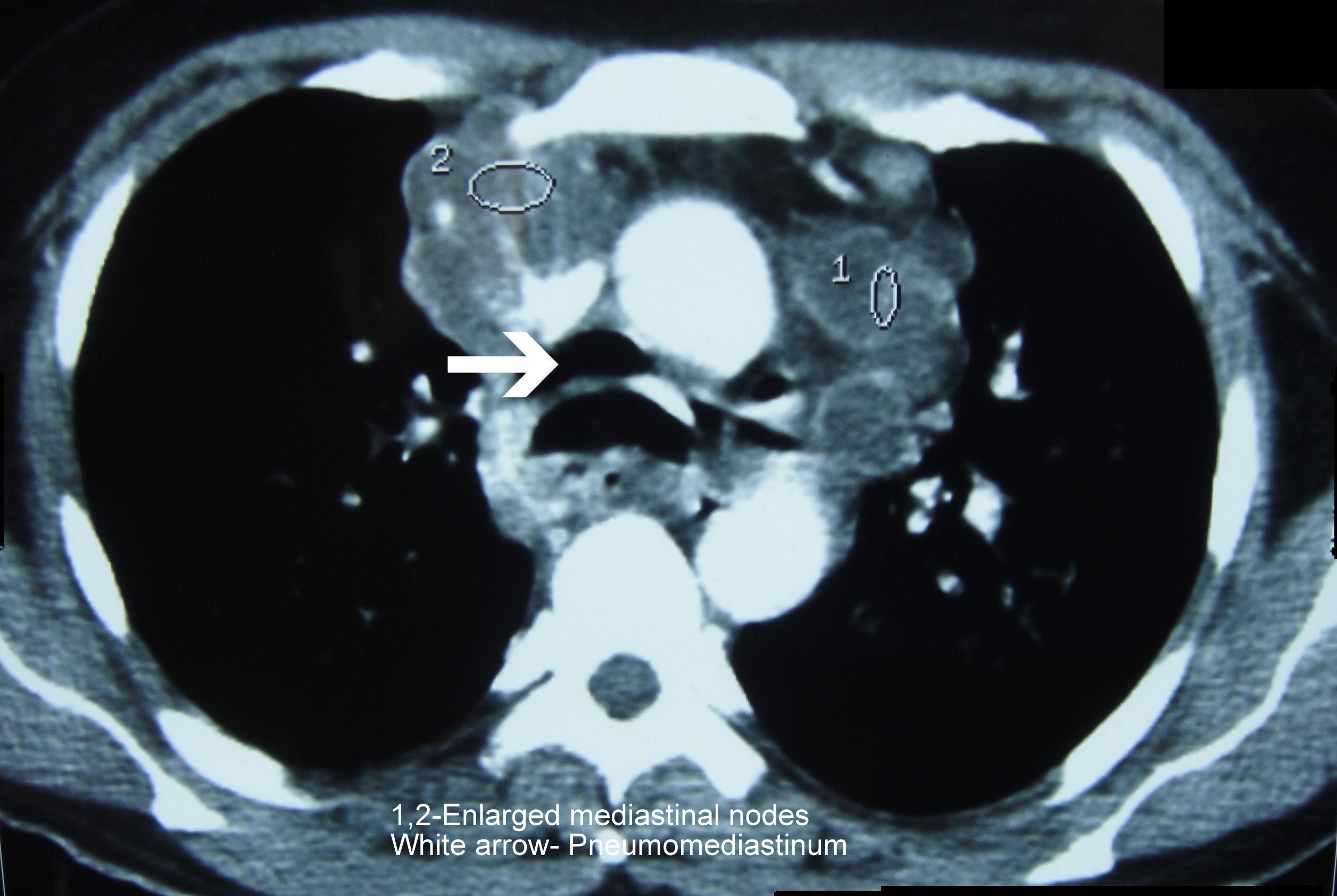
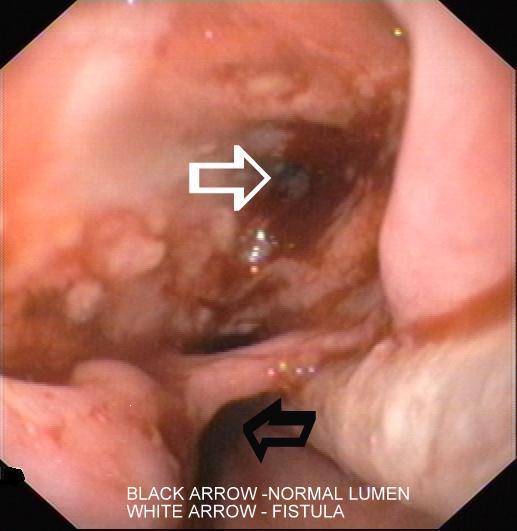
His lab investigations showed Hb -9.9 g/dl, Total White Blood Cell count -8700 cells/cu.mm, DC– N77 L-11, E-3 and M-9, platelet count-2,33,000 cells/cu.mm. ESR- 104mm/1st hour,Total.Bilirubin-1mg/dl, SGPT/SGOT(U/L)-172/83, ALP-157 U/L, total protein-7.5g/ dl, Serum Albumin-2.2g/dl and Serum Globulin-5.3g/ dl. His serum electrolytes, blood sugar and renal function were normal. The tests for HIV-1 and the Hepatitis B surface antigen were positive. His CD4+ count was 75cells/ìl. His chest X-ray was suggestive of miliary tuberculosis. His chest X-ray also showed Mahalingaman evidence of a mediastinal lymphadenopathy. Ultrasound of his abdomen showed cirrhosis of his liver. CT scan of his chest revealed miliary tuberculosis, mediastinal lymphadenopathy [Table/Fig-1] and pneumomediastinum. His sputum AFB (Acid fast bacilli) test was positive. FNAC of his cervical lymph nodes also showed AFB. An upper gastrointestinal endoscopy revealed a large ulcer in his oesophagus with a fistulous opening, which was suggestive of a Tracheo-Oesophageal Fistula (TOF) [Table/Fig-2]. Histology revealed an oesophageal mucosa with extensive ulceration and acute and chronic inflammatory cells. The staining for acid-fast bacilli was positive. A nasogastric feeding tube was placed and anti tubercular drugs were given.
CTScan of Chest showing Enlarged Mediastinal Nodes (1,2) and Pneumomediastinum(white arrow)
Upper GI Endoscopy Showing Normal Lumen (Black arrow) with Fistula (White arrow)
ART (Zidovudine, Lamivudine and Efaviranz) was started. Trimethoprim/sulfamethoxazole prophylaxis was started. Our patient did not want a percutaneous gastrostomy. He took treatment for the first 2 months and did not come for follow up.
DISCUSSION
Primary involvement of the oesophagus by tuberculosis is extremely rare, and an oesophageal involvement usually results from the extension of the tuberculosis from the adjacent structures such as the mediastinal lymph nodes or the lungs or by a haematogenous spread from a distant site [5]. Our patient had secondary oesophageal tuberculosis. An oesophageal involvement by tuberculosis usually affects the middle third of the oesophagus, at the level of the carina [6]. Even our patient had an ulcer in the middle third of the oesophagus.
Oesophageal tuberculosis is almost always associated with mediastinal lymphadenopathy, with or without a tracheo-oesophageal fistula [7]. Our patient had mediastinal lymphadenopathy and a tracheo-oesophageal fistula.
The most common symptom of oesophageal tuberculosis is dysphagia [8]. Patients with an oesophago-bronchial fistula present with cough after the ingestion of food [7,9]. A tuberculous dysphagia can be due to intrinsic oesophageal ulcers, tracheo-oesophageal fistulae and the extrinsic compression which is caused by the mediastinal lymph nodes. In 14 patients with dysphagia which was caused by TB, the aetiology was mediastinal and subcarinal lymphadenopathy in seven, it was tracheo-oesophageal fistulas in four, it was oesophageal ulcers in two, and it was cervical node suppuration in one [10]. The dysphagia in our patient was mainly due to the large oesophageal ulcer and the tracheo-oesophageal fistula.
‘Ono’s sign’ (uncontrolled coughing after swallowing) suggests the possibility of a tracheo-oesophageal fistula. Our patient had choking and cough after the consumption of food. Iatrogenic, malignant and traumatic causes have now superseded infection, which was formerly the predominant aetiology of acquired TOF [11,12]. Mediastinal tuberculous lymphadenitis can also cause dysphagia [13]. Tuberculous mediastinal lymphadenitis can also cause oesophageal ulceration and fistula.
An oesophageal endoscopy is the most important investigation in the evaluation of dysphagia. The endoscopic features of oesophageal tuberculosis are large oesophageal ulcers, tracheoesophageal fistulas, and chronic nonhealing ulcers [14]. Biopsies from the ulcer may show the classic granuloma in approximately 50% of the cases, whereas AFB are demonstrated in less than 25% of the patients [15]. A biopsy from the ulcer was positive for AFB in our patient. Bronchoscopy, with the application of methylene blue into the oesophagus, will show even a small fistula. Bronchoscopy and barium studies were not done in our patient. CT scan of the chest must be done to assess mediastinal adenopathy, an oesophageal rupture and pneumomediastinum. A spontaneous pneumomediastinum in tuberculosis has been reported in miliary as well as non-miliary tuberculosis [16].
Tuberculous tracheo-oesophageal fistulae usually require a combination of both surgical and medical treatments. Surgery consists of a simple division and closure or tracheal resection and reconstruction [10, 17]. However, there are case reports where the fistula had healed completely with medical therapy alone [7,18].Our patient did not want surgery. He was treated with Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. He completed 2 months of ATT and then did not come for follow up.
CONCLUSION
Candida, cytomegalovirus, Herpes simplex virus and non-specific ulceration of the oesophagus commonly cause dysphagia in an HIV patient. Although it is rare, oesophageal tuberculosis must be kept in mind in the patients who present with dysphagia, especially in the countries with a high prevalence of tuberculosis and HIV.
[1]. Connolly GM, Hawkins D, Harcourt-Webster JN, Parsons PA, Husain OA, Gazzard BG, Oesophageal symptoms, their causes, treatment, and prognosis in patients with the acquired immunodeficiency syndromeGut 1989 30:1033-39. [Google Scholar]
[2]. Wilcox CM, Schwartz DA, Clark WS, Esophageal ulceration in human immunodeficiency virus infection: Causes, response to therapy, and long-term outcomeAnn Intern Med 1995 123:143-49. [Google Scholar]
[3]. Jain SK, Jain S, Jain M, Yaduvanshi A, Oesophageal tuberculosis: is it so rare? Report of 12 cases and review of the literatureAm J Gastroenterol 2002 97:287-91. [Google Scholar]
[4]. Marshall JB, Tuberculosis of the gastrointestinal tract and peritoneumAm J Gastroenterol 1993 88:989-99. [Google Scholar]
[5]. Fahrny AR, Guirdi R, Farid A, Tuberculosis of the oesophagusThorax 1969 24:254-56. [Google Scholar]
[6]. Eng J, Sabanathan S, Tuberculosis of the esophagusDig Dis Sci 1991 36:536-40. [Google Scholar]
[7]. Devarbhavi HC, Alvares JF, Radhikadevi M, Esophageal tuberculosis associated with esophagotracheal or esophagomediastinal fistula: report of 10 casesGastrointest Endosc 2003 57:588-92. [Google Scholar]
[8]. Mokoena T, Shama DM, Ngakane H, Bryer JV, Oesophageal tuberculosis: a review of eleven casesPostgrad Med J 1992 68:110-15. [Google Scholar]
[9]. Dow C.J., Oesophageal tuberculosis: Four casesGut 1981 22:234-36. [Google Scholar]
[10]. Rathinam S, Kanagavel M, Tiruvadanan BS, Santhosam R, Chandramohan SM, Dysphagia due to tuberculosisEur J Cardiothorac Surg 2006 30:833-36. [Google Scholar]
[11]. Reed MF, Mathisen DJ, Tracheoesophageal fistulaChest Surg Clin N Am 2003 13:271-89. [Google Scholar]
[12]. Couraud L, Ballester ML, Delaisement C, Acquired tracheoesophageal fistula and its managementSemin Thorac Cardiovasc Surg 1998 8:392-99. [Google Scholar]
[13]. Ghimire MP, Walker RJ, Painful dysphagia in a case of mediastinal tuberculous lymphadenopathyPostgrad Med J 1985 61:427-28. [Google Scholar]
[14]. Abid S, Jafri W, Hamid S, Khan H, Hussainy A, Endoscopic features of esophageal tuberculosisGastrointest Endosc 2003 57:759-62. [Google Scholar]
[15]. Seivewright N, Fechally J, Wiks ACB, Primary tuberculosis of the esophagusAm J Gastroenterol 1984 79:842-43. [Google Scholar]
[16]. Dixit R, George J, Subcutaneous emphysema in cavitary pulmonary tuberculosis without pneumothorax or pneumomediastinumLung India 2012 29:70-72. [Google Scholar]
[17]. Mathisen DJ, Grillo HC, Wain JC, Hilgenberg AD, Management of acquired nonmalignant tracheoesophageal fistulaAnn Thorac Surg 1991 52:759-65. [Google Scholar]
[18]. Lee JH, Shin DH, Kang KW, Park SS, Lee DH, The medical treatment of a tuberculous tracheo-esophageal fistulaTuber Lung Dis 1992 73:177-79. [Google Scholar]