Fahr’s syndrome refers to a rare syndrome which is characterized by symmetrical and bilateral intracranial calcification. We are presenting a 63 year old male, who complained of progressive dysarthria of 6 months, which was associated with slowness of movements. His neurological examination revealed Parkinsonian features. His CT scan revealed a symmetrical large area of calcification over the basal ganglia, the thalamus and the cerebellum. The secondary causes of the bilateral calcification were ruled out to make the clinical diagnosis of Idiopathic Bilateral Striopallidodentate Calcinosis, which is otherwise called as the Fahr’s syndrome. Deposits of calcium and minerals cannot be linked to a single chromosomal locus and further genetic studies are in progress for identifying the chromosomal locus of the disease.
Fahr’s syndrome, Bilateral intracranial calcification
INTRODUCTION
Fahr’s disease is a rare, degenerative neurological condition which is characterized by the idiopathic calcification of the basal ganglia. This disease was described for the first time by a German neurologist, Karl Theodor Fahr in 1930. Neuropsychiatric, extra pyramidal and cerebellar symptoms, convulsive seizures, Parkinsonian features, dementia and speech disorders may accompany the clinical picture. There are also cases without neurological signs, which have been reported. This disease usually appears between the age of 40-60 years [1,2].
It may be rarely seen in children, who may present with choreoathetotic movements [1,3]. Within the basal ganglia, the globus pallidus is the most frequent site of the calcification but deposits may be present in the putamen, the caudate nucleus, the internal capsule, the dentate nucleus, the thalamus, the cerebellum and the cerebral white matter. Histologically, these deposits which contain proteins and polysaccharides, are found in the perivascular space and in the media layer of the small vessels. The pathogenesis is not known, but it may be secondary to the impairment of the blood brain barrier or to a neuronal calcium phosphoric metabolism disorder [2,4].
CASE REPORT
A 63 years old male presented to the outpatient clinic of a tertiary care centre with the chief complaint of a difficulty in speech since 6 months. He also had slowness of movements for the past one year. There was no history of any neuropsychiatric manifestations , mood disturbances or seizures. He was a hypertensive who was on regular treatment. His family history was not contributory. He was a non smoker and he denied any high risk behaviour.
He was moderately built and nourished without any skeletal abnormalities or neurocutaneous markers. He was conscious and was oriented to the time and place, with a normal memory and intelligence. His speech was slow and dysarthric. He had a mask like, expressionless face with a reduced blink rate. Bradykinaesia was noted, with a reduced arm swing and a stooped posture.
He did not have any motor weakness or cranial nerve involvement. There was no rigidity, tremor or abnormal movements. His coordination was intact. The primitive reflexes were absent. His other systemic examinations were normal.
His laboratory investigations revealed a normal haemogram and his renal parameters and liver function test were normal. His Erythrocyte Sedimentation Rate (ESR) was 47. The serum levels of calcium, magnesium, phosphorus and alkaline phosphatase were normal. The Parathyroid Hormonal (PTH) assay and the Serum Vit D assay showed normal values. The Ellsworth Howard test was not done as the serum levels of calcium, phosphorus and PTH were normal and as he did not have any skeletal abnormalities, thus ruling out the possibility of a parathyroid dysfunction. His thyroid function tests were normal. The CSF analysis was normal . The The VDRL and HIV tests gave negative results.
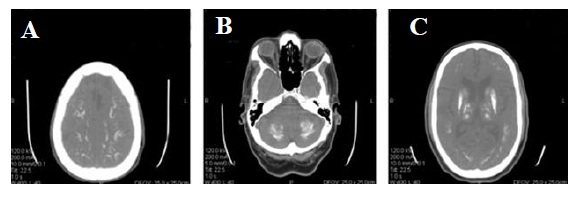
CT scan of the brain revealed bilateral, symmetrical, large areas of calcification over the basal ganglia, the thalamus, the cerebellum and the pons, which were suggestive of Fahr’s disease [Table/Fig-1]. The patient’s relatives were examined and no abnormalities were detected clinically in them. The patient was initiated on treatment with Levodopa.
CT Head showing bilateral symmetrical calcification in the cerebrum (fig-1a), cerebellum (fig-1b), basal ganglia (fig-1c)
DISCUSSION
Bilateral Striopallido Dentate Calcinosis (BSPDC), which is otherwise known as idiopathic Basal ganglia calcification, is a neurodegenerative disorder which is popularly known as Fahr’s Syndrome. A bilateral, symmetrical, intra cranial calcification characterizes Fahr’s disease with a predilection for the basal ganglia and the dentate nuclei. Because of the symmetrical involvement of these nuclei, the descriptive terminology, BSPDC, has been put forth [5].
This is a very rare disease of unknown prevalence. The typical age at the onset of the symptoms is 40-60 years. This is among the few inherited neurological conditions that lead to progressive dystonia Parkinsonism and neuropsychiatric manifestations.
The most common presentations as per the Fahr’s Disease Registry are movement disorders, which account for about 55% of the cases. Among these, Parkinsonism was seen in 57% cases, chorea was seen in 19% cases, tremor was seen in 8% cases, dystonia was seen in 8% cases, athetosis was seen in 5% cases and orofacial dyskinesia was seen in 3% cases. The other neurological manifestations include a cognitive impairment, cerebellar signs, speech disorders, pyramidal signs, psychiatric features, gait disorders and sensory changes [6]. The clinical diagnosis of Fahr’s disease is based on the combination of clinical features, brain imaging and on an exclusion of other causes of the intracranial calcification [7].
The imaging findings of the symmetric and extensive calcification are usually typical, as was seen in our case. The disorders of calcium metabolism may occur in association with the intracerebral calcification. Hypoparathyroidism,pseudohypoparathyroidism and hyperparathyroidism may be associated with the intracerebral calcification. Other causes of the intracranial calcification include infectious diseases like Toxoplasmosis and Syphilis and inflammatory illnesses like SLE. But Fahr’s disease represents a heterogeneous group of disorders that are not associated with any known disorder of the calcium metabolism [8].
Genetic studies have shown an autosomal dominant inheritance in the familial cases. A genetic heterogeneity and an anticipatory effect also have been observed. One multigenerational family with a linkage to the IBGC1 of chromosome 14 has been identified, but the causal gene is still unknown. The genetic studies which were done on other families did not replicate the result [9].
Benke et al., studied brain metabolism by using brain positron emission tomography with flurodeoxyglucose in a person with Fahr’s disease, who presented with a predominant frontal lobe syndrome and dementia. There was a massive reduction of the glucose metabolism in both the basal ganglia and the frontal lobes, which included the orbitofrontal and the anterior cingulate areas, which correlated with the clinical picture of disinhibition and a personality change [10].
Computed tomography scan remains the most effective screening tool. No prenatal or genetic tests are available for genetic counselling. The minimum age at which a negative CT scan can suggest the exclusion of the disease has not been established as yet. To clarify whether the disease is sporadic or familial, doing the imaging scan of the parents and other kindred is more reliable than their clinical screening [7].
The treatment targets include symptomatic support. The response to levodopa in those with Parkinsonian features is reportedly poor. Atypical antipsychotics are preferred for the psychiatric symptoms because of the coexistence of the extra pyramidal syndrome in these group of patients. The National Institute of Neurological Disorders and Stroke (NINDS) supports and conducts research on neurogenetic disorders such as Fahr’s disease. The goals of this research are to locate and understand the actions of the genes which are involved in this disorder. Finding these genes could lead to an effective method of treating and preventing Fahr’s syndrome.
[1]. Gülsün Murat, FuatBaykýz Ali, Kabata Serdar, Belli Hasan, Fahr’s Syndrome - Three cases presenting with psychiatric signsEur J Gen Med 2006 3(1):35-40. [Google Scholar]
[2]. Kotan D, Aygul R, Familial Fahr’s disease in a Turkish familySouth Med J 2009 102(1):85-86. [Google Scholar]
[3]. Billard C, Dulac O, Bouloche J, Echenne B, Lebon P, Motte J, Encephalopathy withcalcifications of the basal ganglia in children. A reappraisal of Fahr’s syndrome with respect to 14 new casesNeuropediatrics 1989 20(1):12-19. [Google Scholar]
[4]. Malik R, Pandya VK, Naik D, Fahr’s disease: A rare neurodegenerative disorderIndian J Radiol Imaging 2004 14:383-84. [Google Scholar]
[5]. Manyam BV, Bilateral strio-pallido-dentate calcinosis: a proposed classification of genetic and secondary causesMov Disord 1990 5(Suppl 1):94S [Google Scholar]
[6]. Manyam BV, Walters AS, Narla KR, Bilateral striopallido dentate calcinosis: clinical characteristics of patients seen in a registryMov Disord 2001 16(2):258-64. [Google Scholar]
[7]. Lam JS, Fong SY, Yiu GC, Wing YK, Fahr’s disease: a differential diagnosis of frontal lobe syndromeHong Kong Med J 2007 13(1):75-77. [Google Scholar]
[8]. Manyam BV, What is and what is not ‘Fahr’s disease’Parkinsonism Relat Disord 2005 11(2):73-80. [Google Scholar]
[9]. Geschwind DH, Loginov M, Stern JM, Identification of a locus on chromosome 14q .for idiopathic basal ganglia calcification (Fahr’s disease)Am J Hum Genet 1999 65(3):764-72. [Google Scholar]
[10]. Benke T, Karner E, Seppi K, Delazer M, Marksteiner J, Donnemiller E, Subacute dementia and imaging correlates in a case of Fahr’s diseaseJ Neurol Neurosurg Psychiatry 2004 75(8):1163-65. [Google Scholar]