The Appropriate DOTS Regimen Greatly Reduces the Disabilities in Polyarticular EPTB
Arvnd S. Pandey1, Ashish Surana2
1 Professor & Head, Department of TB & Respiratory Medicine, Surat Municipal Institute of Medical Education & Research (SMIMER), Surat, India.
2 Assistant Professor, Department of Microbiology, Surat Municipal Institute of Medical Education & Research (SMIMER), Surat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Ashish Surana, Department of Microbiology, SMIMER, Near Bombay Market, Umarwada, Surat, Gujarat, India.
Phone: 09426854701
E-mail: suranaan@yahoo.com
The placement of cases of Extrapulmonary Tuberculosis (EPTB) on the appropriate Directly Observed Treatment Short Course (DOTS) regimen remains a problematic issue in India and often, consultants delay this, leading to significant avoidable pain, discomfort and reduction in the quality of life of the patients. In contrast, a prompt institution of the DOTS regimen can regress such problems, even at a delayed stage. The following case report on polyarticular tuberculosis which involved the bilateral knee and ankle joints without a pulmonary or disseminated form of tuberculosis, amply highlights these facts.
Polyarticular Tuberculosis, EPTB, Dots Regimen
INTRODUCTION
Tuberculosis may develop in the skeletal system, apart from its primary location, the lungs. Osteoarticular tuberculosis is a quite uncommon form of extrapulmonary tuberculosis, with skeletal tuberculosis accounting for 1-5% of all the tuberculosis infections [1]. Mostly, the vertebra is affected in the skeletal system followed by the joints, the hips and the knees being the most common among the joints [2,3]. Skeletal tuberculosis is localized to a single site in 90-95% of the reported cases. A multifocal involvement is rare (0.05-0.1%) and it is usually associated with disseminated disease [4,5]. We are presenting a rare case of polyarticular tuberculosis without an obvious form of disseminated tuberculosis.
CASE REPORT
A 32-year-old female presented at the Outpatient Tuberculosis and Respiratory Diseases Department of our teaching hospital. The chief complaints were severe pain and swelling in the left knee, which restricted her daily activities. Since one year, the patient was on the Cat-I DOTS regimen. On physical examination, the patient was found to be in a poor general condition, crippled and anaemic. A local examination revealed a painful knee with swelling, increased temperature, effusion and a limited range of motion [Table/Fig-1]. The joint fluid aspiration was smear positive for Acid Fast Bacilli (AFB) and the culture and drug susceptibility which were assessed by the BacT/Alert method, demonstrated Mycobacterium tuberculosis on the 24th day of incubation, which was sensitive to all the primary anti-tubercular drugs i.e. Izoniazid, Rifampicin, Pyrazinamide, Streptomycin and Ethambutol. There was no significant present or past history of respiratory complaints and the X-ray of the chest was normal [Table/Fig-2].
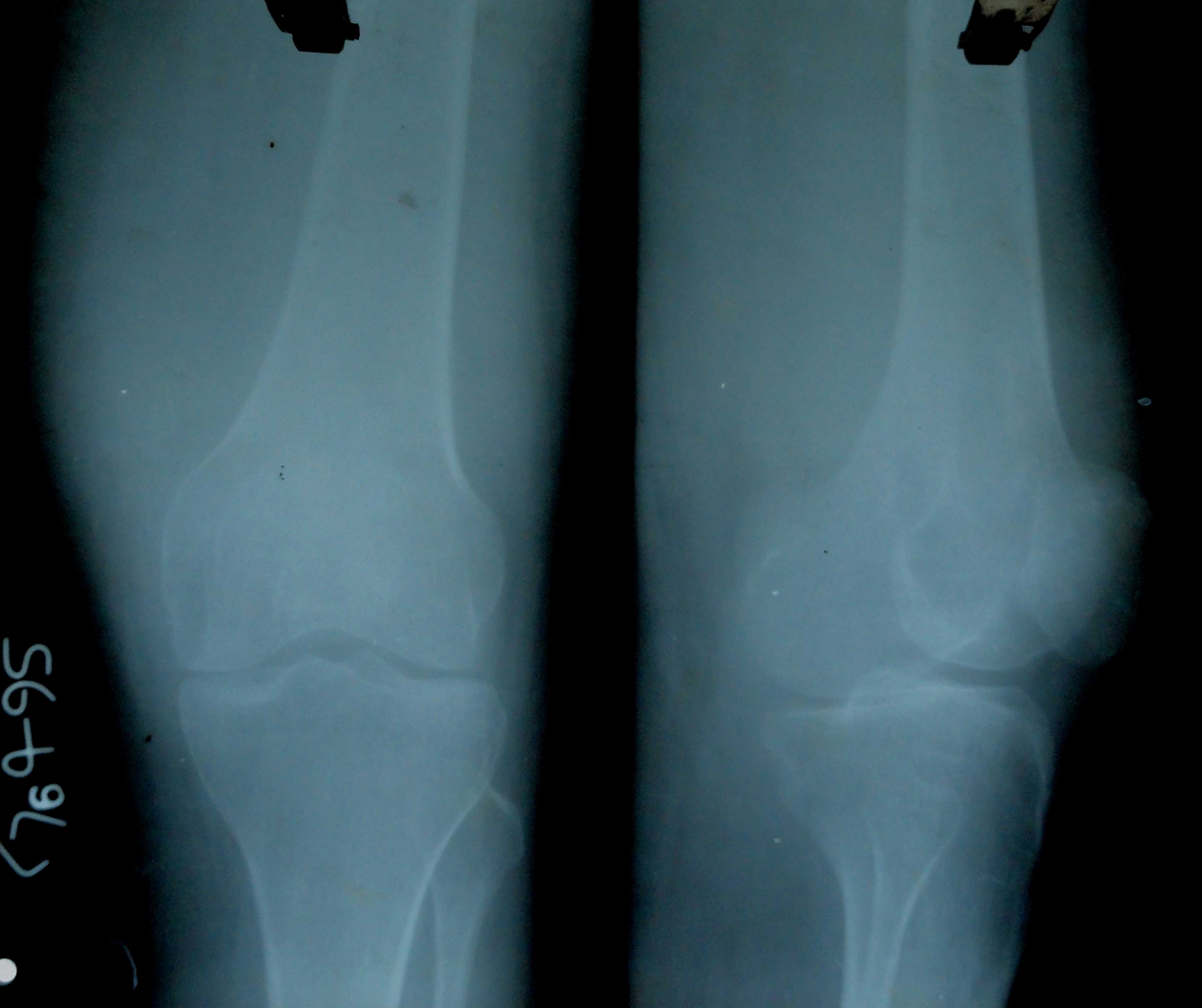
Anteroposterior and Lateral plain radiograph of left knee showing reduction in joint space along with significant soft tissue swelling
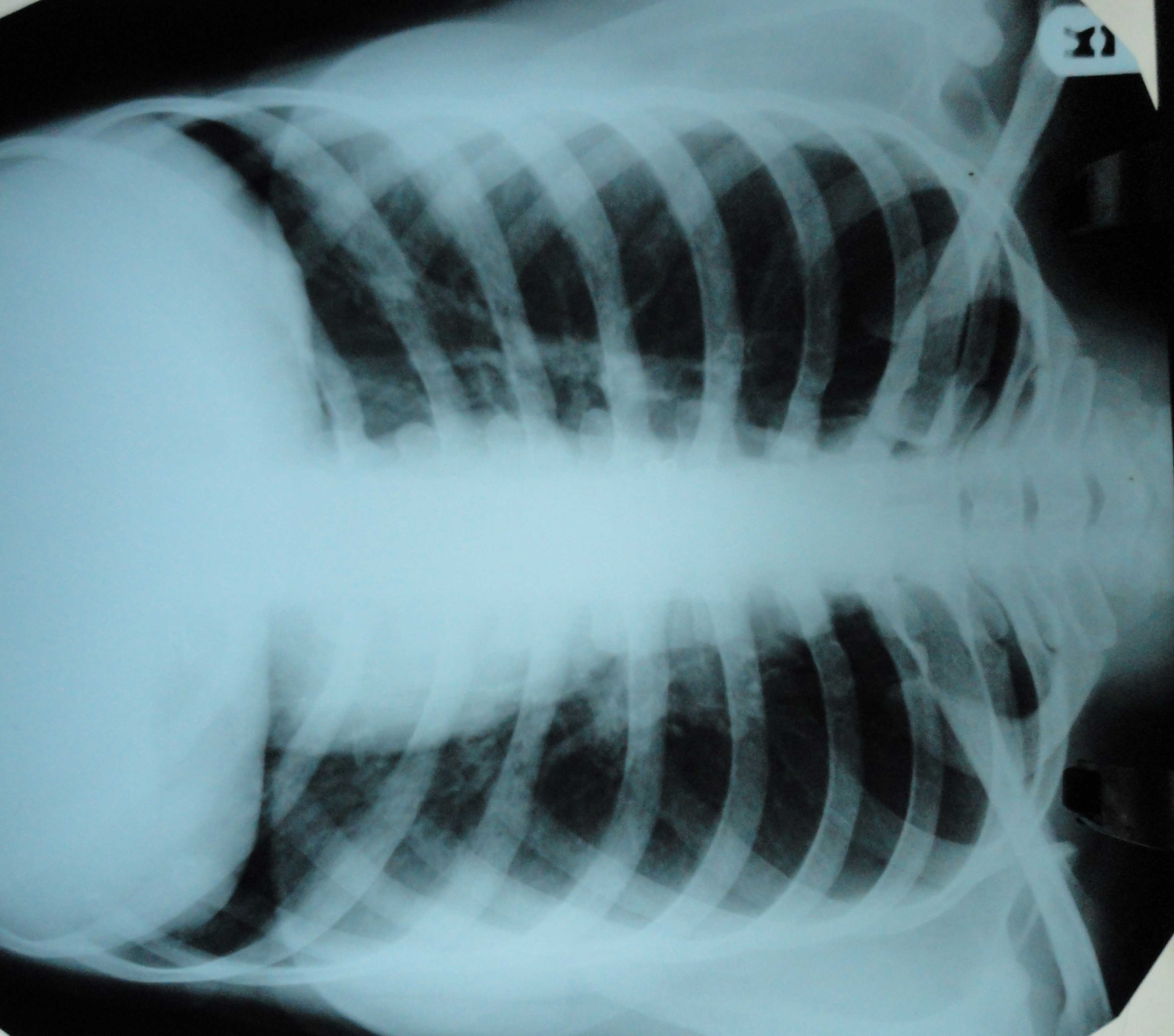
Posteroanterior plain radiograph of chest showing no significant abnormality
There was no history of alcohol ingestion, trauma, Diabetes mellitus or any other immunocompromised disease. The tests for the Human Immunodeficiency Virus (HIV) were repeatedly non-reactive.
Her past history revealed that she was well one and a half years ago, in April 2008, after which she developed fever and swelling in the right neck, for which she consulted a local doctor. One month later, on getting no relief and due to an additional complaint of pain and swelling in the left knee, the patient revisited the same doctor. Her laboratory examination revealed that her haemoglobin was 10.6 gm/dl, ESR was 98 mm in the first hour by the Westergren method and the tuberculin test showed a positive result of 20 millimetres. Fine needle aspiration cytology of the neck swelling revealed features which were suggestive of tuberculosis. Consequently, an unsupervised antitubercular regimen, consisting of Rifampicin, Isoniazid, Pyrazinamide and Ethambutol was started.
Despite 5 months of the treatment with antitubercular drugs, a progressive elevation of the ESR occurred, from 90 mm to 120 mm to 146 mm in the first hour. Though the neck swelling improved, the pain in the left knee continued, with the appearance of a swelling in left ankle, making her bed ridden [Table/Fig-3]. Six weeks later, in December 2008, there was an appearance of swelling and pain in the right knee also, for which the patient was referred to the Orthopaedics Department of a tertiary government hospital, where incision and drainage (I and D) of the swellings of the right knee and the left ankle was done. The histopathology report revealed features of tuberculosis. The patient was placed on the Cat-I DOTS regimen.
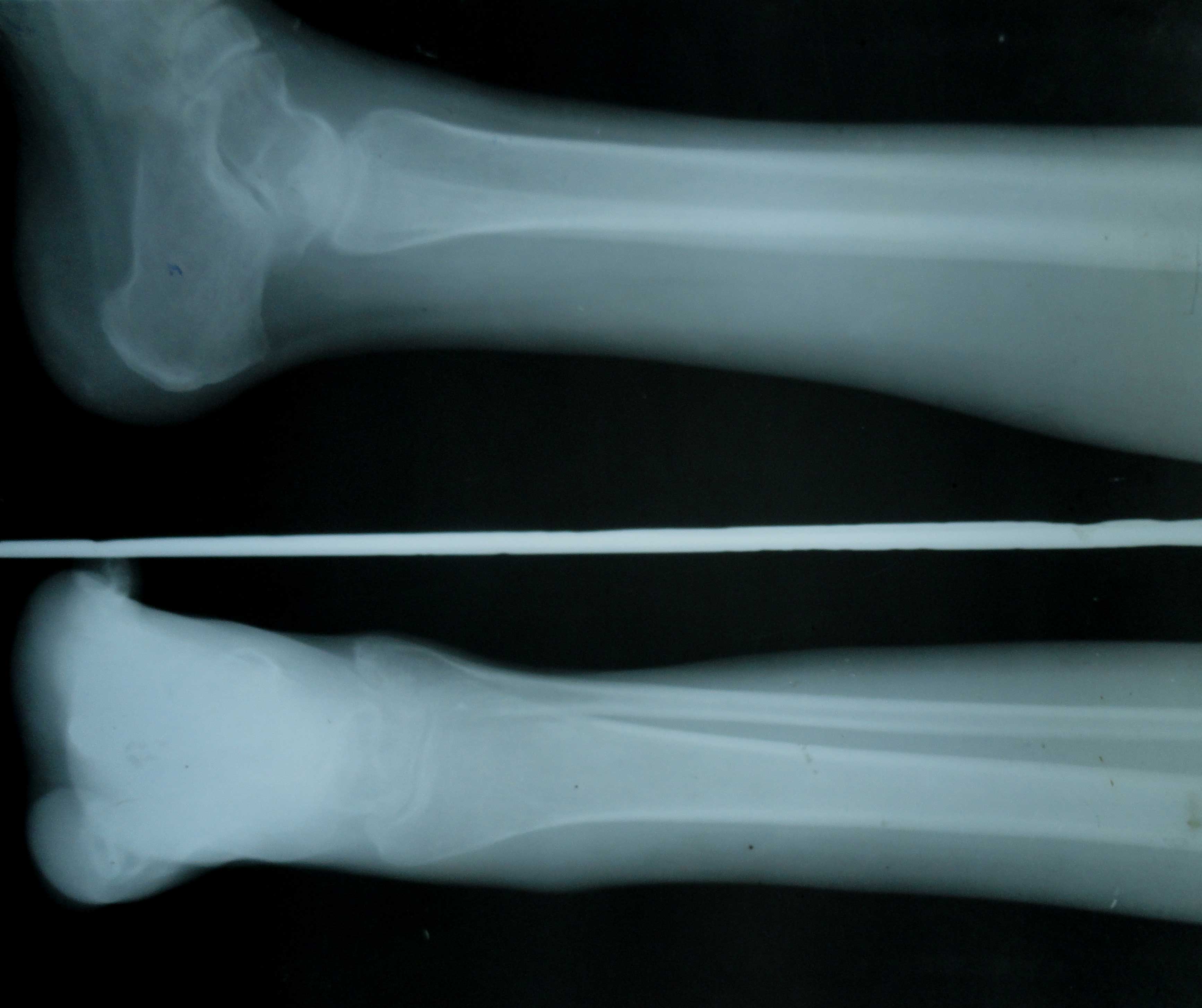
Anteroposterior plain radiograph of both ankle joints showing reduction in joint space, reduction in bone density along with significant soft tissue swelling

About one and a half months later, a swelling and pain appeared in the right ankle. I and D of the right ankle was done. The histopathology report was suggestive of tuberculosis. The Cat-I DOTS regimen was continued. As her complaints remained unabated, the patient sought care in December 2009, at our department. Considering her past history and the persistence of the swelling and pain in the left knee, the patient was labelled as a treatment failure case, as per the Revised National Tuberculosis Control Programme (RNTCP) guidelines [6] and she was placed on the Cat-II regimen.
After being for about 6 months on the Cat-II regimen, the patient started walking with a mild limp. At present, as in December 2010, the patient is on a continuous phase of the Cat-II regimen and she can walk normally; her ESR is 11 mm in the first hour. The latest X-ray of her knee and ankle joints shows mild sclerosis [Table/Fig-4 & 5].
Post-treatment Anteroposterior plain radiograph of both knee joints showing normal bony structures with mild reduction in joint space and no soft tissue swelling

Post-treatment Anteroposterior and Lateral plain radiograph of ankle joint showing normal bony structures
DISCUSSION
Multifocal osteoarticular tuberculosis which involves the knee and ankle, is an uncommon presentation of skeletal tuberculosis. The uncommon site, a lack of awareness and the ability to mimic other disorders clinically and on radiographs, lead to diagnostic and therapeutic delays, sometimes with devastating consequences for the patients [1,7]. Despite the widespread osteoarticular involvement, the outcome of the patient was favourable after the medical management as per RNTCP guidelines, leading to an excellent healing and limited residual disabilities.
The treatment of extrapulmonary tuberculosis under RNTCP is consistent with the international recommendations which have been made by the WHO and the International Union Against Tuberculosis and Lung Disease (IUATLD) [8,9]. The categorization is done according to the history, clinical and diagnostic criteria. All the RNTCP regimens are given thrice weekly. The RNTCP Category I regimen consists of two months of Isoniazid, Rifampicin, Pyrazinamide and Ethambutol, which are given under the direct observation of a DOT provider. This two-month intensive phase is followed by a four-month continuation phase of the treatment with Isoniazid, Rifampicin and Pyrazinamide, where at least the first of the thrice-weekly doses is given under the direct observation of a DOT provider. In Category II, Streptomycin is added to the two months of intensive phase, followed by a one-month course of Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. This is followed by the continuation phase of the treatment with Isoniazid, Rifampicin and Ethambutol for five months.
This case report reveals two important observations. Firstly, the patient was not placed on the DOTS regimen, which is provided free of cost to all the tuberculosis patients by the Government of India through RNTCP. The DOTS regimen plays a pivotal role in checking the concealed irregularities which are often seen in the patients who are on a non-DOTS antitubercular therapy, thereby ensuring high cure rates. Secondly, this patient continued to be treated inappropriately by the Cat I regimen for more than a year. Ideally, this patient should have been labelled as a treatment failure case as per the RNTCP guidelines [6] and switched on to the Cat II regimen, after five months of the antitubercular treatment with no clinical improvement and positive laboratory findings for tuberculosis. This is further exemplified by the fact that the subsequent placement on the appropriate Cat II regimen led to amelioration of her complaints.
These observations point out the need to guarantee that all the tuberculosis patients are placed on the appropriate DOTS regimen, both in the private and public sectors and to ensure this, the inevitable role of the RNTCP modular trainings cannot be overemphasized, which should form an integral part of the curriculum of the medical graduates.
[1]. Bajracharya S, Nepal P, Singh MP, Singh GK, Polyarticular tuberculosis in a young boy: A rare presentationKathmandu University Medical Journal 2007 5(1)(17):112-13. [Google Scholar]
[2]. Hoffman EB, Campbell JA, Lee AS, Tuberculosis of the hip and knee in childrenS Afr Bone Joint Surg 1995 1:24-28. [Google Scholar]
[3]. Silva JF, A review of patients with skeletal tuberculosis treated at the University Hospital, Kuala LumpurInt Orthop 1980 4:79-81. [Google Scholar]
[4]. Kaya A, Topu Z, Fitoz S, Numanoglu N, Pulmonary tuberculosis with multifocal skeletal involvementMonaldi Arch Chest Dis 2004 Apr-Jun 61(2):133-35. [Google Scholar]
[5]. Shah BA, Splain S, Multifocal osteoarticular tuberculosisOrthopedics 2005 Mar 28(3):329-32. [Google Scholar]
[6]. Revised National Tuberculosis Control Programme, DOTS Plus Guidelines, Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, January. 2010 ; 15-21 [Google Scholar]
[7]. Dhillon M S, Nagi O N, Tuberculosis of the Foot and AnkleClinical Orthopaedics and Related Research May 2002 398:107-13. [Google Scholar]
[8]. World Health Organization (WHO)Treatment of TuberculosisGuidelines for National Programmes 2003 3rd(WHO/CDS/TB, 2003.313)Geneva, SwitzerlandWHO [Google Scholar]
[9]. International Union Against Tuberculosis and Lung Disease (IUATLD)Management of tuberculosis: a guide for low-income countries 2000 5thParisIUATLD [Google Scholar]