Bone Marrow Necrosis (BMN) is regarded as a rare entity in the aspirates and the trephine biopsies which are obtained from living patients and it is a rare antemortem diagnosis. Usually, BMN is associated with a poor prognosis and it has a 90% association with malignancies (mainly haematological). Its other causes include infections, drugs and other non malignant haematological causes. BMN which occurs due to unknown causes (idiopathic), is very rare. The present case report describes a case of BMN in a 14 year old male child from rural background, who came to the medicine outpatient department of a tertiary care centre in north India, with the complaints of generalized weakness, severe bone pains, especially in the ribcage area and fatigue. His peripheral blood film revealed pancytopaenia. His bone marrow aspiration yielded a watery, sero-sanguinous fluid from 2 different sites. Microscopy revealed “ghost like” haematopoietic cells lying in eosinophilic, proteinaceous material. Bone marrow biopsies from both the sites revealed extensive foci of gelatinous transformation and necrosis.
A diagnosis of BMN was rendered. No underlying neoplastic / non neoplastic cause was identified, even after a thorough systematic investigation (haematological/biochemical/ radiological and immunological). Thus, a final diagnosis of BMN due to an idiopathic cause, was finally given. The patient was given supportive treatment, after which he was referred to a higher centre. BMN which arises idiopathically is usually very rare and often precedes the aetiological diagnosis and obscures the diagnosis. Traditionally, the prognoses of the patients with BMN were considered as poor, but with better treatment aids (chemotherapy and supportive treatment), the prognoses of these patients have been found to improve. Vigorous supportive care, along with a disease specific treatment, is the key to its management. This case was worth reporting, as no cause of BMN was elicited in it and we have summarized the signs and symptoms, the associations, haematological and other lab investigations and the role of radiology, which helped in its diagnosis.
INTRODUCTION
Bone Marrow Necrosis (BMN) is regarded as a rare entity in the aspirates and the trephine biopsies which are obtained from living patients and it is a rare antemortem diagnosis [1–5].
Although it is an example of a bone marrow stromal reaction, bone marrow necrosis, if it is present, is significant, as it indicates a poor prognosis and points towards an underlying disease pathology (malignancy-haematological/ solid, infections, drugs and other non malignant haematological causes). BMN which occurs due to unknown causes (idiopathic) is very rare.
Often, the extensive necrosis can obscure the cellular elements, leading to a non-diagnosis [5] and it can also precede the disease pathology [5–7] before its presentation, which can lead to much confusion in the diagnosis.
The present case report has described a case of a 14 year old male who was diagnosed as having BMN, with no underlying neoplastic / non neoplastic cause, even after a thorough systematic investigation, who responded partially to the supportive care management.
CASE REPORT
A 14 years old male child from a rural background, came to the medicine outpatient department of a tertiary care centre in north India with the complaints of a generalized weakness, severe bone pains, especially in the ribcage area and fatigue. On clinical examination, pallor was noted and the patient was advised to undergo a haematological investigation, which revealed pancytopaenia with low haemoglobin (5.1gm/dl), leucopeania (3900 cells/ cu mm) and thrombocytopaenia (82,000/cu.mm). The attendants of the child said that he was prescribed haematinics by a local general practitioner, on the basis of his pallor, fatigue and a haemoglobin report of 8.5 gm/dl, 4 months back. During the next 4 months, his haemoglobin levels fell steadily, which prompted his guardians to visit our tertiary care unit. The patient was examined, where apart from sternal tenderness and pallor; no lymphadenopathy or organomegaly was noted.
In view of the above findings a bone marrow aspiration was planned. The aspiration was done from the right posterior superior iliac spine (PSIS), following all the aseptic measures. On aspiration, the aspirate was found to be of an altered sero-sanguinous type. Slides were prepared, but in view of the nature of the aspirate, a reaspiration was planned from the left PSIS. This time also, a watery, dark red to clear fluid was aspirated.
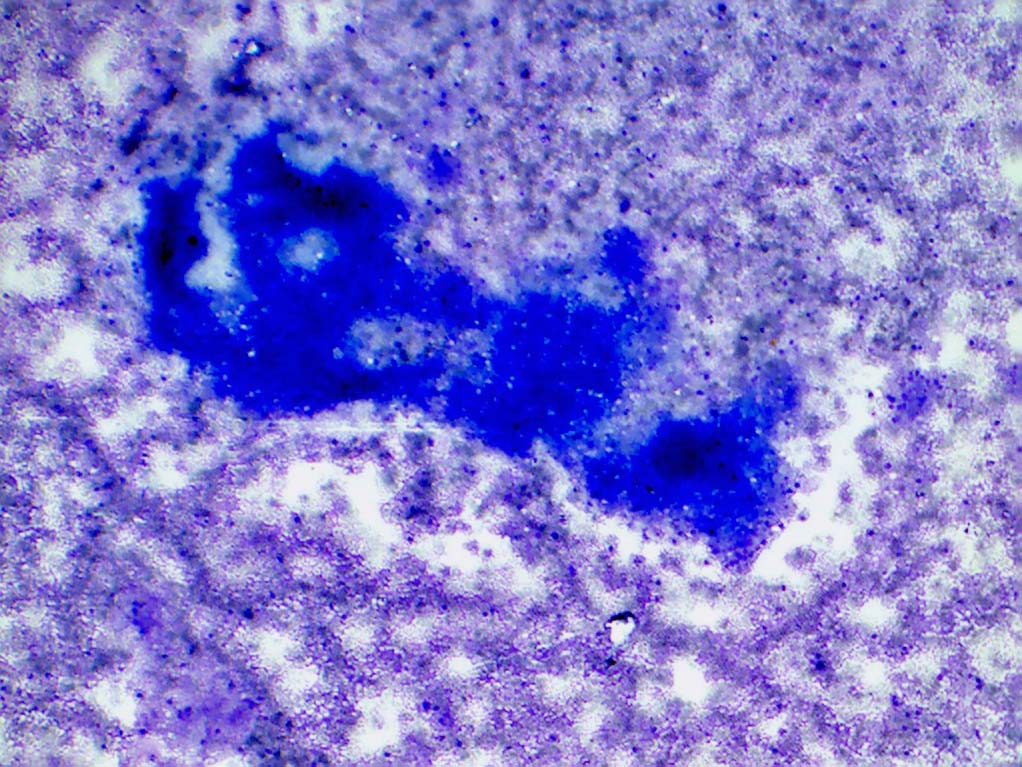
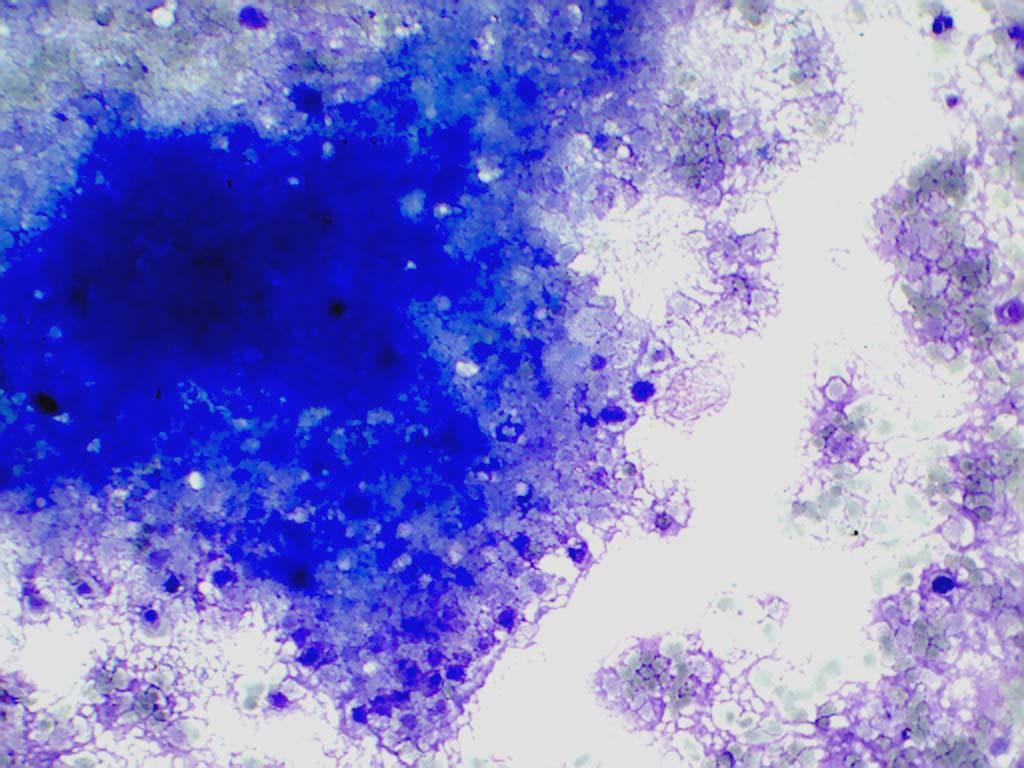
The smears were air dried and they were subsequently stained with May Grunwald Giemsa (MGG), which revealed a differential, irregular staining with the presence of an amorphous eosinophilic proteinaceous material; enmeshed within which were seen “ghost like” haematopoietic cells with irregular or indistinct cell membranes and with the nuclei showing the nuclear features which were associated with necrosis [Table/Fig-1] and [Table/Fig-2].
Irregular staining with presence of amorphous proteinaceous material; enmeshed within which were seen “ghost like” hematopoietic cells with irregular or indistinct cell membrane and the nuclei showing the nuclear features associated with necrosis. (MGG 100X)
Higher Magnification emphasizing on “ghost like” hematopoietic cells. (MGG 400X)
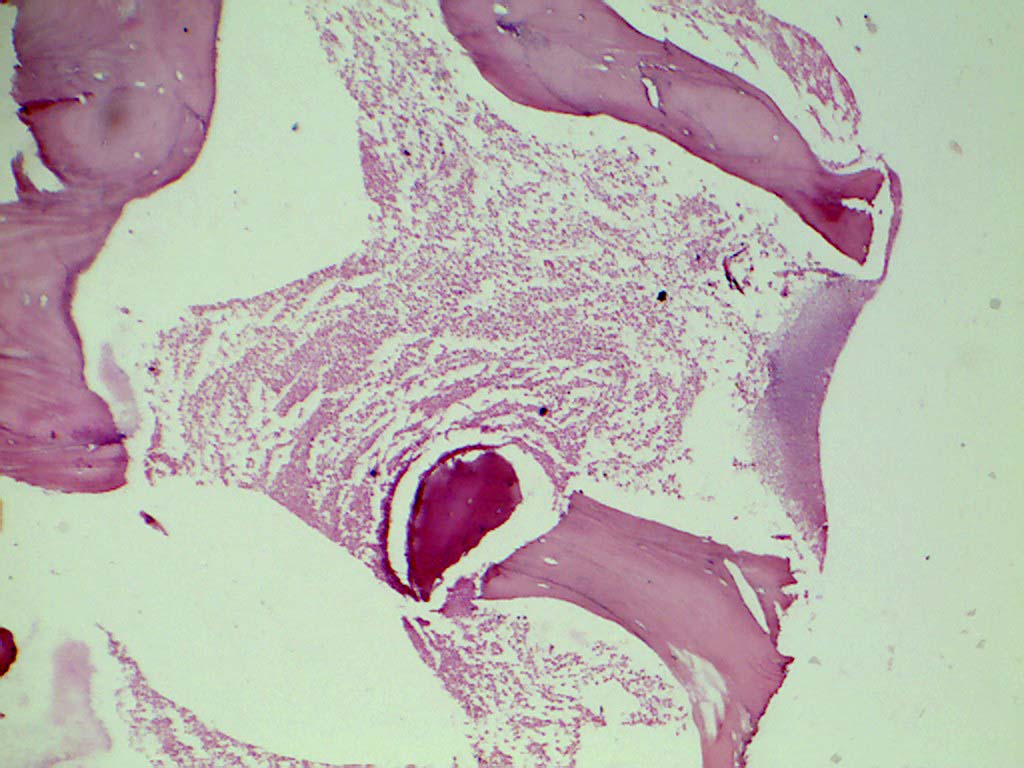
Bone marrow biopsies which were obtained from both the sites revealed extensive foci of gelatinous transformation with necrosis. No increase in the number of fat cells or destruction of the bony trabeculae were noted. The individual cells which surrounded the eosinophillic gelatinous material were heaped up at the periphery in the form of a cellular debris, with the cells exhibiting a similar morphology as that which was noted in the aspiration smears. [Table/Fig-3]. Based on these findings, a diagnosis of BMN was rendered. Following this, an extensive radiological, biochemical and serological work-up was taken up.
Section shows disruption of the normal bone marrow architecture with a considerable loss of fat spaces with necrotizing hematopoietic cells. (H & E 200 X)
Biochemically, apart from an elevated alkaline phosphatase, the rest of the biochemical parameters were within the normal range, which included normal serum calcium, uric acid and lactate dehydrogenase.
The chest X-ray, ultrasonography of the abdomen and the Computed Tomographic (CT) scans were unremarkable. On Magnetic Resonance Imaging (MRI), changes in the bone marrow signal intensities were observed at many places, which owed to the change in proportions of the fat and water, which were significant when BMN was diagnosed on the basis of the trephine biopsy. Serologicaly, all the viral markers (including hepatitis) and other important markers of an infectious aetiology were negative. The patient’s ESR was elevated; however, it was not associated with the reactive tuberculin test.
No significant drug intake history was elicited. However, an inadvertant exposure to an agricultural insecticide in the past could not be comprehensively ruled out. In view of the consistent absence of any underlying malignant or non-malignant disorder, the patient was diagnosed as a case of BMN which had an idiopathic aetiology.
A supportive therapy was planned and it was decided that a haematopoietic support would be provided to the patient by the means of blood transfusions (with PRBCs), with the administration of FFPs or platelet transfusions, as and when required. The patient and his guardians were educated about the importance of hydration, the principles of asepsis and the hazards of agricultural toxins as occupational hazards. The patient was discharged and he was referred to a higher referral centre.
DISCUSSION
BMN, as a separate and a distinct clinic-pathologic entity, is relatively unknown and unrecognized; although it was described for the first time 7 decades ago by Wade and Stevenson in 1942 [8], in a patient of sickle disease, who had died of cerebral infarction. The incidence of BMN is reported to be in range of 0.37% to 6.5% [3, 4, 9].
BMN is best defined as “necrosis of the myeloid issue and the medullary stroma in large areas of the haematopoietic bone marrow” [10]. On trephine biopsies, BMN is characterized by a disruption of the normal bone marrow architecture, with a considerable loss of the fat spaces. This contrasts the findings of aplastic anaemia, in which there is loss of myeloid tissue and no destruction of the reticular structure. In contrast to the aseptic necrosis, there is no destruction of the spicular architecture [10]. Various researchers have defined and have tried to grade BMN, based on their own individual parameters.
The failure of a micro-circulation (immunological, inflammatory or mechanical) of the marrow plays a central role in its pathophysiology [10].This includes a decreased oxygen tension which is due to the increased proliferative capacity of the infiltrating malignant cells [3], the toxic effects of chemotherapy, a micro-vascular infarction, tumour necrosis factor α (TNF-α) and thrombosis [3, 4].
BMN is most often noted at post-mortem and mostly in the patients who suffer from haematological and other malignancies, who are on chemotherapy or are suffering from vaso-occlusive events. It is also associated with some non malignant conditions such as infections, sepsis, pneumonia and the HIV infection. Certain pharmaceutical agents such as sulfasalazine, interferon, trans retinoic acid and fludarabine are amongst the aetiological agents [9, 10]. BMN also has association with hyperparathyroidism, anorexia, anti-phospholipids and haemolytic uraemic syndromes and with a diffuse intravascular coagulation. BMN which arises idiopathically, as in the present case report, is usually very rare; often, BMN precedes the aetiological diagnosis and obscures the diagnosis. Multiple sites and repeated aspirations and biopsies are recommended in all such cases to reach a diagnosis [9].
The symptoms of BMN include bone pain (the commonest and an important diagnostic sign) and episodes of fever which are related to anaemia and thrombocytopaenia (peticheal spots). Embolic episodes, though rare, have also been reported and they are associated with high mortality rates [11].
Haematologically, BMN is associated with pancytopaenia and in some cases, with a leukoerytheroblastic picture [2–4]. The biochemical lab investigations often reveal elevated lactic dehydrogenase, alkaline phosphatase, uric acid and glutamic oxaloacetic transaminase levels. Other than aspirations and biopsies; bone marrow scintiography and magnetic resonance imaging provide the alternate, non invasive methods of diagnosis [12].
Traditionally, the prognoses of the patients with BMN were considered to be poor (especially in children with acute leukaemia; the median survival being 4-13 months); but the outcomes in the cases of BMN are age and aetiology-dependant. With better treatment aids, chemotherapy and supportive treatment, the prognoses of these patients are improving, which can lead to a complete recovery [13, 14]. Vigorous supportive care, along with a disease specific treatment, is the key to its management. Packed RBCs with platelet concentrates are provided to tide over the cytopaenias, so that adequate time is provided for the spontaneous recovery of the haematopoietic cells. Antibiotics, chemotherapy and proper hydration can be employed, wherever necessary. The newer modalities include the usage of cytokines and other such neo-adjvants and the employment of adjusted low toxic chemotherapeutic agents which are less toxic to the bone marrow stem cells and the stroma [15].
The BMN class comprises of a large cohort of patients who have characteristic clinical features and are under-recognized by the medical fraternity. Their problems are compounded further by the fact that its aetio-pathogenesis, factors and subsequent management protocols are highly under reported in the medical literature. This case was worth reporting as no cause of BMN was elicited in it and we have summarized the signs and symptoms, the associations, haematological and other lab investigations and the role of radiology, which helped in its diagnosis.
CONCLUSION
Bone Marrow Necrosis (BMN)- “necrosis of the myeloid issue and the medullary stroma in large areas of the haematopoietic bone marrow”, is a rare antemortem diagnosis and it is mostly associated with malignancies (especially haematological).
The aspirates, in cases of BMN, are watery and sero-sanguinous and the smears reveal a differential, irregular staining with the presence of amorphous eosinophilic proteinaceous material; which is enmeshed within which were seen as “ghost like” haematopoietic cells with irregular or indistinct cell membranes and with the nuclei showing the nuclear features which were associated with necrosis.
A BMN biopsy is characterized by a disruption of the normal bone marrow architecture, with a considerable loss of the fat spaces. This contrasts the findings of aplastic anaemia, in which there is loss of myeloid tissue and no destruction of the reticular structure. In contrast to the aseptic necrosis, there is no destruction of the spicular architecture.
BMN which arises idiopathically, as in the present case report, is usually very rare; often, BMN precedes the aetiological diagnosis and obscures the diagnosis. Multiple sites and repeated aspirations and biopsies are recommended in all such cases to reach a diagnosis.
Presently, the outcomes in the cases of BMN are considered age and aetiology-dependant. With better treatment aids, chemotherapy and supportive treatment, the prognoses of these patients are improving, which can result in a complete recovery.
[1]. Kiraly JF, Wheby MS, Bone marrow necrosisAm J Med 1976 60:361-68. [Google Scholar]
[2]. Ranaghan L, Morris TCM, Desai ZR, Markey GM, Bone marrow necrosisAm J Hematol 1994 47:225-28. [Google Scholar]
[3]. Markovic SN, Phyliky RL, Li CY, Pancytopenia due to bone marrow necrosis in acute myelogenous leukemia: role of reactive CD8 cellsAm J Hematol 1998 59:74 [Google Scholar]
[4]. Al-Gwaiz LA, Bone marrow necrosisAnn Saudi Med 1997 17:374-76. [Google Scholar]
[5]. Granot H, Polliack A, Matzner Y, Bone marrow necrosis as the only manifestation of disseminated carcinomatosisActa Hematol 1980 64:232-35. [Google Scholar]
[6]. Majumdar G, Massive bone marrow necrosis as the presenting feature in a case of primary bone marrow high-grade non-Hodgkin’s lymphomaLeuk Lymph 1997 26:409-12. [Google Scholar]
[7]. Niebrugge DJ, Benjamin DR, Bone marrow necrosis preceding acute lymphoblastic leukemia in childhoodCancer 1983 52:2162-64. [Google Scholar]
[8]. Wade L, Stevenson L, Necrosis of bone marrow with fat embolism in sickle cell anaemiaAm J Path 1941 17:47-54. [Google Scholar]
[9]. Bashwari L, Satti MB, Bone marrow necrosis: report of five cases and review of literatureAnnals Saudi Med 2000 20(1):78-82. [Google Scholar]
[10]. Janssens AM, Offner FC, Van Hove WZ, Bone marrow necrosisCancer 2000 88:1769-80. [Google Scholar]
[11]. Garza JA, Massive fat and necrotic bone marrow embolization in previously undiagnosed case of sickle cell diseaseAm J Forensic Med Pathol 1990 11:83-88. [Google Scholar]
[12]. Weissman DE, Negendank WG, Al-Katib AM, Smith MR, Bone marrow necrosis in lymphoma studied by magnetic resonance imagingAm J Hematol 1992 40:42-46. [Google Scholar]
[13]. Khan AM, Yamase H, Tutschka PJ, Bilgram S, Autologous peripheral blood progenitor cell transplantation for non-Hodgkin’s lymphoma with extensive bone marrow necrosisBone Marrow Transplant 1997 19:1037:39 [Google Scholar]
[14]. Sporn JR, Fallon MA, Recovery from widespread bone marrow necrosis occurring after chemotherapy for adult monocytic leukemiaMed Pediatr Oncol 1992 20:224-26. [Google Scholar]
[15]. Knupp C, Pekala PH, Cornelius P, Extensive bone marrow necrosis in patients with cancer and tumor necrosis factor activity in plasmaAm J Hematol 1988 29:215-21. [Google Scholar]