A Case Report of a Spontaneous Oesophageal Pleural Fistula
Sanjeev Kumar1, Arshdeep Singh2, Prithpal S Matreja3, Sanjiv Kumar Kler4
1 Assistant Professor, Department of Pulmonary Medicine, Dr Rajinder, Prasad Government Medical College, Kangra, Tanda, 1760011, India.
2 Associate Professor, Department of Radiodiagnosis, Gian Sagar Medical College, Ram Nagar, Rajpura, Patiala, 1406012, India.
3 Associate Professor, Department of Pharmacology, Gian Sagar Medical College, Ram Nagar, Rajpura, Patiala 1406013, India.
4 Assistant Professor, Department of Medicine, Gian Sagar Medical College, Ram Nagar, Rajpura, Patiala 1406014.
NAME, ADRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prithpal Singh Matreja, Associate Professor, Department of Pharmacology, Gian Sagar Medical College and Hospital, Ramnagar, Patiala, India.
Phone: +91-9855001847, +91-1762-507118 Fax: +91-1762-520024
E-mail: drpsmatreja@yahoo.co.in
We are reporting a case of an asthmatic patient who presented to us with retrosternal chest pain, constipation, and shortness of breath, with features which were suggestive of a hydropneumothorax and shock. On recovery from the shock, the patient was found to have increased chest tube drainage, which was suggestive of an oesophageal rupture. The Computerized Tomography (CT) scan showed a fistulous track. The patient was diagnosed as a case of a spontaneous oesophageal pleural fistula (Spontaneous EPF) on the basis of her clinical and radiological findings.
Asthma, Shock, Oesophageal pleural fistula, Rupture
INTRODUCTION
An Oesophageal Pleural Fistula (EPF) is very uncommon and it is formed secondary to an instrumentation, a malignancy, a surgery or a postpneumectomy complication [1]. It is associated with high morbidity and mortality because of the ensuing empyema and the nutritional debilitation [2]. Spontaneous oesophageal pleural fistulae have very rarely been reported. We are reporting the case of a patient who presented with the complaints of vague pain in the retrosternal region and the upper abdomen, with shortness of breath. Later, the patient went into shock; her chest radiograph was suggestive of a hydropneumothorax. An Intercostals Chest Tube Drainage (ICTD) was done; the patient recovered from the shock and was allowed oral intake. When she was allowed oral intake, the chest tube drainage increased significantly. A gastrograffin study and computed tomography (CT) of the chest revealed a fistulous track in the lower one third of the oesophagus. Contrast enhanced computed tomography is useful in evaluating oesophageal pleural fistulae [1]. A brief review of the imaging findings and the management of EPF has been discussed.
CASE REPORT
A 60 year old female patient, a known case of psoriasis and bronchial asthma; who was maintained on oral corticosteroids, presented with the complaint of a vague pain in the chest and the upper abdomen, which was associated with constipation and breathlessness for 2 days. The pain was dull in nature, it was located in the retrosternal area and it was continuously radiating to the upper abdomen. It was not associated with nausea or vomiting. But, her oral intake had been inadequate for the last 3-4 days before her admission. She had passed stools prior to the day of her admission. On examination, her abdomen was found to be soft; on per rectal examination, faeces were felt. The pain was associated with shortness of breath; and there was no history of upper gastrointestinal endoscopy, instrumentation or surgery. On the evening of her admission, the patient felt a progressive shortness of breath and her Blood Pressure (BP) and pulse were not recordable; she was put on a ventilator, along with an inotropic support.
Her chest examination revealed a markedly reduced air entry in the left hemi thorax with a hyper resonant percussion note anteriorly. Her chest radiograph showed a right sided pleural effusion. An intercostal chest tube drainage was inserted, which drained 1.2 liters of fluid with flakes of pus; within 6 hours of the ICTD insertion, the inotropic support was slowly weaned off and her blood pressure and pulse returned to normal. When she was allowed to take per orally, it was noticed that the drainage volume was increasing significantly. So an EPF was suspected clinically. A gastrograffin study and her chest radiograph revealed a fistulous track at the mid thoracic region, which was going up to the left pleural cavity [Table/Fig-1].
Chest radiograph showing a fistulous tract in the lower one-third of the esophagus at the mid-thoracic region going up to left pleural cavity
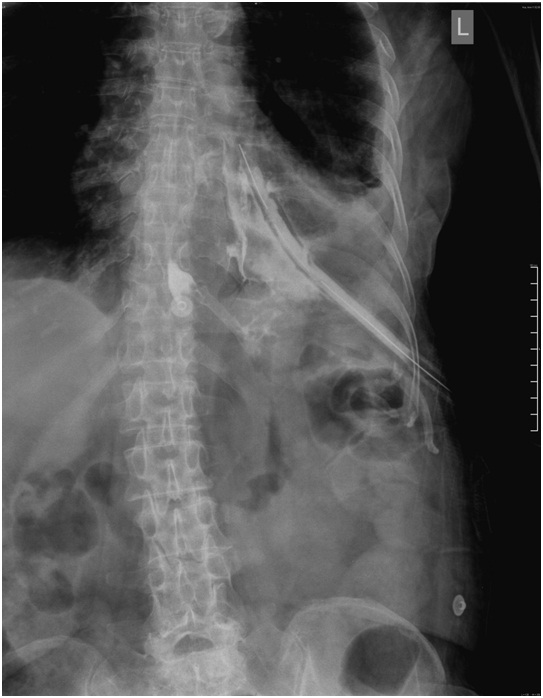
The gastrograffin study and the CT scan showed a fistulous tract in the lower one-third of the oesophagus, at the mid-thoracic region, which was going up to the left pleural cavity, which was suggestive of an EPF [Table/Fig-2 & 3].
CT Scan (Coronal Section) showing a fistulous tract in the lower one-third of the esophagus at the mid-thoracic region going up to left pleural cavity (Arrow)

CT scan (Axial Section) showing a fistulous tract in the lower one-third of the esophagus at the mid-thoracic region going up to left pleural cavity (Arrow)
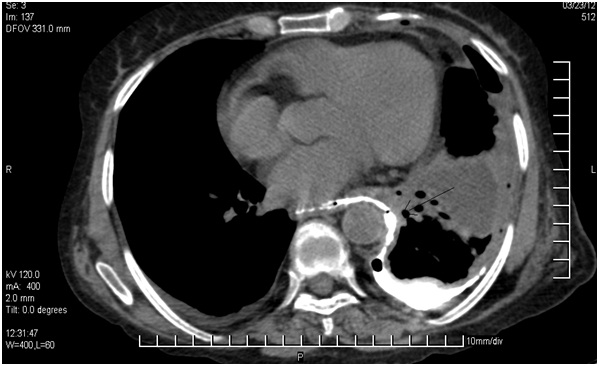
Though in the initial radiograph, on the day of admission, there was some evidence of mediastinitis, the post procedure radiograph and CT scan showed no evidence of mediastinitis or a hilar/mediastinal lymphadenopathy. While going through the previous records and CT of the abdomen, an oesophageal wall thickening was found to be present at the junction of the middle and lower third of the oesophagus.
This was previously reported when the patient was admitted to the hospital with psoriasis. The perforation was sealed and it was managed conservatively. An EPF is a rare entity and so, when either the drainage fluid contains food particles or when a persistent large volume of chest tube drain is seen, it should alert the treating physician towards getting a radiological confirmation. A contrast gastrograffin study or contrast enhanced CT scans are crucial for an early diagnosis and treatment.
DISCUSSION
An oesophageal pleural fistula is an uncommon entity and it is reported as a complication of an iatrogenic trauma or postpneumectomy [1]. The clinical signs and symptoms of an EPF are inconsistent and non specific, which include lassitude, chest pain, fever, dyspnoea and hypotension. The additional symptoms of dysphagia, odynophagia or a foul smelling regurgitation suggest the possibility of an EPF [2–4]. In the patients who complain of these non specific signs and symptoms post an oesophageal instrumentation or surgery, the possibility of an oesophageal trauma should be excluded [4]. The diagnosis of an EPF is made clinically and it has to be confirmed by various imaging modalities [1]. The radiological signs are also non specific and are dependent on the site, duration and the severity of the perforation [1,4].
The radiographic findings may not appear for up to 24 hours and if the pleura are intact, mediastinal emphysema occurs, with a mediastinal widening,within several hours. The mediastinitis could further lead to mediastinal pleura, hydrothorax or pneumothorax. On the rupture of the pleura, the mediastinum is spared and an oesophageal pleural fistula occurs because of the decompression of the oesophageal content into the pleura spaces. The radiographic picture could be of a pleural effusion, a pneumothorax or a hydrothorax. An EPF must be differentiated from aspiration pneumonia, a lung abscess, pulmonary emboli and a bronchopleural fistula [1,4]. The presentation of a pneuomediastinum or a subcutaneous emphysema may be seen in the later stages if the mediastinal pressure is less than the pleural pressure [1].
A CT scan confirms the radiological findings and it differentiates the pleural disease form the pulmonary disease [1]. A pleural effusion is seen in a majority of the patients and the presence of a pneumothorax reduces the diagnostic consideration [4]. The contrast media which are given orally and are seen in the pleural space, are pathognomonic of this uncommon disease [1, 2,4].
CT scan is also helpful in the management of this disease condition and the prognosis depends on the extent of the mediastinal involvement [1]. The management of an EPF depends on the size, site, duration and the severity of the perforation. We prefer local irrigation, antibiotics and an intracaval high calorie nutrition. This conservative therapy should as soon as possible, be followed by the direct reconstruction of the oesophageal wall [3].
To conclude, the presence of food particles or gastric contents in the pleural space confirms the diagnosis of an EPF. CT scan can confirm the diagnosis and detect the presence of mediastinitis, as the mediastinal involvement has a severe clinical course and as it responds to surgery. The diagnosis should be confirmed, so as to better manage the patient and to prevent the morbidity and the mortality which are associated with it.
[1]. Vyas S, Prakash M, Kaman L, Bhardwaj N, Khandelwal N, Spontaneous esophageal-pleural fistulaLung India 2011 28:300-02. [Google Scholar]
[2]. Liu PS, Levine MS, Torigian DA, Esophagopleural fistula sceonadry to esophageal wall ballooning and thinning after pneumonectomy: Findings of Chest CT and EsophagographyAJR 2006 186:1627-29. [Google Scholar]
[3]. Van Den Bosch JMM, Swierenga J, Gelissen HJ, Laros CD, Postpneumonectomy oesophagopleural fistulaThorax 1980 35:865-68. [Google Scholar]
[4]. Wechsler RJ, CT of esophageal-plerual fistulaeAJR 1986 147:907-09. [Google Scholar]