Primary non-Hodgkin’s lymphoma of bone (PLB) is a rare entity. Patients generally present with localized bone pain and, less frequently, soft-tissue swelling or a palpable mass. Pathological fracture of the proximal femur and proximal humerus secondary to soft-tissue tumours is well documented in the literature; however, lymphomas presenting primarily at these sites with pathological fracture is unusual. A review of the world literature shows that the incidence of skeletal manifestation from NHL is less than 5%, and in all these cases, bony involvement was reported many years after presentation of the primary cancer. Histopathologically, PLB usually represents diffuse large B-cell lymphoma. We report our experience with two cases of Primary non-Hodgkin’s lymphoma of proximal femur and proximal humerus with pathological fracture and their management.
INTRODUCTION
Primary lymphoma of the bone (PLB) is a rare extranodal presentation
of non-Hodgkin’s lymphoma (NHL). It was first described by Oberling in 1928 [1]. It accounts for approximately 3% of the malignant bone neoplasms and it comprises of less than 5% of all the extranodal non-Hodgkin’s lymphomas. An osseous involvement
of a lymphoma is generally seen as a part of a multi-system dissemination. Primary lymphoma of the bone can be defined as a lymphoma which occurs in the bone without any evidence of a distal nodal or an extra-nodal tissue involvement [2,3]. PLB can involve any part of the skeleton, but a trend exists in favour of the bones with persistent bone marrow. The femur is the most common site and it is affected in 29% of the cases. The other sites include the pelvis, humerus, head and neck, and the tibia [4].The clinical presentation depends upon the rate of the tumour cell proliferation and on the initial localization. The patients generally present with localized bone pain and, less frequently, with a soft-tissue swelling or a palpable mass. On conventional radiology, PLB has a widely variable imaging manifestation which consists of either a ‘lytic destructive pattern’ or a ‘blastic sclerotic pattern’ [5]. Pathological fractures may be present in approximately one quarter of the cases, as were seen in our patients.
CASE: 1
A 58-year-old male patient presented with pain in the left hip of 5 months duration and difficulty in bearing weight on the left lower limb of 2 months duration. Clinically, the patient was well, with no history of fever, sweats, weight loss or fatigue. On examination, he was found to be normotensive and he had no palpable hepatospleenomegaly or lymphadenopathy. When the patient reported to our hospital, he had already been investigated elsewhere. His chest radiograph was normal, as was his full blood count and biochemical profiles. The X-ray of his pelvis with both the hips, showed an expansile lytic lesion in his neck and metaphyses of the left femur [Table/Fig-1]. MRI findings revealed an expansile lytic lesion in the left femoral neck and in the intertrochanteric region with an associated thin periosteal reaction and adjacent cortical thinning, which were suggestive of metastasis/an osteogenic tumour. The myeloma study was negative. The biopsy report was suggestive of a lymphoproliferative disorder which involved the bone. The patient was admitted to our hospital with a pathological fracture [Table/Fig-2] which was sustained by a trivial fall. He was operated on with resection of the proximal femur and reconstruction of the defect by using megaprostheses [Table/Fig-3]. The tissue was sent for a histopathological examination. The final pathologic diagnosis was a primary lymphoma- NHL, diffuse large B-cell type of the proximal femur. Postoperatively, the patient received chemotherapy which consisted of cyclophosphamide, adriamycin, vincristine, and prednisone (CHOP). After 18 months of the operation, there has been no relapse either clinically or radiologically [Table/Fig-4]. The present case agreed with the literature on primary bone lymphoma, in which the diagnostic problem, a trauma-related presentation and an excellent prognosis of a malignant tumour have been emphasized.
X-ray pelvis with both hips AP-view showing an expansile lytic lesion in neck and metaphyses of left femur without any periosteal reaction.

X-ray left hip AP-view showing an expansile lytic lesion in neck and metaphyses of left femur with pathological fracture.

X-ray pelvis with both hips AP-view showing replacement of left proximal femur with megaprostheses (immediate postoperative radiograph).

X-ray pelvis with both hips AP-view at 18 months follow-up showing well seated megaprostheses in-situ with no evidence of recurrence.

CASE: 2
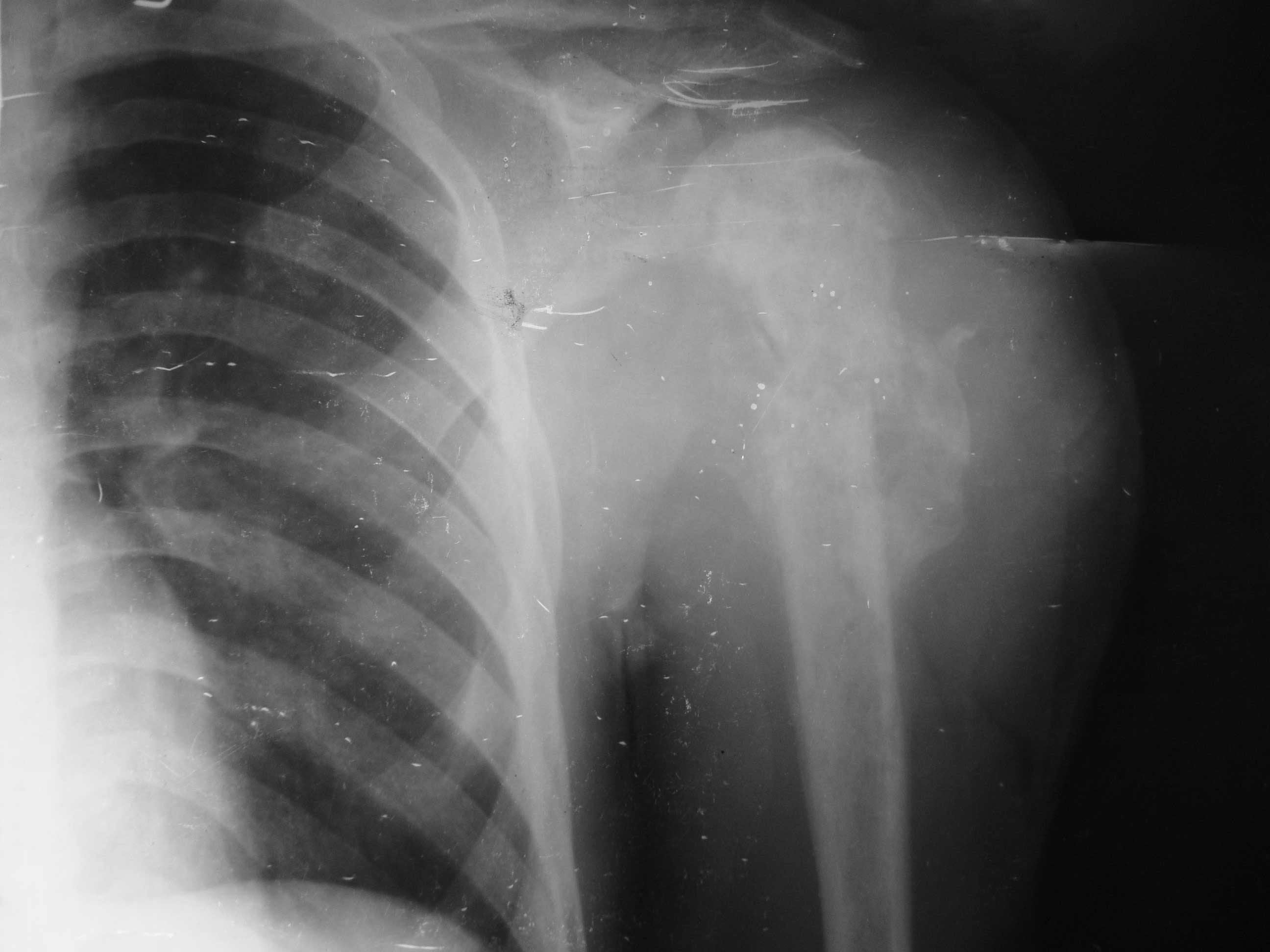
A 23-year-old male presented with pain and swelling of the left shoulder of 3 months duration. The pain worsened over the past 1 month, following a minor fall. Following the injury, the patient was unable to use his left upper limb. Clinically, a diffuse swelling was present around the shoulder girdle [Table/Fig-5]. No neck or axillary lymph nodes were palpable. There was no palpable hepatospleenomegaly or lymphadenopathy. The chest radiograph was normal. Both the WBC and the CRP levels were within the normal range. The only medications which were taken at the time of the presentation were non-steroid anti-inflammatory drugs (NSAIDS). A screening X-ray of his left shoulder showed an osteosclerotic lesion in the proximal humerus with a pathological fracture [Table/Fig-6]. Magnetic resonance imaging (MRI) of the left shoulder and the humerus showed that the lesion was hypointense on T1-weighted images and hyperintense on T2-weighted images. A malignant lesion was suspected and an open bone biopsy was performed. The biopsy revealed a diffuse, large, B-cell type of lymphoma which was positive for the leukocyte common antigen and CD20. A molecular analysis which was carried out with PCR revealed a monoclonal B-lymphocyte population. The diagnosis of diffuse large peripheral B cell lymphoma of the bone was confirmed. The patient was treated with both radiotherapy and systemic chemotherapy. The radiotherapy was performed with 25 Gy to the left shoulder. 6 courses of chemotherapy with the use of the CHOP regimen were completed. The therapeutic effects were assessed after two courses and at the end of the sixth course. After the 2 courses of the therapy, an X-ray of the left shoulder which was done, showed an osteosclerotic lesion in the proximal humerus, with a uniting pathological fracture [Table/Fig-7] and a clinically subsidence of a massive swelling [Table/Fig-8]. The patient showed a clinically complete remission, and neither relapse nor metastasis has been recognized till his last follow-up at 12 months [Table/Fig-9]. A continuous follow-up for the possibility of a local tumour recurrence and dissemination of the disease should be emphasized in these patients.
Clinical photograph of patient showing diffuse swelling around left shoulder girdle.

X-ray left shoulder AP-view showing osteosclerotic lesion in proximal humerus with pathological fracture, ill-defined radiolucencies and marked soft tissue shadow.
X-ray left shoulder AP-view at 2 months showing uniting fracture, sclerosis of proximal humerus with progressive mineralization of radiolucencies.

Clinical photograph of patient showing subsidence of massive swelling.

X-ray left shoulder AP-view at 12 months showing united pathological fracture, sclerosis of proximal humerus with mineralization of radiolucencies.

DISCUSSION
PLB occurs commonly between 20 and 50 years of age and it shows a male preponderance with a male to female ratio of 3:2. The femur (29%) is the most common site, followed by the pelvis (19%), humerus (13%), skull (11%) and the tibia (10%) [4]. Some series have found that the long bones and the flat bones are equally affected [6]. The clinical presentation includes local pain, swelling and sometimes even a pathological fracture. The diagnosis is established by biopsy. The other investigations which are done to establish the diagnosis include a skeletal survey, a bone scan and a bone marrow biopsy. CT scan of the whole abdomen and the chest to assess the lymph node involvement and serum LDH estimation are done as a part of the staging procedure [3]. In the younger patients, the differential diagnosis of PLB mainly includes osteosarcoma, Ewing’s sarcoma, and osteomyelitis. In the older patients, bone metastasis of the solid tumours should be considered.
A review of the world literature shows that the incidence of the skeletal manifestation from NHL is less than 5%, and that in all these cases, a bony involvement was reported, many years after the presentation of the primary cancer. The histological features of primary non-Hodgkin’s lymphoma of the bone are identical to those of the conventional, non-osseous forms of non-Hodgkin’s lymphoma. The hallmark attribute of the lesion is a replacement of the normal marrow constituents by neoplastic lymphoid tissue; however, the most common histologic subtype is diffuse large B-cell lymphoma [3,6]. For the diagnosis of PLB, Coley’s criteria should be met, namely a primary focus in a single bone, a positive histological diagnosis and a lack of evidence of a distal soft tissue or a nodal involvement [7].
A pathological fracture of the proximal femur and the proximal humerus, which is secondary to the soft-tissue tumours, has been well documented in the literature; however, lymphomas which present primarily at these sites with pathological fractures are unusual. The pathological fracture is due to either bone damage by the tumour, radiotherapy, or disuse atrophy. In a large series of 131 patients with primary bone lymphoma, Ramadan et al reported that one third of the patients had lymphoma involvement of the long bones, with pathological fractures occurring in only nine patients [6]. Therefore, our patients illustrated pathological fractures secondary to the lymphoma involvement of the femur and the humerus, which is uncommon even in patients with lymphoma involvement of the long bones. On conventional radiology, PLB has a widely variable imaging manifestation that was divided into certain radiographic patterns by Krishan et al., [5] in their evaluation of 20 cases of established primary lymphoma of the bone. The most common pattern which was noted was the ‘lytic destructive pattern’, which was reported in around 70% of the cases, followed by the ‘blastic sclerotic pattern’. The ‘lytic destructive pattern’ may present as permeative, moth-eaten or focal lyses with well-defined margins. A cortical erosion or destruction may occur, but there is usually a little periosteal reaction. Sequestra formation has also been demonstrated by CT in the cases of PLB. An associated soft tissue mass usually heralds a poorer prognosis. Our patient with the femoral lesion demonstrated radiographic findings which were consistent with a ‘lytic destructive pattern’, with a large focal lytic lesion, a permeative pattern which extended into the metaphysis, a cortical breakthrough and a pathological fracture. The plain radiographs often underestimate the extent of the lesion, as was observed in our patient, with absence of the soft tissue extension of the tumour mass and a periosteal reaction on the plain radiographs, which however were demonstrated on MRI. The other ‘blastic sclerotic pattern’, is more common in metastatic disease. Hodgkin’s lymphoma, the rarer type of primary bone lymphoma, may occasionally present with this pattern, but even in Hodgkin’s lymphoma, the lytic pattern predominates. Our patient with the humeral lesion demonstrated radiographic findings which were consistent with a ‘blastic sclerotic pattern’, with a large osteosclerotic lesion, ill-defined radiolucencies with a pathological fracture and a marked soft tissue shadow.
As with conventional radiology, the findings of the other imaging modalities such as bone scan, MRI, CT and PET are not specific. CT scan is useful for the disease staging and for delineating the spinal lesions, whereas MRI is the most sensitive imaging technique which can be used for the diagnosis of PLB [4]. On the other hand, in the follow-up examinations, it cannot reliably differentiate between a persistent disease and a healing bone. Although the role of the positron emission tomography (PET) scan is not well defined in PLB due to the rarity of the lesion, it is preferred over MRI for assessing the remission status. Lymphoma has an increased uptake on a bone scan.
The treatment of PLB typically involves a combination of radiation and chemotherapy. Even with the use of PET [8], the assessment of the remission status is rather difficult in PLB; hence, the chemotherapy should involve a sufficient number of treatment cycles, i.e., six to eight cycles. The role of surgery in the treatment of PLB is restricted to biopsies and the management of pathological fractures. The role of radiation in PLB is controversial. In a study which was done by Ramadan et al., [6] the patients with the advanced-stage disease who received chemotherapy plus irradiation, actually had a poorer outcome as compared with those who received chemotherapy alone. A major reason for avoiding radiotherapy, was the risk of the late effects from this treatment modality, especially the delayed bone growth in children and the development of a second cancer within a previously irradiated field [9].
To conclude, PLB is a rare malignant bone tumour with a variable radiographic manifestation. The prognosis, nonetheless, is much better than that of other malignant bone tumours. Thus, primary lymphoma of the bone should be considered in the differential diagnosis of bony tumours in young patients in the second to fourth decades of life. Chemotherapy, followed by radiotherapy, is the treatment of choice and these are associated with a good outcome. Thus, a high index of suspicion should be maintained for this disease in the patients who present with solitary bone lesions.
[1]. Oberling C, Les reticulosarcomes et les reticuloendotheliosarcomes de la moelle osseuse (sarcomes d’Ewing)Bull Assoc Fr Etude Cancer. (Paris) 1928 17:259-96. [Google Scholar]
[2]. Rahmat K, Wastie ML, Abdullah BJJ, Primary bone lymphoma: the report of a case with a multifocal skeletal involvementBiomedical Imaging and Interventional Journal 2008 3:52 [Google Scholar]
[3]. Singh T, Lakshmaiah CT, Suresh TM, Babu GK, Lokanatha D, Jacob LA, Halkud R, Primary bone lymphoma: A report of two cases and review of the literatureJournal of Cancer Research and Therapeutics 2010 6:296-98. [Google Scholar]
[4]. Salter M, Sollaccio RJ, Bernreuter WK, Weppelmann B, Primary lymphoma of the bone: The use of MRI in the pretreatment evaluationAm J Clin Oncol 1989 12:101-5. [Google Scholar]
[5]. Krishan A, Shirkoda A, Tehranzadeh J, Armin AR, Irwin R, Les K, Primary bone lymphoma: A radiographic-MR imaging correlationRadiographics 2003 23:1371-87. [Google Scholar]
[6]. Ramadan KM, Shenkier T, Sehn LH, Gascoyne RD, Connors JM, A clinicopathological retrospective study on 131 patients with primary bone lymphoma: A population-based study of successively treated cohorts from the British Columbia Cancer AgencyAnn Oncol 2007 18:129-35. [Google Scholar]
[7]. Coley BL, Higginbotham NL, Groesbeck HP, Primary reticulum cell sarcoma of the bone; a summary of 37 casesRadiology 1950 55:641-58. [Google Scholar]
[8]. Spaepen K, Stroobants S, Dupont P, The prognostic value of positron emission tomography (PET) with fluorine-18 fluorodeoxyglucose ([18F]FDG) after the first-line chemotherapy in non-Hodgkin’s lymphoma: Is [18F]FDG-PET a valid alternative to the conventional diagnostic methods?J Clin Oncol 2001 19:414-19. [Google Scholar]
[9]. Loeffler JS, Tarbell NJ, Kozakewich H, Primary lymphoma of the bone in children: Analysis of the treatment results with adriamycin, prednisone, oncovin (APO) and local radiation therapyJ Clin Oncol 1986 4:496-501. [Google Scholar]