Benign Breast Diseases (BBDs) is a group of breast diseases which is not cancer. It is the most common cause of breast problems in females and it is more frequent than the malignant ones [1–6]. In fact, it is at least 10 times more common than breast cancer in the west [7]. Upto 30% of the women who suffer from BBDs will require treatment at some time in their lives [8]. A triple assessment which is done by a clinical examination imaging like ultrasonography (USG) or mammography and a pathological examination – FNAC or core needle biopsy, during the initial consultation, allows a majority of the patients with discrete BBDs to be given immediate reassurance. Since a majority of the benign lesions are not associated with an increased risk for subsequent breast cancer, unnecessary surgical procedures can be avoided. Making an early diagnosis and planning the treatment within 72 hours of the first consultation, helps in alleviating unnecessary anxiety about breast cancer and those BBDs patients with an increased risk of malignancy like atypical hyperplasia, are given a prompt treatment, a proper follow-up and awareness regarding the risk of breast cancer.
The popular classification of BBDs according to the Aberration of the Normal Development and Involution (ANDI) causes confusion due to a lack of clarity in distinguishing between the normal physiological changes and the pathologic ones. One of the more satisfying classifications would be the one which was devised by Love S et al., [9], the so -called Nashville classification. According to this, BBDs is classified by 2 systems. Pathologically, BBDs is divided into (a) non-proliferative lesions, (b) proliferative lesions Sectionwithout atypia and(c) atypical proliferative lesions. Clinically, BBDs is classified as (a) physiologic swelling and tenderness, (b) nodularity, (c) breast pain, (d) palpable lumps, (e) nipple discharge and (f) infections or inflammation. In this study, we profiled the incidence of BBDs, the relative frequencies of the different types of BBDs and their clinical features. Secondly, we attempted at correlating the clinical and pathological findings wherever possible.
MATERIALS AND METHODS
This descriptive study was conducted in the Out Patients Department of General Surgery in Indira Gandhi Medical College and Research Institute, Pondicherry, India from October 2011 to September 2012. The first 100 (one hundred) women who were treated for BBDs were included in this study. The patients were required to give written informed consents prior to their enrolment in the study and a clearance was taken as per the institute’s ethical committee guidelines.
Inclusion criteria
Female patients with any benign disorder/disease of the breast-for example, a breast lump, breast pain or a nipple discharge, were included.
Exclusion criteria
Women with an obvious malignant disease or those who had been treated for malignancy earlier, were excluded in this study. However, any patient who was diagnosed with carcinoma or proliferative lesions after she was clinically diagnosed as benign earlier, was treated and included in this study.
A detailed history and a thorough physical examination were the basis of the study. After making an appropriate clinical diagnosis, one or more of the special investigations – FNAC, mammography, ultrasound or a core-needle biopsy were carried out for the confirmation of the diagnosis.
The FNAC smears were reported by using standardized diagnostic criteria by the same pathologist and they were categorized into non proliferative/proliferative without atypia/atypical proliferative lesion/frank carcinoma. A routine histopathological examination was done for the core biopsy and the excision biopsy samples and a cytohisto-correlation was also done. The clinical diagnosis, particularly in the case of the benign breast lumps, was compared with the cytological or the histological findings and the accuracy of the clinical diagnosis was evaluated.
RESULTS
A total of 100 female patients who attended in the Surgery Out-patients Department for breast diseases, were studied in the Department of General Surgery. The patients were broadly divided into 3 groups, depending on their symptoms or presentations, such as a breast lump, breast pain and a nipple discharge.
The commonest presentation was breast lumps which comprised 87 (87%) cases, out of which 27 (27%) had associated complaints like breast pain and nipple discharge. More than one symptom was present for the same patient.
Among 33 (33%) patients with breast pain, 9 (9%) patients complained of breast pain (mastalgia) only, who were treated by using a conservative approach or reassurance. The rest had associated complaints like breast lumps and nipple discharges. Half of these had pain in both the breasts. The pain was cyclical in 20 patients and it was non-cyclical in 13 cases.
Among the 8 cases with nipple discharges, only one case presented with nipple discharge only, without any associated lump or pain. The nipple discharge was blood in 3 cases and it was serosanguinous fluid in 4 cases, and only one case had a yellow discharge. The cause for 2 cases was intraductal papilloma and for the rest, it was mammary duct ectasia.
The different types of presentations and their incidences are shown in [Table/Fig-1].
Different types of presentation and their incidence
| Presentation | No. of patients | Percentage |
|---|
| 1. Breast lump only | 63 | 63% |
| 2. Breast lump + Pain | 20 | 20% |
| 3. Breast lump + Nipples discharge | 3 | 3% |
| 4. Breast lump + Pain + Nipple discharge | 4 | 4% |
| 5. Breast Pain only | 9 | 9% |
| 6. Nipple discharge only | 1 | 1% |
| Total | 100 | 100% |
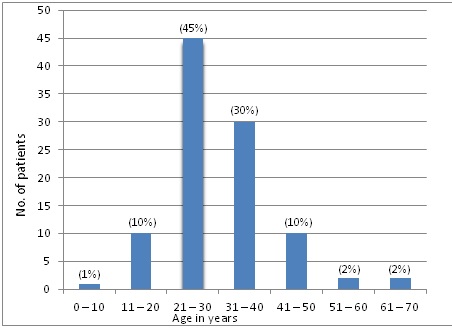
The age distribution of the patients is given in [Table/Fig-2]. The ages of the patients with BBDs ranged from 8 years to 68 years. The mean age at presentation was 28.4 years. 45 patients were in the age group of 21-30 years. The youngest was a 6 years old girl 504who presented with a small lump on the right side, with mastitis. The oldest was a 68 years old lady who had a lump on the right side of the breast, with invasive ductal breast cancer. Among the 87 patients with breast lumps, 39 patients are in the age group of 21-30 years. The lump was 3cm across in 40 cases, which happened to be the commonest size in the series.
Age-wise distribution of benign breast disease
There were 6 giant fibroadenomas, the largest being of the size, 7x9cm. There are 10 cases with multiple fibroadenomas. One young girl who was 22 years of age, presented with 8 fibroadenomas, five on the right side of the breast and three on the left side, which had average sizes of 3-2cms. The largest lump which was reported was a phylloid tumour of size 15x17cm, which was on the right side. Three of the non-tender breast lumps which were clinically reported as fibroadenomas, were diagnosed by HPE as proliferative disease with atypia in 2 cases and one was reported as florid hyperplasia. Two of the breast lumps which were clinically diagnosed as fibrocystic changes, were reported by a histopathological examination (HPE) as a proliferative lesion with atypia in one case and as invasive ductal carcinoma in the other case of the biopsy sample, for whom treatment was given in our hospital. Among the 100 patients, the right breast affected is 48 (48%) patients,
while the left breast was affected in 40 (40%) patients. In 12 (12%) cases, both the breasts were affected, as shown in [Table/Fig-3].
Side-wise distribution of benign breast disease
| Side involved | No. of cases | Percentage |
|---|
| Right breast | 48 | 48% |
| Left breast | 40 | 40% |
| Both breast | 12 | 12% |
| Total | 100 | 100% |
The incidences of different types of benign breast diseases are given in [Table/Fig-4].
Incidence of different types of benign breast disease
| Diagnosis | No. of BBD | Percentage |
|---|
| Fibroadenoma | 48 | 48% |
| Fibrocystic changes | 18 | 18% |
| Breast abscess | 12 | 12% |
| Mastalgia | 10 | 10% |
| Nipple discharge Intraductal papilloma – 2 Mammary duct ectasia – 6 | 8 | 8% |
| Accessory breast | 5 | 5% |
| Mastitis | 5 | 5% |
| Galactocele | 4 | 4% |
| Proliferative disease with atypia | 3 | 3% |
| Proliferative disease with florid hyperplasia | 1 | 1% |
| Invasive ductal carcinoma | 1 | 1% |
Clinical and histocytological correlations
The diagnoses of the lumps were confirmed either cytologically or histologically, or in both ways. FNAC was done in 87cases. FNAC and biopsy were done in 65 cases. The accuracy of the clinical diagnosis of fibroadenoma was 92% (48 out of 52 cases). Among the 65 cases of excised biopsies, 3 cases were reported as proliferative lesions with atypia. Two FNAC cases of proliferative lesions with atypia were missed cytologically and they were subsequently diagnosed by HPE. The clinical diagnoses of the fibrocystic changes were made in 22 cases and 18 of them were correct. One of them was reported by HPE as a proliferative lesion with atypia and the oldest lady of this group was reported as invasive ductal carcinoma, for whom treatment was given in our hospital and they were advised follow up. So, the diagnosis was wrong in these two cases of fibrocystic changes. Three of the non-tender breast lumps which were clinically reported as fibroadenomas, were diagnosed by HPE as proliferative disease with atypia in 2 cases and one was diagnosed as florid hyperplasia. On the whole, the clinical diagnosis was correct in 80 out of the 87 patients with benign breast lumps (91.95% accuracy).
DISCUSSION
Benign breast diseases includes a heterogeneous group of conditions which range from normal, to aberrations in the physiology, to frank disease. The patients of BBDs generally present with one or more of these complaints – breast lump, breast pain or nipple discharge. It has been recommended that all the patients with discrete breast lumps should undergo a triple assessment to make an early diagnosis. By this approach, we provided the diagnoses of most of the benign breast conditions within 72 hours of the initial consultation. In the study of Foncroft LM et al., [10], they found that 87.4% of the women who attended the Wesley Breast Clinic had presented with breast lumps, while in the series of Ratana Chaikanont T [11], a breast lump was the presenting symptom in 72.35% of the 331 benign breast patients. The corresponding figure for our study was 87%. Fibroadenomas accounted for 52.74% of the benign breast lumps in our study. Our finding was in agreement with most of the available literature on benign breast lumps, where the frequency of fibroadenoma ranged from 46.6%-55.6% [12–15]. The peak incidence of fibroadenoma ranged from the 2nd to the 3rd decade of life, which was consistent with the findings of other studies. FNAC was the quickest and the most reliable method which helped in making the diagnoses of the breast lumps.
The fibrocystic changes were the next common condition in our study and a majority of the patients belonged to the 3rd and 4th decades. The incidence varies geographically. Many authors like Adesunkanmi AR and Agbakwuru EA and Ihekwaba FN found that the incidence of the fibrocystic changes ranged from 29.5-42.2% for the benign breast lumps [12–13]. We had a slightly smaller figure, with 19.7%.
The mean age at presentation was 28.4 years. In the age group of 21-30 years, there were 45 patients. This was almost similar to the observation which was made by Navneet Kaur et al.,[16].
The incidence of breast pain in our series was 33%, which was nearly equal to the breast pain series, which ranged from 12.8%- 30.3% [11–17]. Leis HP et al., [18] reported that the incidence of breast discharge was only 9% of all the breast complaints in his study, which was almost equal to the 8% incidence which was found in our study.
Out of the 8 cases of nipple discharge, 2 were intraductal papilloma with bloody nipple discharges and 6 were mammary duct ectasia. The treatment of the nipple discharge must be done first, to exclude carcinoma on occult blood test and cytology. A simple reassurance may then be sufficient, but if the discharge is proving to be intolerable, an operation must be done to remove the affected duct or ducts [8]. A total excision of 2 cases of intraductal papilloma was done. Mammary duct ectasia generally does not require surgery and it should be managed conservatively [19]. We treated 6 cases of mammary duct ectasia by using a conservative management.
The incidence of benign breast diseases begins to rise in the 2nd decade and it peaks in the 4th or 5th decades as compared to the malignant lesions, for which the incidence continues to rise after menopause [20–22]. In the study of Dupont and Page [23], atypical hyperplasia was identified in only 4% of the biopsy samples. In our study, 3 patients with breast lumps had proliferative lesion with atypia on the biopsy samples, which was 4.6% of the total 65 biopsy samples which were taken. The findings of our study were almost the same as those of their studies. However, our samples were smaller in number than theirs.
We advised follow up every 3 months for both the low and high risk categories, since some studies have shown the progression of the low risk category to carcinoma [24]. The risk factors for carcinoma of the breast were explained to the patients, which is a two-fold increased risk for developing Ca breast in florid hyperplasia and a four-fold increase risk in proliferative lesions with atypia. The only case with invasive breast cancer was treated in our hospital and she was advised follow up every 3 months. Currently, there is a controversy over the classification of the proliferative lesions and the microscopic risk assessment, which have less relevance in the clinical practice. So, there is a need for non morphologic markers (genetic/molecular) so that chemoprevention agents can be used as an alternative to surgery and so that the histo-pathological criteria can be refined for the risk assessment [25].
CONCLUSIONS
Benign breast diseases is a common problem in women. A lump in the breast is the commonest presentation. Breast pain and nipple discharge are the other symptoms. Most of the patients have more than one symptom. The commonest age group which is affected is the 21-30 years age group. Among the breast lumps, fibroadenoma is the commonest, followed by fibrocystic changes and breast abscesses. The other lumps are relatively uncommon. Breast pain may occur alone or in association with a lump or a nipple discharge. The incidence of cyclical pain is 20% and that of non-cyclical pain is 13%. The nipple discharge, particularly if it is serous or greenish, is harmless. The clinical diagnoses of the benign breast lumps were accurate in 91.95 % cases.
The risk factors for developing invasive carcinoma in the patients with proliferative lesions were also identified and the patients were advised follow-up. Since there is no consensus on the morphologic risk markers, in future, molecular genetic markers may help in the risk stratification, which will help in a better clinical management.