Semmelweis’s Forgotten Gift: Has Handwashing Lost Its Importance?
Yashasvi Chugh1, Shrikala Baligathe1
1 Intern, Kasturba Medical College, Mangalore, India.
2 Professor and Head of Department Microbiology, Kasturba Medical College, Mangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shrikala Baliga, Microbiology Department, Kasturba Medical College, Light House Hill Road, Mangalore- 575001
Phone: +91 9972413064
E-mail: shrikalab@yahoo.com
Background and Objectives: The hands harbour a kaleidoscope of bacteria, thus making hand washing an essential attribute in preventing the transmission of nosocomial pathogens. Medical students, as a part of their curriculum, are taught about handwashing. However, their adherence to it is doubtful. This study was carried out to ascertain the impact of educating medical students about the correct technique of handwashing and its role in reducing the bacterial contamination of their hands.
Methods: The hands of 50 medical students who attended the clinical postings were screened for bacterial colonisation. Following their screening, 30 students who had the highest colonization of bacteria were followed up for a second round of sampling. They were further allotted into two arbitrary groups: the control group and the test group. The procedure for an adequate handwash was taught to the test group, whereas the control group had been taught it as a part of their clinical curriculum during their postings. Each student’s hands were sampled, both preceding and following a handwash.
Results: Following the handwashing, the students of the test group had a significantly (p=0.011) lower mean bacterial colonization on their hands, in contrast to the control group. Moreover, 86.7% of the students from the control group harboured Staphylococcus aureus even after handwashing, whereas only 40% of the test group students had it. The preliminary screening concluded that: (i) Females harboured a significantly greater (p=0.038) bacterial colonization on their hands than males.(ii) The students who wore rings showed a higher contamination (p=0.05).
Interpretation and Conclusion: This study revealed that the students of the test group were at an advantage, as they had been given immediate prior instructions, whereas the control group had been taught the same technique at their clinical postings and were not instructed preceding the handwash and the sample collection. It can be concluded that a prior instruction in the form of teaching or visual aids such as posters etc., regarding the method of handwashing, is essential for an effective handwash, regardless of the past teaching. The instruction that is imparted to the students as a part of their curriculum needs reinforcement.
Handwashing, Medical students, Hygiene
INTRODUCTION
A study of the microbial flora on the hands is of utmost relevance, as the hands are of primary concern in the spread of nosocomial infections [1]. It has been estimated that an increase in the hand washing compliance by 1.5 to 2 fold would result in a 25-50% decrease in the incidence of nosocomial infections [2]. Similar was the belief of Dr.Ignaz P Semmelweis who first hypothesised in the mid 1800s, that the incidence of nosocomial sepsis would decline following a handwash [3].
The microbial hand flora consists broadly of two types; the transient and the resident flora [2]. The transient flora comprises the microorganisms which are acquired by contact with patients or environmental surfaces. These organisms are easily removed by washing and are paramount in causing nosocomial infections [1,2,4]. The resident flora on the other hand are not easily removed by ordinary handwashing and they are rarely problematic to the patients, except during invasive procedures [4]. Pittet and colleagues studied the contamination of the Health Care Workers’ (HCWs) hands before and after a direct patient contact; they found that the number of bacteria which were recovered from the fingertips after a direct patient contact and respiratory tract care were most likely to contaminate the fingers of the caregivers [5].
The primary purpose of hand washing is to remove the transient flora and thereby to reduce nosocomial infections [4]. Therefore, hand washing is considered as the most effective measure to prevent the spread of nosocomial infections [2].
It has been previously shown that an improvement in the hand hygiene compliance results in reduction of health care associated infection [6]. Bhalla and colleagues studied the patients with skin colonization with S. aureus (including MRSA) and found that the organism was frequently transferred to the hands of the HCWs who touched both the skin of the patients and the surrounding environmental surfaces [7]. A study which was done by Trick and colleagues found that 40% of the nurses harboured the gram-negative bacilli, Acinetobacter spp. on the skin under rings and that some nurses carried the same organism under their rings for months [8].
Medical students, as a part of their curriculum, examine numerous patients during their clinical postings. Though the importance of handwashing has been emphasized, their adherence to it is doubtful.
Our study was carried out on the undergraduate medical students who attended the clinical postings in 4 departments of the medical college, aiming to evaluate the level of bacterial contamination on their hands and the effectiveness of their handwashing techniques.
METHOD
All the undergraduate medical students who attended their clinical postings in the departments of Obstetrics and Gynaecology, Medicine, Community Medicine, and Surgery from July to September 2011 were eligible for inclusion in the study. Two students with evident eczema and one with onychomycosis were excluded from the data collection. A note of the students who wore rings was made before initiating the sampling. By taking the proportion of the students who were expected to have bacteria on their hands to be 50% and with a 95% confidence level and 80% power of the test, the minimum sample size which was required was 43. Thus, a total of 50 undergraduate medical students (12 to 13 volunteers from each department) were randomly selected from the college and they were requested to participate.
As soon as they were relieved from their clinics, they were asked to come to the Microbiology Lab at the central hospital. After obtaining written informed consents from them, we obtained pre-handwash samples of their hand flora by using the Broth Rinse Technique [9]. The participating students inserted both their hands (one after the other) in a sterile plastic bag which contained 50ml of Trypticase soy broth. The students were requested to open and close their fists for a total of 30 seconds, while they were immersed in broth. The broth was cultured onto Trypticase soy agar (Himedia Laboratories Pvt. Ltd.). Ten fold dilutions of the broth was made (1in10, 1in100, and 1in 1000) [10]. A sample of 0.1ml from each dilution was plated onto the Trypticase soy agar and they were incubated for 24-48 hours at 370C. The enteric pathogens were quantitated by plating 0.1ml of the broth onto Mac Conkey’s agar plates. The plates were examined after 24 to 48 hours of incubation [10]. The total number of aerobic bacteria per millilitre of the broth was determined by the colonies on the Trypticase soy agar plates. The viable counts were calculated from the average colony counts/plate which were multiplied by the dilution and they were expressed as colony forming units per millilitre of the broth. Once the colony counts of the rinsed broth were obtained, 30 students with the highest colony counts were called back to the lab within the next ten days after their clinics had got over. On their subsequent visit to the lab, their pre hand wash samples were taken by using the same Broth Rinse Technique [9]. The organisms were identified by using standard microbiological techniques [11]. The students were then divided into two equal arbitrary groups: the test and the control. The test group’s members were asked to wash their hands after having been shown the proper handwashing technique as per the WHO guidelines, whereas the control group members were not given any new instructions preceding the sample collection [2]. The quantity of antiseptic soap which had to be used for each handwash was fixed to 2ml, irrespective of the group. The antiseptic soap which was used in this study was BactoScrubR, which contained 4% (w/v) Chlorhexidine Gluconate. A post hand wash sample was obtained by using the same method [9]. An ethics committee approval was taken before initiating all the microbiological sampling procedures. To avoid any technical errors during the sampling, the quality of all the media which were used was tested for performance as well as sterility. The collected data was preserved in Microsoft Excel and their analysis was done by using the Statistical Package for Social Sciences (SPSS), Version 11.5. An association was found by using the Chi square test.
RESULTS
Fifty undergraduate medical students took part in the study: 13 each from the departments of Surgery and Medicine and 12 each from the departments of Community Medicine, Obstetrics and Gynecology.
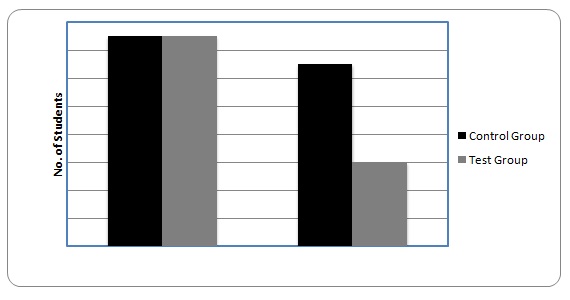
There were in total 26 men and 24 women. The mean of colonization among the students before the handwashing was 1.3+0.4 x 106 cfus/ml of the broth. The colonization on the hands of the women contributed a mean of 1.7x106 cfus/ml, which was significantly greater than the colonization on the hands of the men, which was 0.9x106 cfus/ml (p=0.05). The students who wore rings possessed a greater contamination with bacteria.(p=0.05) [Table/Fig-1] Following the preliminary screening, 30 students (those with the highest colonization) from among the aforementioned 50 students, were arbitrarily allotted into a test group(n=15) and a control group (n=15) .The mean bacterial colonization on the members in the test group was 2.5x105 CFU/ml and that on the members of the control group was 1.9x105CFU/ml. S.aureus (100%) was the predominant microbe which was found to contaminate the hands in both the groups. Following the handwashing, a reduction in the bacterial colonization was noted in both the groups; however, it was significantly lower in the test group (p=0.011). Moreover, fewer members of the test group retained S.aureus as a part of their hand flora after the handwashing [Table/Fig-2].
A comparison of the mean bacterial contamination on the hands of students with and without rings
| Students wearing Rings (n=12) | Students not wearing rings(n=38) | p* (Pearson’s Chi Square Test) |
|---|
| Mean contamination of hands (cfu/ml) | 3.3x106 cfu/ml | 0.7x106 cfu/ml | 0.05 |
A comparison of the No. of Student from the Test and control groups harbouring S.aureus on their hands before and after Hand washing. Handwashing effectively reduced the S. aureus in the test group.
DISCUSSION
In 1847, Ignaz Semmelweis insisted that the doctors who performed necropsies should wash their hands in chlorinated lime before delivering babies, thereby reducing the streptococcal puerperal sepsis from 22-23%. Many other studies have also shown that the doctors who decontaminated their hands between the patients could reduce nosocomial infections [12]. However, many observational studies have indicated that the compliance of handwashing, especially among doctors, is the least [12]. Though doctors have a lesser contact time as compared to nurses, they may still harbour harmful pathogens as their transient flora which can transmit infections. Health care associated pathogens have been recovered from patient wounds, and draining sites. They even colonize the intact skin of the patients [12].
In our study, the hands of the medical students who were screened, had a mean colonization of (1.3+0.4) x 106 CFUs/ml of broth. Our figures were comparable with the data from similar studies which were conducted on health care workers, where the mean colonization was found to be 3.9 x 104 to 4.6 x 106 [13].
The hands of the women in our study were found to be more colonized than that of the men. It has been hypothesised that women have a greater diversity of flora on their hands, which could be due to the more alkaline pH of their skin, which favours the growth of bacteria [14].
The ring wearing students were found to have a greater colonization with transient flora. Trick et al., had similar findings, where they found that the ring wearing was associated with a 10-fold higher median skin organism counts [8]. S.aureus was the most prevalent organism (100%) which was detected. Borges et al., [9] studied the hands of nurses in a general hospital and found a prevalence of 23% for S. aureus.
It was noticed that the bacterial colonization in the test group after the handwashing was on an average, 2.3x102 cfus/ml, which was much lower than that in the control group (1.4x104 cfus/ml). This was statistically significant (p=0.011), indicating that giving correct instructions regarding the hand washing technique preceding the task, results in a significant decline in the bacterial colonization. Various studies have indicated that giving repeated instructions to the health care workers regarding hand hygiene, helps in their adherence to the hand hygiene practices [15]. We would like to add that a frequent reinforcement ( in the form of instructions or visual aids) at least on a daily basis, regarding effective handwashing, would further benefit in reducing the bacterial counts and in improving the infection control.
Unfortunately, our study was limited and no correlation could be inferred between the contamination of the hands of students and the transmission of pathogens to susceptible patients.
Simple hand hygiene should be taught and learnt throughout the undergraduate course, both theoretically in the lectures and it should be practically reinforced in the laboratory, in the dissection room and in the clinical setting [16]. The handwashing which is performed by the correct technique in a clinical environment will be effective in infection control and it will also help in reducing nosocomial infections. This will go a long way in improving the adherence to handwashing and in the reduction of the bacterial counts among the health care personnel, thereby reducing transmission of nosocomial infections.
[1]. Sutter ST, Frei R, Dangel M, Effect of teaching recommended World Health Organization technique on the use of alcohol-based hand rub by medical studentsInfect Control Hosp Epidemiol 2010 31(11):1194-95. [Google Scholar]
[2]. World Health Organisation (WHO)WHO Guidelines for Hand Hygiene in Health care 2009 Geneva, SwitzerlandWHO [Google Scholar]
[3]. Noakes TD, Borrensen J, HewButler T, Semmelweis and the aetiology of puerperal sepsis 160 years on: an historical reviewEpidemiol. Infect 2008 136:1-9. [Google Scholar]
[4]. Bolon M, Hand HygieneInfect Dis Clin N Am 2011 25:21-43. [Google Scholar]
[5]. Pittet D, Dharan S, Touveneau S, Bacterial contamination of the hands of hospital staff during routine patient careArchives of Internal Medicine 1999 159:821-26. [Google Scholar]
[6]. Pittet D, Hugonnet S, Harbarth S, Effectiveness of a hospitalwide programme to improve compliance with hand hygieneLancet 2000 356:1307-12. [Google Scholar]
[7]. Bhalla A, Aron DC, Donskey CJ, Staphylococcus aureus intestinal colonization is associated with increased frequency of S. aureus on skin of hospitalized patientsBMC Infectious Diseases 2007 7:105 [Google Scholar]
[8]. Trick WE, Vernon MO, Hayes RO, Impact of Ring Wearing on Hand Contamination and Comparison of Hand Hygiene Agents in a HospitalClin Infect Dis 2003 36:1383-90. [Google Scholar]
[9]. Borges LFA, Silva BL, Filho PPG, Hand washing: Changes in the skin floraAm J Infect Control 2007 35:417-20. [Google Scholar]
[10]. Brown R, Poxton IR, Centrifuges, colorimeters and bacterial counts. In: Collee JG, Marmion BP, Fraser AG et alMackie and McCartney: Practical Medical Microbiology 1996 4814thChurchill Livingstone:850 [Google Scholar]
[11]. Murray PR, Baron EJ, Jorgensen JH, Manual of clinical microbiology 2004 8thWashington, DCASM Press [Google Scholar]
[12]. Centers for Disease Control and Prevention. Guideline for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR. 2002;51 [Google Scholar]
[13]. Boyce JM, Pittet D, Guideline for hand hygiene in health-care settings. Recom- mendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA hand hygiene task forceMMWR Recomm Rep 2002 51(RR–16):1-45. [Google Scholar]
[14]. Fierer N, Hamady M, Lauber CL, The influence of sex, handedness, and washing on the diversity of hand surface bacteriaProc Natl Acad Sci U S A 2008 105(46):17994-99. [Google Scholar]
[15]. MacDonald F, Dinah D, MacKenzie. Performance feedback of hand hygiene, using alcohol gel as the skin decontaminant, reduces the number of inpatients newly affected by MRSA and antibiotic costsJ Hosp Infect 2004 56:56-63. [Google Scholar]
[16]. Fisher D, Pereira L, Ng TM, Teaching hand hygiene to medical students using a hands-on approachJ Hosp Infect 2010 76:84-95. [Google Scholar]