The iliolumbar artery classically arises from the posterior radix of the internal iliac artery and it extends in an oblique fashion superiorly and laterally, in front of the sacroiliac joint and the lumbosacral trunk. It crosses the obturator nerve and the external iliac artery and vein. Subsequently, it reaches the medial edge of the psoas major, it branches off the lumbar and the iliac arteries behind this muscle, and it joins the arterial supply of the iliac bone, iliopsoas, quadratus lumborum, and the cauda equina [1]. The internal iliac artery and its branches can be damaged during the anterior and the anterolateral spinal approaches, lumbosacral spinal endoscopic procedures, and especially, during far-lateral disc excisions. Additionally, during anterior approaches to the sacroiliac joint for arthrodesis or internal fixation, posterior pelvic fractures (open book or shearing fractures, these vessels can be injured [2,3]. The location and the variations of the iliolumbar artery are very important for surgeons, since it is used as a feeding pedicle in bone flaps and as it has an injury risk after a pelvic trauma or regional operations [4].
The iliolumbar vein drains lower lumbar region,need to be identified during lumbar spine surgeries using anterior approach.[5-17] during mobilization of great vessels to expose the L4/L5 junction, surgeons have to careful not to injure the vein which can cause massive bleed. [18-20] this type of bleed can be controlled by dissection and ligation of vein during surgery. we tried to study detailed anatomy of iliolumbar veins. [5-17,21]. Our aim was to describe these vessels, their variations and their relationship with the nearby structures.
Materials and Methods
We dissected the iliolumbar veins and the iliolumbar artery bilaterally in 20 formalin-fixed adult cadavers. The origin, diameter, and the course of the iliolumbar artery were evaluated. The common iliac artery, the external iliac artery, and the internal iliac artery were dissected. The diameter of the iliolumbar artery at its origin, its length up to the point where it divided into the lumbar and the iliacus branches, the distance between the iliolumbar artery and the L5 inferior margin, and the distance between the iliolumbar artery and the bifurcation point of the common iliac artery were measured.
The presence of the veins was noted and the patterns of their drainage, their dimensions, their points of confluence with the common iliac vein and the obliquity of the veins were noted. The obturator nerve and the lumbosacral trunk which are closely related, were determined and dissected. The relation of the iliolumbar artery and the veins with the obturator nerve and the lumbosacral trunk was determined and recorded. The measurements of the diameters of the vessels were performed by using a Vernier caliper which was sensitive to 0.1 mm. The lengths of the vessels were measured by using a thread and a scale by following their curves.
Results
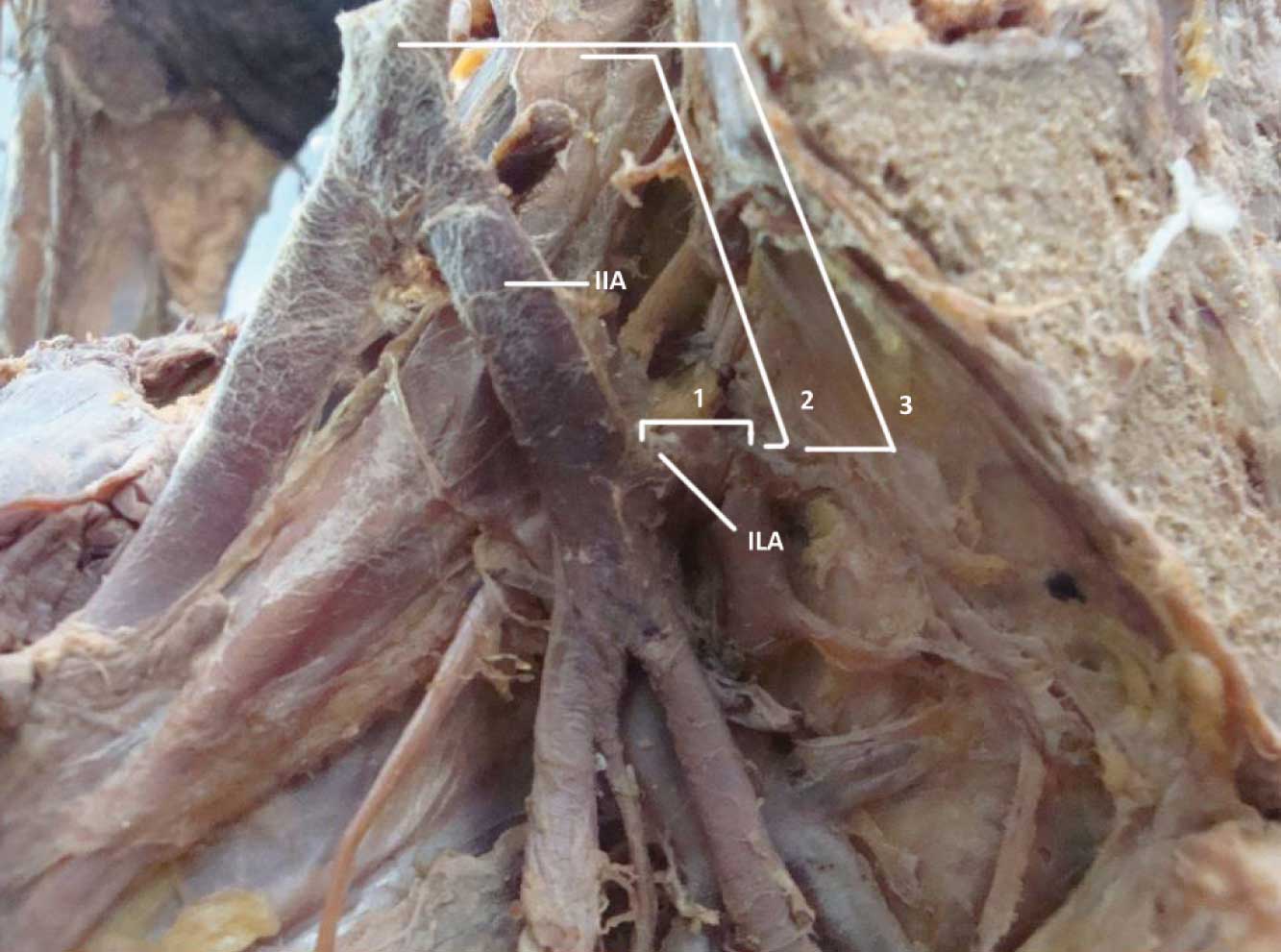
The iliolumbar artery originated from the posterior division of the internal iliac artery in 80% (32 arteries) [Table/Fig-1], from the internal iliac artery itself in 20% (8 arteries) and from two different points from the internal iliac artery or the common iliac artery in none of cases. The mean diameter of the iliolumbar artery at its origin was 3.5±0.5 mm. The mean distance between the origin of the iliolumbar artery and the bifurcation point to the iliacus and the lumbar branches was 12.2±5.5 mm. The distance between the origin of the iliolumbar artery and the lower edge of the fifth lumbar vertebra was 43.2±11.6 mm. The distance between the origin of the iliolumbar artery and the bifurcation point of the common iliac artery was 38.7±10.6 mm. In all the cases, the iliolumbar artery showed two branches and the lumbar branch supplied the psoas major and the quadratus lumborum and it anastomosed with the fourth lumbar artery. A small spinal branch through the intervertebral foramen between the fifth lumbar and the first sacral vertebrae, though it was described that it would supply the cauda equine, it was really difficult to trace. The iliac branch supplied the muscle and the bone iliacus and it anastomosed with the iliac branches of the other to supply the gluteal and the abdominal muscles.
Commonest branching pattern of iliolumbar artery [ILA]
Different parameters measured:
Distance from Origin to branching of iliolumbar artery-1
Distance between 5th lumbar vertebra to origin of ilolumbar artery-2
Distance between common iliac artery to origin of ilolumbar artery-3
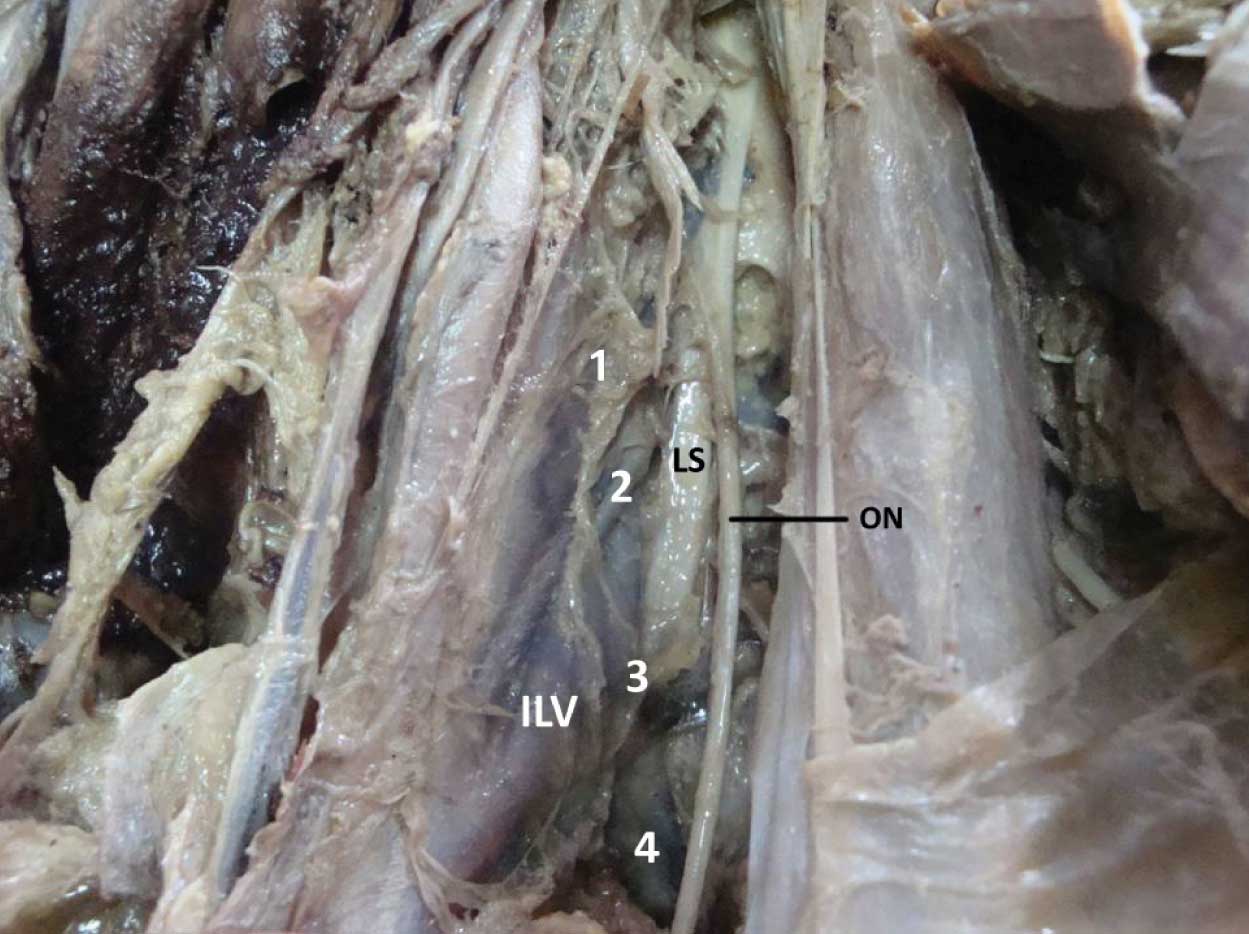
The mean distance of the iliolumbar veins from the inferior vena cava, overall, was 35±9.9 mm. The mean width of the mouth of the iliolumbar vein was10.7±5.1 mm, and the mean angle of obliquity of the vein with respect to the long axis of the common iliac vein was 75.50. There were some variations in the tributaries which drained into the main iliolumbar vein [Table/Fig-2]. Two main tributaries drained into an iliolumbar trunk in 40% (16 cases). Three or more tributaries drained into an iliolumbar vein in 55% (22 cases) [Table/Fig-3]. A single trunk drained into the common iliac vein in 5% (2 cases) .In all dissections, the tributaries drained the iliacus and the psoas muscles. There was a tributary which drained the fifth lumbar vertebral body in 10% (4 cases). These were difficult to follow, but they could communicate with the internal vertebral venous plexus. Of great interest was the presence of a distal or an accessory vein. In a system with a true main and an accessory iliolumbar vein, the mean distance between the two was about 3 cm and both ran more horizontally.
Male and female distribution and side distribution of iliolumbar veins
| No of tributaries forming the iliolumbar vein | Males [16] | Females [4] |
|---|
| Right [16] | Left [16] | Right [4] | Left [4] |
|---|
| Single | 1 | | 1 | |
| Two | 8 | 8 | 1 | 1 |
| Three or more | 7 | 8 | 2 | 3 |
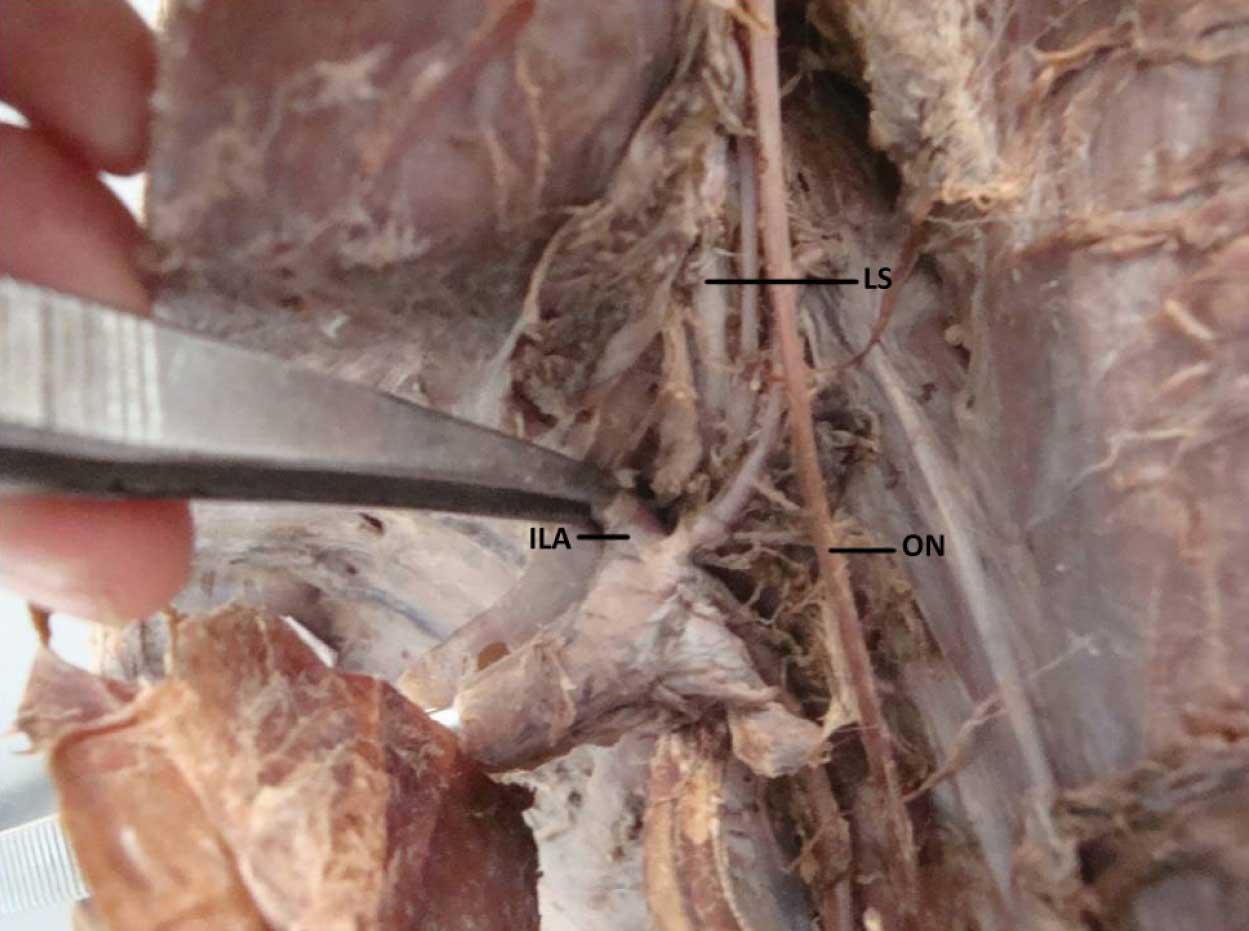
Iliolumbar veins[ILV] are passing behind obturator nerve [ON] but anterior to lumbosacral trunk [LS] and 4 tributaries of Iliolumbar vein passing between lumbosacral trunk and obturator nerve
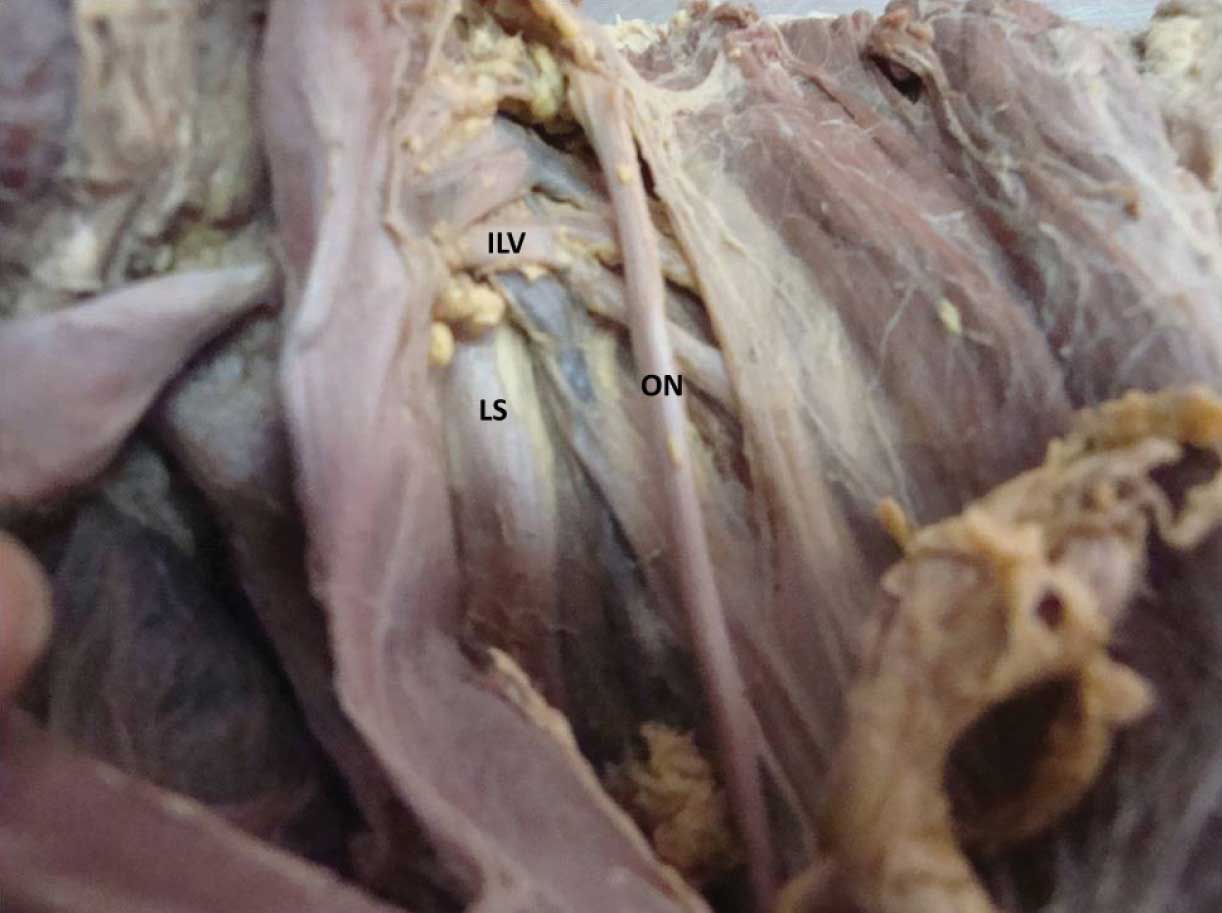
The most intimate relationship with the vein was that of the lumbar plexus, and in particular, with the obturator nerve and the lumbosacral trunk. The iliolumbar artery passed anterior to the obturator nerve in 70 % cadavers (28 cases) and posteriorly in 30 % cadavers (12 cases). The veins were lying anterior to the obturator nerve in 45 % cadavers (18 cases) and posterior to the nerve in 55 % cadavers (22 cases). In cases of multiple tributaries draining into the iliolumbar vein, the correlation of the tributaries was variable, few passed anterior and few passed posterior [Table/Fig-3 and 4].
Ilolumbar vein receiving 4 tributaries [1, 2, 3, 4], upper two passing behind lumbosacral trunk lower two tributaries are passing between lumbosacral trunk and obturator nerve
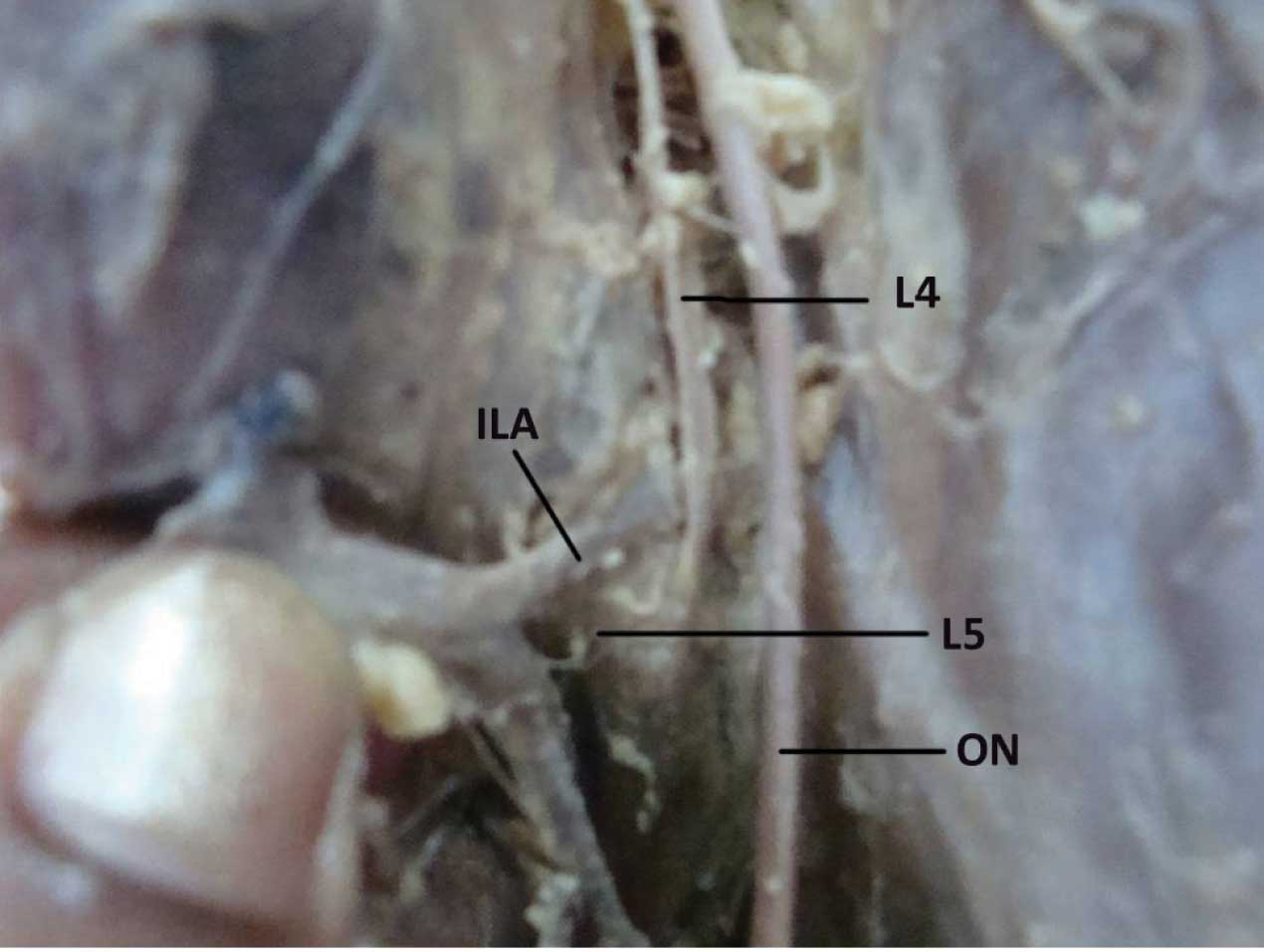
The iliolumbar artery was seen anterior to the lumbosacral trunk in 30% (12 cases), posterior in 54% (24cases) and it was cleaved in 8% (2cases) [Table/Fig-5] The branches of the artery were passing on either side of the lumbosacral trunk to enclose it like a clasp in 8% (2 cases) [Table/Fig-6]. The veins were anterior to the lumbosacral trunk in 40% (16 cases) and they were posterior in 60% (24 cases).
Iliolumbar artery branch is passing between L4 & L5 spinal nerves of lumbosacral trunk
Iliolumbar artery [ILA] branches are passing on either side of lumbosacral trunk [LS]
Discussion
In reconstructive bone surgery, vascularized bone grafts have some advantages such as a rapid bone healing and a decreased morbidity. In these surgical approaches; the fibula, iliac crest and the ribs are used frequently as donor sites [1, 22, 23]. The iliac crest is supplied by different vessels and it can be used in reconstructive bone surgeries in different ways [1]. The deep circumflex iliac artery, the superior gluteal artery, the fourth lumbar artery, and the iliolumbar artery are used as vascular pedicles in iliac crest flaps. The iliolumbar artery and its branches are used in bone reconstructions and particularly in lumbar spinal surgeries, as supplying pedicles, because it is easily defined, it lies in the loose connective tissue, and it has an appropriate length and diameter. Besides serving as a vascular pedicle of bone grafts, the trajectory of the iliolumbar artery is important because it is vulnerable to injury during lumbosacral spinal surgeries, anterior approaches to the sacroiliac joint, and posterior pelvis fractures. Harrington [4] reported that the iliolumbar artery can be injured during an L5-S1 far-lateral disc excision and he emphasized the importance of its variations at this level. Ebraheim et al., [2] reported that the iliolumbar artery and the branch supplying ilium that arises from the iliolumbar artery have a risk of injury during anterior approaches to sacroiliac joint for arthrodesis and an internal fixation. Thus, the anatomic location of this artery must be well known.
In addition, Yiming et al., [3] suggested that the iliolumbar artery can be injured during open-book or shearing fractures because it has very close relationship with the sacroiliac joint. So, if a patient has a pelvic posterior arcus fracture and bleeding symptoms, the risk of injury of the iliolumbar artery should be considered. The vascular anatomy of the pelvis and the sacrum is also very important in orthopaedic surgeries and in some spinal fixations. The relationship of the iliolumbar artery with the sacroiliac joint and L5 increases the risk of injury of artery during posterior pelvic fixations or lumbosacral implantations. The anterior exposure of the lumbosacral junction and the L4/L5 disc space is widely used in the surgical treatment of tumours, infections, and degenerative disorders. A posterior surgery is advocated for open-book type pelvic fractures, and it can be used in a percutaneous way [24]. It is also indicated for spinopelvic fixations in neuropathic scoliosis. For these approaches, the determination of the variations of the iliolumbar artery and the topographical patterns are crucial. Harrington [4] emphasized that the iliolumbar artery variants may be at the margins of extraforaminal intervertebral disc exposures, and that thus, the preoperative magnetic resonance imaging scans should be evaluated for this vasculature structure. It was biomechanically shown that the bicortical screw purchase to the sacrum increases the pull-out strength [25]. This theory may be adapted to other cancellous bones such as the pelvis and the sacroiliac joint. The tips of the screws or pins may penetrate the inner cortex of the pelvic bones and they may damage the vascular structures [26]. Therefore, the iliolumbar artery variations and the related neurovascular structures are important.
Chen et al., [22] reported that the iliolumbar artery arises 96.3% from the internal iliac artery and 3.7% from the common iliac artery. Yiming et al., [3] studied 10 cadavers and found that theiliolumbar artery arises from the internal iliac artery in all. In our study, the iliolumbar artery arose mostly from the posterior trunk of the internal iliac artery in 80% cadavers, from the common iliac artery in 0% cadavers and from the internal iliac artery in 20% cadavers. Chen et al., [4] evaluated the diameter and the length of the iliolumbar artery at the medial of the psoas major and found that its mean diameter was 2.7±0.6 mm and that its length was 2.2±0.7 cm. Harrington [4] reported that its diameter was 3-4 mm. In our study, the average diameter of the iliolumbar artery, at its origin was 3.5±0.5 mm and the distance between the origin and the bifurcation point was 12.2±5.5 mm. The distance between the origin of the iliolumbar artery and the bifurcation point of the common iliac artery was 38.7±10.6 mm. Harrington [4] reported this distance as 20 mm. This showed that the numeric measurements were similar between studies and that there was no remarkable difference between the people from different ethnic origins in terms of these measurements. In addition, we found that the mean distance between the origin of the iliolumbar artery and the lower edge of the L5 vertebra was 43.2±12.0 mm. We also evaluated its correlation with the obturator nerve, one of the important neural structures which was closely related to the iliolumbar artery, before it divided to the lumbar and the iliac branches and found that the iliolumbar artery passed from the anterior of the obturator nerve in 2 cases (4.8%) and from the posterior of the obturator nerve in 40 cases (95.2%). This study showed that the iliolumbar artery had many different variations. An injury to the iliolumbar artery during surgery may lead to acute haemorrhage or a postoperative haematoma. The anatomical variations of the iliolumbar artery can also be important for harvesting the vascular iliac bone graft. The surgeons should consider that the anatomical variations of the iliolumbar artery may complicate both the anterior exposure of the lumbosacral junction and the posterior sacroiliac fixations.
The iliolumbar artery was seen anterior to the lumbosacral trunk in 30% cadavers (12 cases) , posterior in 54 % (24 cases) and cleaved in 8% (2cases) and the branches of this artery were passing on either side of the lumbosacral trunk to enclose it like a clasp in 8% cadavers (2 cases). The artery clasping or cleaving the lumbosacral trunk was an interesting finding and this was not described by any author earlier.
Safe exposure of iliolumbar veins at L4/ L5 disc junction during anterior approach surgeries is needed [20,21,27.28] since iliolumbar vein communicates with valve less common iliac vein, injury to iliolumbar vein will lead to massive haemorrhage [18-20] though surgically significant relations are not much known, iliolumbar system was demonstrated in every cadaver, it drained the iliacus and the psoas muscles, and the fifth lumbar vertebra. A separate ascending lumbar vein running longitudinally to azygus system was seen [16,17,29] The mean distance of the iliolumbar veins from the inferior vena cava, overall, was 35± 9.9 mm. The mean width of the mouth of the iliolumbar vein was10.7 ± 5.1 mm and the mean angle of obliquity of the vein with respect to the long axis of the common iliac vein was 75.50. due to its length and its variable angle of entry to IVC makes it prone for injuries. Also the variability of tributaries can be cause of bleeding if one of them is missed of ligation. The iliolumbar vein is related between obturator and lumbosacral nerve makes it very significant to dissect ,identify and segregate the structures and ligating all tributaries of iliolumbar vein.