In the literature, there are countless reports on the anatomical variations of the muscles of the forearm. Amongst these, a small cylindrical muscle is frequently seen. It is the accessory head of Flexor Pollicis Longus (FPL) muscle. FPL is one of the deep flexors of the forearm. It takes origin from the grooved anterior surface of the radius and from the adjacent interosseus membrane and gets inserted onto the base of the distal phalanx of the thumb [1]. It has been noted that FPL frequently arises from a variable slip from the lateral border, or more rarely, from the medial border of the coronoid process of the ulna or also from the medial epicondyle of the humerus. This variable slip has also been called as the Gantzer’s muscle or an occasional head [2]. The anatomical variations in which the Gantzer’s muscle might contribute to the median nerve compression in the pronator syndrome have been discussed.
The present study was planned to analyze the AHFPL (Gantzer’s muscles) and its incidence. It is an additional muscle in the forearm which might cause pressure symptoms to the underlying structures, especially to the anterior interosseus nerve.
MATATERIALS AND METHODS
The incidence and the morphology of the AHFPL muscle were studied in 180 upper limbs (90 right and 90 left). The relations of the muscle with the AIN and MN have been examined. The length of the fleshy belly, the tendinous part of the AHFPL and the maximum width of the muscle were measured with the help of a measuring scale. The data which was collected in this study was analyzed and it was expressed as percentage. Wherever required, the data was subjected to a statistical analysis.
OBSERVATIOATIONS AND RESULT
The incidence of the accessory head of the flexor pollicis longus muscle was 51.11% (92 limbs). It was found bilaterally in 33 cadavers (71.73%) and unilaterally in 26 limbs (28.26%), 16 of the right side and 10 of the left side.
The shape of AHFPL was thin and it was fusiform in 77 cases (83.69%) [Table/Fig-1]. It was short, thick and broad at the origin (triangular) in 15 cases (16.31%).
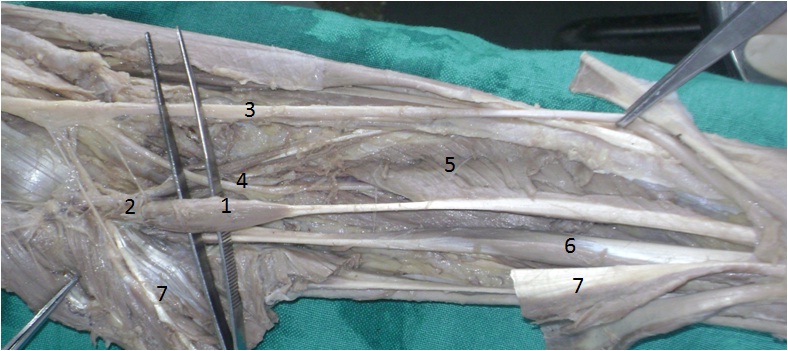
Anterior view of the right forearm 1- AHFPL accessory head of flexor pollicis longus, 2- FPL flexor pollicis longus, 3- FDP flexor digitorum profundus, 4- Median nerve, 5- Anterior interosseus nerve; 6- Flexor digitorum superficialis

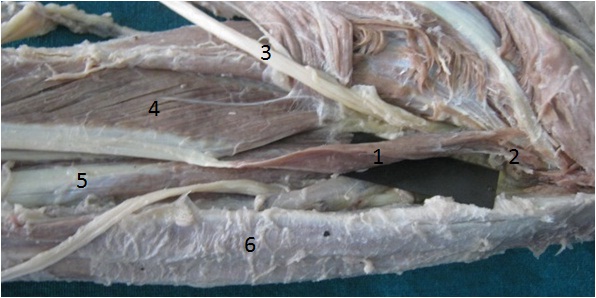
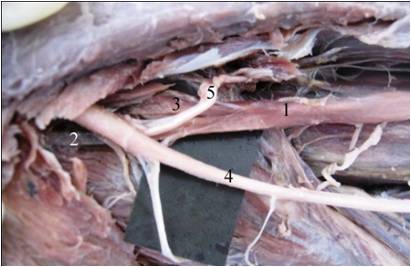
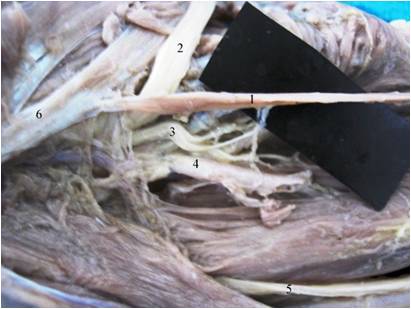
The origin of the AHFPL muscle from the coronoid process of the ulna was observed in 76 limbs (82.60%) [Table/Fig-2], while it was from the medial epicondyle of the humerus in 10 limbs (10.86 %) [Table/Fig-3]. Its origin, which was merged with the fibres of the flexor digitorum superficialis, was seen in only 2 specimens (2.17%). In 4 cases, its origin was by two heads, one arose from the coronoid process of the ulna and other from the medial epicondyle of the humerus [Table/Fig-4].
Anterior view of left forearm showing AHFPL taking origin from coronoid process of ulna. 1- AHFPL accessory head of flexor pollicis longus, 2- coronoid process of ulna, 3- Median nerve, 4- Anterior interosseus nerve, 5- FPL flexor pollicis longus, 6- FDP flexor digitorum profundus, 7- FDS flexor digitorum superficialis
Anterior view of the right forearm showing AHFPL taking origin from medial epicondyle of humerus. 1- AHFPL accessory head of flexor pollicis longus, 2 medial epicondyle of humerus, 3 Median nerve, 4 FPL flexor pollicis longus, 5 FDP flexor digitorum profundus, 6 Flexor digitorum superficialis.
Antero-medial view of left forearm showing the 2 heads of origin of AHFPL. 1- AHFPL accessory head of flexor pollicis longus, 2- Tendinous head from coronoid process of ulna, 3- Muscular head from medial epicondyle of humerus. 4- Median nerve, 5- Anterior interosseus nerve
The insertion of the muscle was in the upper part of the middle third of the forearm. It ended by merging with the medial side of the tendinous part of the flexor pollicis longus muscle. The distance between the point of insertion and the radial styloid process was measured, as shown in the [Table/Fig-5], along with the length of the fleshy belly, the tendinous part, the maximum width of the muscle and the point of insertion of the muscle from the radial styloid process.
Measurements of accessory head of flexor pollicis longus muscle (AHFPL).
| Measurements | Mean ± SD | Min-Max |
|---|
| Length of muscle | 80.47±1.01 | 55-100 |
| Tendon length | 1.90±0.09 | 6-40 |
| Width of muscle belly | 0.78±0.03 | 3-15 |
| Point of I from the RSP | 139.36±1.35 | 115-160 |
It was observed that the AHFPL was innervated by the branch from the AIN in 74 cases (80.43%) and from the branch of the median nerve in 18 cases (19.56 %). It was further noted that the anterior interosseous nerve was present anterior to the muscle in 9 cases (9.78%) and that it was present posterolateral to the muscle in 83cases (90.21%) [Table/Fig-6].
Antero-medial view of left forearm showing relations of AHFPL. 1- AHFPL accessory head of flexor pollicis longus, 2- Median nerve, 3- Anterior interosseus nerve; 4- Ulnar artery, 5- Ulnar nerve, 6- FDS flexor digitorum superficialis.
DISCUSSION
The occurrence of the belly of the AHFPL is possibly from the development of the common flexor mass in the embryo, which differentiates into the superficial and the deep layers. The deep layer further develops into the flexor digitorum profundus, the FPL, and the pronator quadratus muscle, but an incomplete differentiation creates the AHFPL [3, 4].
There are reports on the incidence and the morphology of the AHFPL muscle and its clinical importance. The incidence of AHFPL was found to be 66.7% by Oh et al., 66.6% by Hemmady et al., 62.1% by Mahakkanukrauh et al, 55% by Jones et al., and Shirali et al., 52% by A1-Qattan, 45% by Dellon and Mackinnon and 51.9% by Feray G et al., [5–11]. In our study, the incidence of the AHFPL muscle was seen in 51.11% cases. Our findings were comparable with the findings of the most of the studies.
Oh et al., observed it to be bilateral in 50% cases and to be unilateral in 33% cases. Mahakkanukrauh et al observed it to be bilateral in 75.3% cases and to be unilateral in 24.7% cases. Jones et al found it to be bilateral in 58.4 % cases and to be unilateral in 33.4 % cases. Feray G et al., found it to be bilateral in 74% cases and to be unilateral in 26% cases. In our study, it was found to be bilateral in 71.73% cases and to be unilateral in 28.26% cases [5, 7, 4, 11].
The origin, shape, relations and measurements of the muscle were compared with the previous findings, as shown in [Table/Fig-7].
CP of U - Cornoid process of ulna, ME of H - Medial epicondyle of Humerus, From FDS - From Flexor Digitorum Superficialis.
| Details | Present study | Oh et al | Mahakkanukrauh | Hemmady et al | Jones et al | A1 Qattan | Feray G et al |
|---|
| Origin | CP of U | 82.60% | 87.5% | 23.5% | 16.6% | ---- | ---- | 81.5% |
| ME of H | 10.86% | 10.4% | 74.5% | 55.5% | ---- | 85% | 18.5% |
| From FDS | 2.17% | 2.1% | 2% | ---- | ---- | ---- | ---- |
| Shape | Papillary | ---- | 62.4% | ---- | ---- | ---- | ---- | 29.6% |
| Fusiform | 83.69% | 18.8% | 98% | ---- | ---- | ---- | 70.4% |
| Slender | ---- | 18.8% | 2% | ---- | ---- | ---- | ---- |
| Triangular | 16.31% | ---- | ---- | ---- | ---- | ---- | ---- |
| Measurements (mm) | Width | 6 | 7 | 6.7 | 10-25 | ----- | ----- | 6.99 |
| Length of muscle belly | 80.47 | ---- | ---- | 50-80 | 68 | ---- | 71.25 |
| Tendon length | 19.04 | ---- | ---- | ---- | 11.7 | ---- | 20.7 |
Regarding the relationship between the AHFPL and the Anterior Interosseous Nerve (AIN), we found the nerve to pass posterior to the belly in 90.21% cases and in 9.78% cases, it passed anterior to the muscle. Mangini [12]; Hemaddy et al., found the nerve posterior to the muscle; Jones and Abrahams; Shirali et al., Oh et al., found the nerve to pass posterior to the belly [6, 4, 8, 5]. This also differed from the reports of Al-Qattan and Dellon and Mackinnon [9, 10], who had stated that the nerve had passed anteriorly in front of the muscle belly.
Repetitive trauma to the forearm and structural anomalies can cause the anterior interosseous nerve syndrome [13]. Paralysis of the AIN due to a compression in the forearm is also called as the Kiloh-Nevin syndrome [14–18]. The AIN innervates the FPL, PQ and FDP. The relationship with the AIN has been studied by several authors [4, 8–10, 12]. Although this muscle has been suspected to be responsible for the KilohNevin syndrome, clear case reports on this are rare.
A complete AINS would occur when the whole nerve passes posteriorly underneath the belly of the AHFPL, causing weakness in the FPL, in the FDP of the index and the middle fingers, and in the pronator quadratus muscles.
An incomplete AIN syndrome may also occur, as has been reported by Tabib et al., [19]. The incomplete type is likely to occur where only the medial branch of the AIN to the FDP which passes underneath the belly is compressed, whereas the lateral branch to the FPL which runs alongside the belly, does not compressed.
According to Levangie and Norkin [20], the architecture of the whole muscle may be important in determining the muscle function. The structural variations affect not only the overall shape and size of the muscle but also the function of the skeletal muscle, especially the range of motion. The function of the flexor pollicis longus (which has unipinnate muscle fibres) is in direct opposition to the additional head of the flexor pollicis longus (which is made up of fusiform muscle fibres). Hemmady [6] has also stated that the presence of the occasional head has to be borne in mind during the anterior approaches to the proximal radius and the elbow joint, as also during decompressive fasciotomies for the compartment syndrome of the forearm.
CONCLUSION
The present study substantiates the pragmatic significance and the surgical importance of the Gantzers muscle, which if present, has far reaching implications which are relevant to the median nerve compression in the pronator syndrome, as well as to the anterior interosseous nerve syndrome. Moreover, this study carries importance for surgical interventionists, whenever they approach the proximal head of the radius or the elbow joint. The findings of the present study could prove to be beneficial for the operating surgeons/ orthopaedicians while they perform decompressive fasciotomies for the compartment syndrome of the forearm. Notwithstanding, the structural/ morphological variations which have been reported must be kept in mind as regards the functionality of the muscle (especially by the range of motion).