The aesthetic needs of the patients are increasing day by day. Each and every patient wants a beautiful smile. To achieve this, not only the teeth but also the gingiva plays an important role. Gingival depigmentation as an aesthetic procedure, improves the smile and the overall appearance of an individual. The colour of the pigmented gingiva varies from light to dark brown or black. The skin tone, texture and colour differ in various races and regions [1–4]. The pigmentation of the gingiva, when it is not related to the skin complexion, is a dampening factor in an otherwise acceptable smile window.
The discolouration of the gingiva may be due to a wide variety of lesions and conditions. It may range from physiologic reasons (e.g. racial pigmentation) to manifestations of systemic illnesses (e.g. Addison’s disease) to malignant neoplasms (e.g. melanoma and Kaposi’s sarcoma). It is essential to understand the cause of a mucosal pigmentation before planning the treatment of such lesion [5]. The physiological gingival melanin hyperpigmentation usually does not present as a medical problem, but the patients may complain that their black gums are unaesthetic. This problem is aggravated in the patients with a “gummy smile” or an excessive gingival display while they smile or talk [6].
The physical and chemical changes which are induced by freezing lead to cell destruction and tissue death. Most of the vital tissues freeze at approximately – 2 degree Celsius and ultra low temperatures of less than – 20 degree Celsius result in total cell death [9,10]. The apparatus which was used to generate a cryogenic temperature for surgical use over the past 130 yrs reflected the technology which was available at that time. A mixture of salt ice was used originally by Arnott in his pioneering work in 1851. A cryoprobe with a cooling agent did not appear until the 1950s, when a mixture of solid CO2 and water was used to provide a cooling source. The liquid nitrogen cryoprobe did not come into use until Cooper’s study was done in the early 1960s. Later in that decade, the high pressure type of cryoprobe which utilized a joule Thompson expansion came into use. The high pressure cryoprobe and the liquid nitrogen spray form the bulk of the equipment today [10,1].
A colourless, non chlorofluorocarbon (CFC), non flammable gas, 1,1,1,2 Tetrafluoroethane is usually used as a refrigerant and in electronic circuits. There are several human and animal toxicology studies which have evaluated the safety of Tetrafluoroethane [11–17]. Tetrafluoroethane (TFE) has recently been introduced in dentistry, in the field of periodontics for depigmentation and it is being used in dermatology as a skin cooling medium in the laser therapy [7,18].
It has been used in the field of endodontics for cold pulp testing for the full crowned or natural teeth and in the orthodontics treatment to facilitate the seating of the Nickel titanium expansion loops [2]. An accidental hypopigmentation of the skin was reported while work was done with Tetrafluoroethane, possibly made to use this agent for depigmentation of gingiva. The present study was undertaken to compare the gingival abrasion technique with the newly introduced, cryogen Tetrafluoroethane for the depigmentation of the gingiva.
MATERIALS AND METHODS
Ten patients who were concerned with their aesthetics, were treated with two different techniques at the Department of Periodontics, Manipal College of Dental Sciences, Manipal University, Manipal, India. In the present study, the patients who complained of ‘black gum’, which was not relative to their skin complexions and who were keen to get it corrected, were taken into consideration. The criteria for the selection of the patients in the present study were the aesthetic considerations in the periodontally healthy patients. The patients who were treated in this study were enrolled in the period from 2008 to 2009.
A detailed medical history which included pregnancy, breast feeding, systemic diseases which were associated or not associated with the gingival melanin pigmentation, malignancy, medications, uncontrolled diabetes and the adverse reactions to cryosurgery were taken. The relative contraindications were cold intolerance and cold utricaria. A personal history regarding the smoking habits of the patients was also recorded. Each patient signed a written informed consent prior to his/her participation in the study. The study was performed in accordance with the Helsinki Declaration 1975, as it was revised in 2000. The study protocol was reviewed and approved by the institutional ethical committee of Kasturba Hospital, Manipal University, Manipal, India.
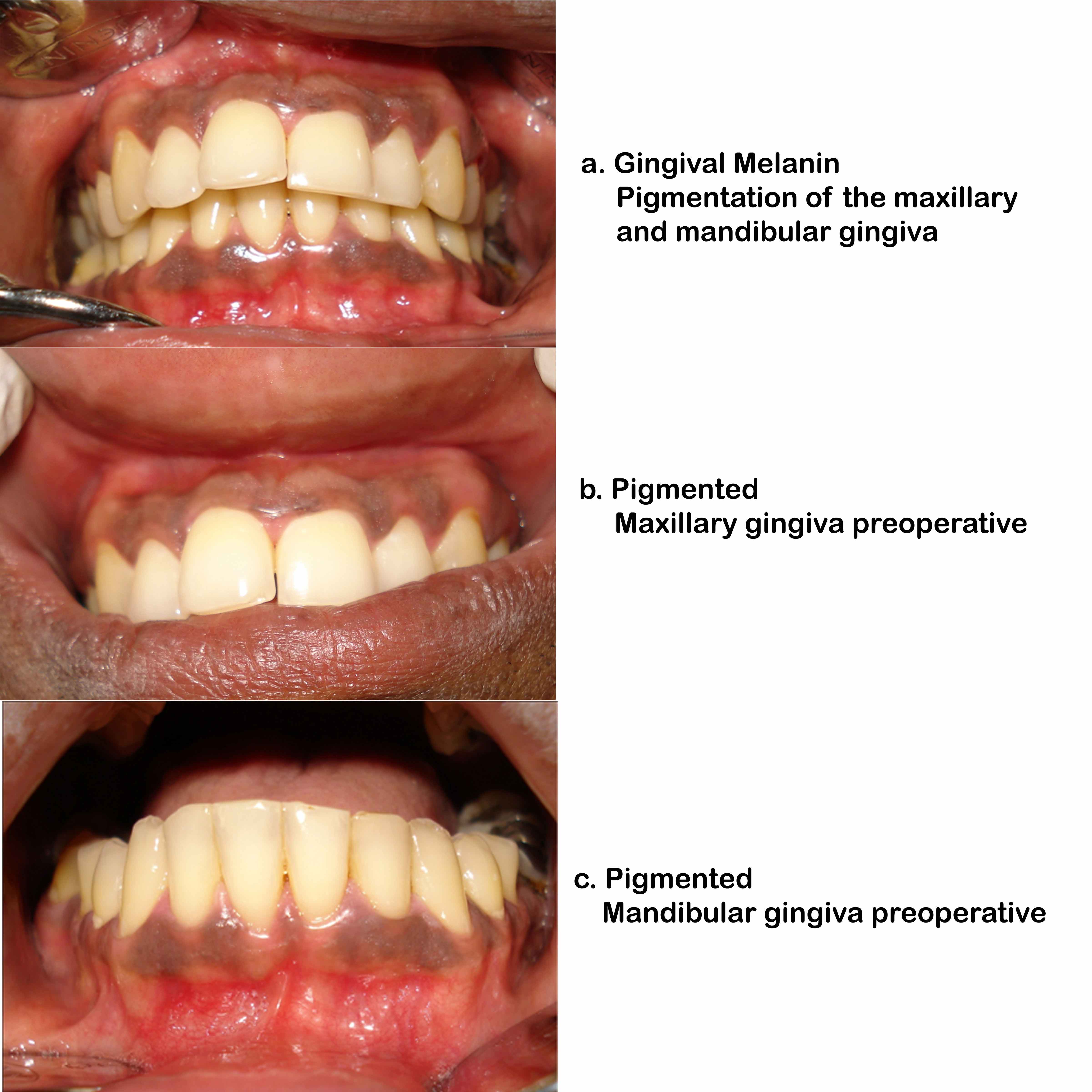
Detailed extra oral/intra oral examinations which included the evaluations of the skin pigmentation, the perioral pigmented lesions and the characteristics of the shape, colour, surface and borders of the gingival melanin pigmentation were recorded. Before undertaking any of the depigmentation procedures, all the patients underwent a full mouth scaling, following which oral hygiene instructions were given to them. To assess the gingival pigmentation, a new index was developed by us, the Gingival Pigmentation Index (GPI) [Table/Fig-1]. The patients were randomly selected for the treatment by using the coin toss method. The maxillary anterior gingival pigmentation was treated by using Tetrafluoroethane. The mandibular anterior area was treated with the gingival abrasion technique by using a coarse flame shaped bur [Table/Fig-2a-c].
Gingival depigmentation index
| 0 | Absence |
| 1 | Spots of brown to black |
| 2 | Brown to Black patches but not diffuse |
| 3 | Diffuse brown to black pigmentation marginal and attached |
Clinical Procedures for depigmentation and post operative changes
For the gingival abrasion technique, a slow speed, micro motor hand piece with doughnut shaped coarse diamond points which were attached to the conventional motor with a water connection and a local anaesthesia injection (2% Lidocaine Hydrochloride with 1,00,000 Adrenaline which was manufactured by ASTRA Company, India.) were used. A periodontal dressing was used to cover the wound. For the cryosurgical technique, a local anaesthetic spray (10% Xylocaine) was used to anaesthetize the area. The Tetrafluoroethane cryogen spray was dispensed into a can and a sterile cotton piece was used to carry it to the site.
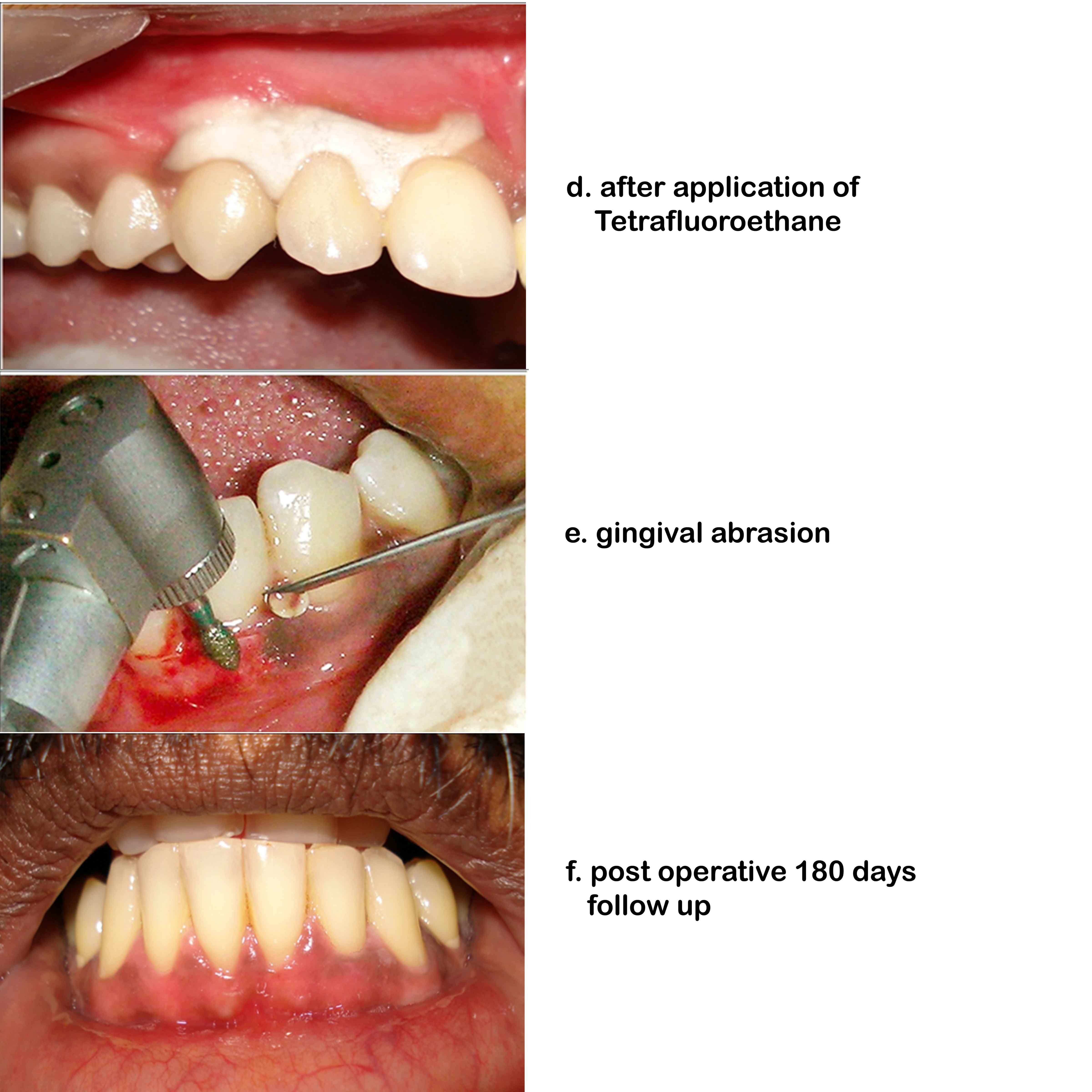
The treatment with the cryosurgical technique: Before the cryosurgical application, the pigmented area was isolated and air dried. A topical anaesthesia with a 10% Xylocaine spray was used to minimize the discomfort. Tetrafluoroethane (TFE) was sprayed on a cotton swab, which was immediately rolled gently over the pigmented area to include the papillae as well [Table/Fig-2d]. A freezing zone was continuously maintained for 30 to 40 seconds in each area by rolling the dampened swab continuously at the site. This technique was continued along the pigmented gingiva. The procedure took about 15-20 minutes. The patients were prescribed analgesics to take if there was any pain.
The treatment with the gingival abrasion technique: Before starting the procedure, the area which had to be operated was infiltrated with a local anaesthetic agent (2% Lignocaine with 1: 1, 00, 000 adrenaline). After the anaesthesia was obtained, a drop of the local anaesthetic agent was deposited into each papilla which was involved. This increased the turgor of the gingiva and it made it easier to abrade.
A spray of saline was constantly directed on the rotating points during their use. An accelerated speed ensures a smooth, rapid operation, while the stream of saline provides a temperature control and it prevents clogging of the burs [Table/Fig-2e]. The procedure was carried out until the underlying soft connective tissue was exposed. Then, the area was mopped with a wet gauze to stop the bleeding. Once the bleeding had subsided, a periodontal dressing was placed over the operated area. Post operative instructions were given, to avoid eating hot and spicy food stuffs to avoid the bleeding. The patients were asked to take analgesics if there was any pain.
The patients were recalled on the 30th, 90th and the 180th days post operatively. Each case was photographed. Standard digital photo images were obtained. The head of each patient was positioned and stabilized before the photographs were taken. The digital images were taken by using a standard magnification and a distance of 38cms. The total area of the gingival pigmentation was traced and measured with an image-analyzing software (Image warp 2.1 build by A and B software). The statistical analysis was done using Freidman’s test. The patient satisfaction was assessed by using a simple questionnaire. A visual analogue scale (1-10cm scale) was used to assess the pain.
The gingival pigmentation was assessed by a single examiner who was masked to the treatment group to which a patient was assigned. Fifty dental students who had gingival melanin pigmentation were used to calibrate the examiner. The examiner evaluated all the dental students on two separate occasions, 48hrs apart. The calibration was accepted if all the recordings could be reproduced with the same scoring by the examiner.
RESULTS
With the rotary technique, immediately after the completion of the treatment, the gingiva appeared raw with visible bleeding points. Since the periodontal dressing was placed, the clinical changes which occurred during the healing were not observed.
No significant clinical changes were noticed immediately after the removal of the cryoprobe, for the evaluation of the healing postoperatively. But the areas became red within half an hour after the procedure. On the first day, the tissue necrosis became evident. In 4-5 days time, the whitish necrosed gingival tissues sloughed off from the underlying tissue.
At the end of 1 week, the gingiva revealed a red colour without any clinically visible gingival pigmentation, irrespective of the technique which was followed. On the 30th day, in 4 cases [Table/Fig-3] which were treated by the gingival abrasion technique, a spotted melanin pigmentation was observed. But the patients refused a retreatment with the gingival abrasion technique. 3 out of the 10 cases which were treated by cryotherapy revealed very minimal repigmentation GPI 1. These 3 patients were willing to undergo a retreatment by using cryotherapy . The cryotherapy was repeated in these spots of the melanin pigmentation.
Tabulated values of the depigmentation procedure
| 30days | 90 days | 180 days | 2 days |
|---|
| Patients | Cryosurgery | Abrasion | Cryosurgery | Abrasion | Cryosurgery | Abrasion | Cryosurgery | Abrasion |
|---|
| 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 |
| 2 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 2 |
| 3 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 2 |
| 4 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 2 |
| 5 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 2 |
| 6 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 |
| 7 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 |
| 8 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| 9 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| 10 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
On the 90th day, in 7 out of the 10 cases which were treated by the gingival abrasion technique , a repigmentation was observed GPI – 1 [Table/Fig-1]. However, the gingiva of these cases which were treated with cryotherapy remained pink in colour.
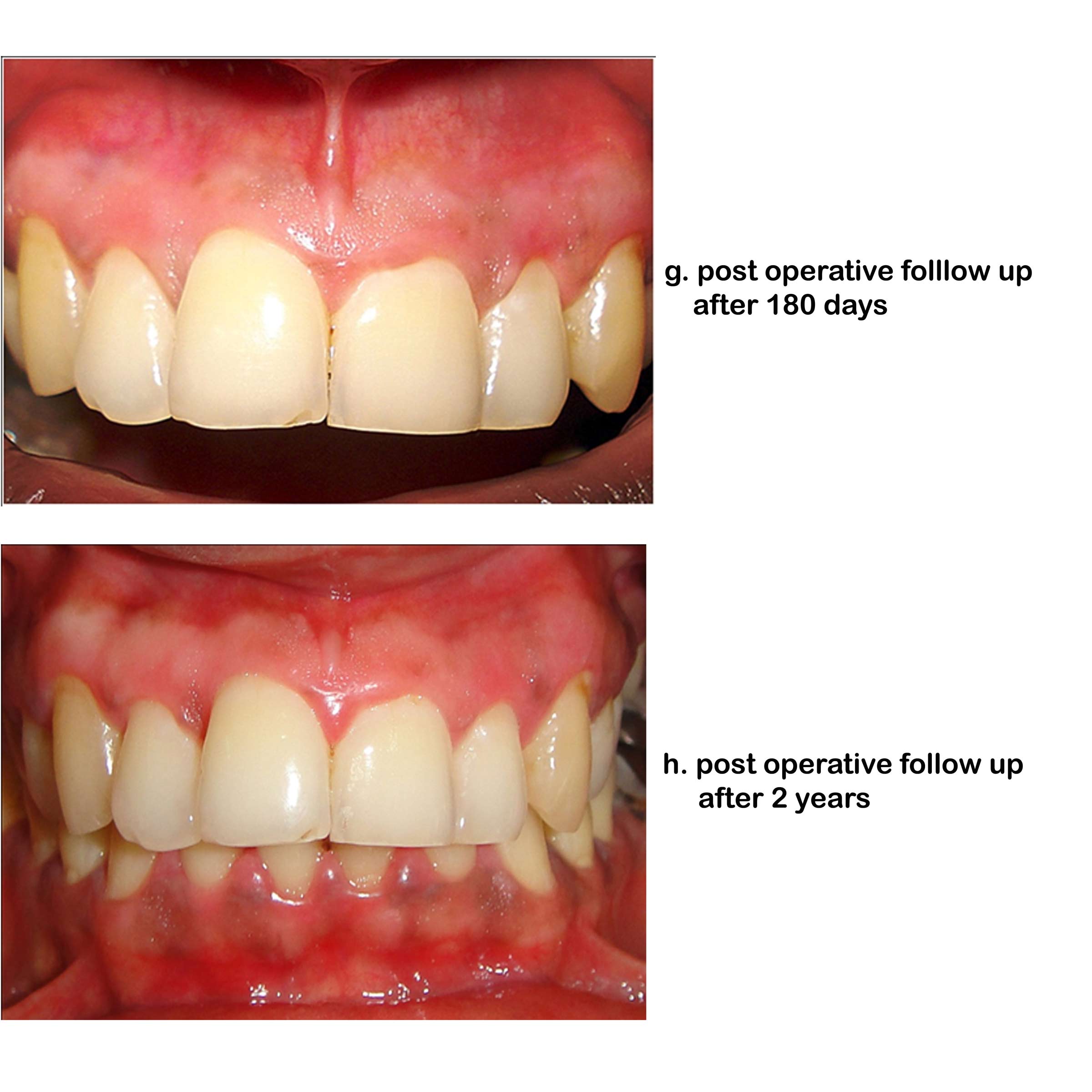
On the 180th day, all the cases which were treated with the gingival abrasion technique showed spots and streaks of the melanin pigmentation GPI 1 [Table/Fig-2f]. One of the ten cases which was treated by cryotherapy revealed spots of the melanin pigmentation GPI 1, while all the other cases remained pink [Table/Fig-2g].
After 2 years, the cases which were treated with tetrafluoroethane showed no unaesthetic repigmentation [Table/Fig-2h]. One of the ten cases revealed spots of the melanin pigmentation GPI 1 (p<0.001) [Table/Fig-3],[Table/Fig-4] Mild pain and discomfort were seen immediately post operatively in the TFE group. All the patients were aesthetically satisfied.
| Friedman Test | | |
| Test Statistics | | |
| N | 10 |
| Cryosurgery | chi square test | 3.8 |
| P | 0.284 |
| N | 10 |
| Abrasion | chi square test | 19.985 |
| P | <0.001 |
| | Vhs |
In the present study, the operator found that, to perform the cryosurgical method of the depigmentation, approximately 15 to 20 minutes per patient was required. The local anaesthetic spray was enough to control the procedural discomfort. This procedure required fewer instruments and less tissue manipulation during its performance. Following the treatment, the healing was satisfactory, even though a periodontal dressing was not used and there was no need of analgesics, as the patients did not experience any pain.
The technique which used rotary diamond points to depigment the gingiva took 35 to 45 minutes per patient to perform. It required the injection of a local anaesthetic before its start, a periodontal dressing and analgesics following the treatment. The discomfort which was caused with the use of the rotary device was unavoidable. Though the gingiva appeared normal in colour, following the treatment, an early reappearance of the melanin pigmentation was noticed. [Table/Fig-5].
VAS- Visual Analogue Scale
| Case description | | | | | | | | | | |
|---|
| Information | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 |
|---|
| Gender | Male | Female | Male | Male | Male | Female | Female | Female | Female | Female |
| Age (years) | 32 | 18 | 27 | 22 | 21 | 20 | 22 | 26 | 28 | 19 |
| Working Status | Factory Worker | Student | Salesman | Student | Student | Student | Unemployed | Teacher | Teacher | Unemployed |
| Gummy smile | slightly | severe | No | No | slightly | slightly | no | no | Slightly | Slightly |
| Smoking Habit | No | No | No | No | No | No | No | No | No | No |
| Pigmentation before treatment | GPI 3 | GPI 3 | GPI 2 | GPI 3 | GPI 3 | GPI 2 | GPI 3 | GPI 3 | GPI 2 | GPI 3 |
| Additional Treatment | Scaling | Scaling | Scaling | Scaling | Scaling | Scaling | Scaling | Scaling | Scaling | Scaling |
| Pain/Discomfort |
| Abrasion | yes (VAS 3-4) | yes (VAS 4-5) | yes (VAS-3-4) | yes (VAS-3-4) | No (VAS-0) | yes (VAS-2-3) | yes (VAS-3-4) | yes (VAS-4-5) | yes (VAS-3-4) | yes (VAS-2-3) |
| Cryosurgery | No (VAS-0) | No (VAS 0) | No (VAS-0) | No (VAS-0) | No (VAS-0) | yes (VAS-2-3) | No (VAS-0) | yes (VAS-3-4) | No (VAS-0) | No (VAS-0) |
| Follow up period (months) | 24 | 26 | 26 | 24 | 22 | 20 | 27 | 24 | 25 | 20 |
When the overall results were analyzed, clinically and on the basis of the patient response, the cryosurgical mode seemed to be favourable, as it was associated with less or no pain, the healing was faster, and the gingiva remained depigmented at the end of 2 years.
DISCUSSION
There are wide variations in the gingival colour in healthy persons. Most of the times, these variations are in the form of blackened spots and are caused by the presence of melanin pigments. In some cases, the presence of a pigmentation indicates nothing more than a physiological phenomenon, whereas in other cases, it is pathologic in nature. As far as the physiologic pigmentation is concerned, the gingival colour variations are dependent on the intensity of the melanogenesis, the degree of epithelial cornification, the depth of epithelialization and the arrangement of the gingival vasculature [19]. So far, only very few literatures have been published regarding the practical methods of treatment of pigmented gingiva, without promising results.
The techniques that were tried in the past to treat gingival pigmentation included chemical cauterization which was tried by Hirshfield I and Hirshfield L [3], gingivectomy which was tried by Dummett CO, Bolden TE [20] and Bergamaschi O et al. [21], the scrapping procedure which was tried by Manchandia in 1979, and abrasion of the gingiva which was tried by TK Pal et al. [22]. The recent techniques which are being used for the gingival depigmentation in practice are cryotherapy by Tal Haim et al. [4] Chin - Jyh Yeh [1], free gingival autograft technique by Tamizi M and Taheri M [23] and laser therapy by Trelles et al [24] out of these lasers and cryotherapy have achieved satisfactory results.
In the present study, the patients found that, as compared to the rotary technique, the cryosurgical management was well – tolerated. All the participants who underwent the cryosurgical depigmentation were highly satisfied with the results and they accepted the procedure as simple and effective.
Cryosurgery is usually applied with a gas expansion system that is expensive, and it is not widely in use in the dental practice. There have been reports on the cryosurgical treatment of a variety of oral lesions by using liquid nitrogen, but both the gas expansion cryosurgical system and the liquid nitrogen which is applied with cotton swabs are not easily obtainable in most of the clinics. The loss of gas due to leakage and evaporation and the risk of accidents are other concerns in its storage [2]. Furthermore, a risk of cross infection is another disadvantage of the dipping method.
In addition, the laser depigmentation techniques have been associated with damage to the underlying alveolar bone and subsequent gingival fenestration. In this regards, the laser depigmentation procedures require measures for avoiding the damage which is done to the adjacent tissues like the acrylic barriers and the anodized periosteal elevators, to effectively and completely remove the pigmentation.
In contrast to laser surgery and the conventional cryosurgery methods, the Tetrafluoroethane cryosurgery serves as an inexpensive method and Tetrafluoromethane has been found to be an easy-to-use store and transport cryosurgery agent. In addition, the lack of bleeding and scar formation, its application without a regional anaesthesia, sutures or dressing, the ease of application of the cryogen at the papillary area by using a small cotton pledget, the added advantage of the depth control by using the time factor [25] of maintaining the cryogen for 30–40 sec at the site and the need of no complicated instruments, makes the Tetrafluoroethane cryosurgery superior to the scalpel, Laser [26], and the conventional cryotherapy procedures in many aspects.
The present study did not show any significant differences in the healing of the depigmented areas of the gingiva, even though with the rotary technique, the healing was associated with increased pain and inflammatory changes as compared to those which were associated with the cryosurgical technique. In both the procedures, the evaluation on the 30th day revealed restoration of the normal features of the gingiva without any scar formation. Thus, the healing of the depigmented gingiva was uneventful, irrespective of the techniques which were used.
The areas where the melanin pigments were eliminated with the rotary diamond points, the reappearance of the pigmentation which was reported, was observed after 30 days following the treatment. In the earlier studies which were done by Ginwalla [7], Dummett CO, Bolden TE [20] and T.K Pal [22], it was reported that there was repigmentation after 15, 24 and 33 days respectively.
The data on the gingival pigmentations which were treated by cryotherapy revealed 3 cases of mild areas of repigmentation without any cosmetic significance on the 30th day of the observation, whereas in the rest of the patients, the gingiva remained depigmented till the end of the study period. The previous studies which were done by Tal Haim et al. [4] and Chin – Jyh Yeh [1] on the cryosurgical mode of the gingival depigmentation reported no evidence of a repigmentation during the initial follow up period of 20 and 48 months respectively. But the continuation of the study which was done by Tal Haim et al. [4] reported two cases with limited areas of repigmentation without any cosmetic significance after 3 years of the treatment.
In these areas where the melanin pigmentation did not occur, either “migration” of the melanocytes did not occur or the melanocytes that migrated were in an inactive state due to the inhibition of their tyrosinase system. They were thus unable to produce melanin pigmentation during the observation period according to Bandish LK [19]. The minimum temperature which is needed for the cell damage is cell-specific, and the melanocytes are very sensitive to a low temperature [-4°C to -7°C] where the cell death can occur [2]. At the ultralow temperature (- 47°C × 30 seconds) which was created by the cryosurgical technique, a complete epithelial destruction and elimination of the gingival epithelium along with the melanocytes, was achieved [9, 25].
The less number of patients which was seen with a delayed reappearance of the melanin pigmentation and the number of areas and the degree of pigmentation remained same throughout the study. The cryosurgical technique was more acceptable to the operator as well as to the patient. The healing after surgery was uneventful and no scar was formed.
SUMMARY AND CONCLUSION
The gingival depigmentation which is achieved by using the simple Tetrafluoroethane cryosurgery is more acceptable and suitable as compared to the rotary diamond point method. The rapid wound healing and the longer period of reappearance of the pigmentation are the added advantages of the TFE usage. Tetrafluoroethane is better and more effective in the elimination of gingival melanin pigmentation.