Neonatal Meningoventriculitis Due to Proteus Mirabilis – A Case Report
Deepak Juyal1, Vyas Kumar Rathaur2, Neelam Sharma3
1 Senior Demonstrator, Department of Microbiology & Immunology,
2 Assistant Professor, Department of Pediatrics,
3 Professor and Head, Department of Microbiology & Immunology, Veer Chandra Singh Garhwali Government, Medical Sciences & Research Institute, Srinagar Garhwal, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mr. Deepak Juyal, Senior demonstrator, Department of Microbiology & Immunology, Veer Chandra Singh Garhwali Government, Medical Sciences & Research Institute, Srinagar Garhwal-246174, Uttarakhand, India.
Phone: +919719769559
E-mail: deepakk787@gmail.com
A five day old full term born baby was admitted to our Neonatal Intensive Care Unit with seizures, opisthotonous posture and was icteric upto thigh. Baby had a three day history of poor feeding, lethargy and abnormal body movements. Mother was a 29 years old primigravida and had a normal vaginal delivery at home. Sepsis profile of the patient was requested, lumbar puncture and ventricular tap was performed. Patient was put on third generation cephalosporins, aminoglycosides and phenobarbitone. Culture and sensitivity report of blood, Cerebro spinal fluid and ventricular fluid showed Proteus mirabilis. Computerized Tomography scan showed a large parenchymal lesion in the right frontal lobe and diffuse ependymal enhancement along both the lateral ventricles suggestive of meningoventriculitis. We hereby present a fatal case of neonatal meningoventriculitis due to Proteus mirabilis.
Proteus mirabilis, Meningoventriculitis, Cerebral abscess, Meningitis
INTRODUCTION
Proteus mirabilis is widely distributed in nature as saprophyte and is often considered to be implicated in contamination and colonization. It is occasionally isolated in severe infections [1]. The organism is encountered worldwide as an uncommon etiological agent in neonatal sepsis and meningitis [2]. Early institution of third generation cephalosporins combined with aminoglycosides and a brain CT scan is recommended in case of neurological sepsis caused by this organism. A fatal case of P.mirabilis meningoventriculitis complicated by cerebral abscess confirmed microbiologically and later by brain CT, is reported herewith.
CASE REPORT
A five day old full term born baby girl was admitted to our Neonatal Intensive Care Unit (NICU) with seizures. She had three days history of poor feeding, lethargy and abnormal body movements and two days history of jaundice. Her mother was a 29 years primigravida who had a vaginal delivery at home, with history of premature rupture of the membrane for 48 hours. On examination the baby was icteric upto thigh, lethargic, hypertonic and had paradoxical irritability. Suckling reflex was poor and there was slight bulging of anterior fontanel. Vital signs were stable. Full sepsis profile was requested and patient was put on intravenous (IV) ceftazidime, amikacin and phenobarbitone.
Peripheral WBC count was 19,300 cells/μl with differential count being 69% neutrophils, 16% lymphocytes, 6% monocytes and 9% eosinophils. The C reactive protein (CRP) was positive; 67mg/ lt. Cerebro spinal fluid (CSF) was turbid and showed 560 WBC/μl with 79% neutrophils, 21% lymphocytes and few RBC’s. CSF protein was 380 mg/dl and glucose 11 mg/dl (parallel blood glucose 97mg/dl). CSF gram staining showed many pus cells and many gram negative bacilli (GNB). Latex antigen test for Hemophilus influenzae type B, Neisseria meningitidis, Escherichia coli, Streptococcus pneumoniae and Streptococcus group B was negative.. The brain CT was deferred at this stage as patient was unstable. On third day of admission she developed generalized hypertonia, hyper reflexia and anterior fontanelle bulging persisted. Respiratory efforts were spontaneous but ineffective. Pupils were dilated and sluggish and prognosis was poor. Both CSF and blood culture showed P.mirabilis with similar antimicrobial sensitivity pattern. Isolate was sensitive to amikacin and ceftazidime hence same treatment was continued. Later that day patient developed further convulsions and went into cardio-respiratory arrest. Cardio pulmonary resuscitation (CPR) was done after entubation and patient revived. Her condition remained unchanged the next day. Ventricular tap was done and was sent for biochemical and microbiological investigations. Gram staining of ventricular fluid showed many pus cells and few GNB. Later ventricular fluid also showed P.mirabilis and the antibiogram of the organism was similar to the isolate from blood and CSF. Brain CT was performed on day 12th of admission which showed a large hypodense parenchymal lesion in the right frontal lobe and thalamus-basal ganglia region. A multiloculated hyperdense lesion with calcifications along the frontal horn of the left lateral ventricle and diffuse ependymal enhancement along both the lateral ventricles was seen [Table/Fig-1].
Image showing a large hypodense parenchymal lesion in the right frontal lobe and diffuse ependymal enhancement along both the lateral ventricles.
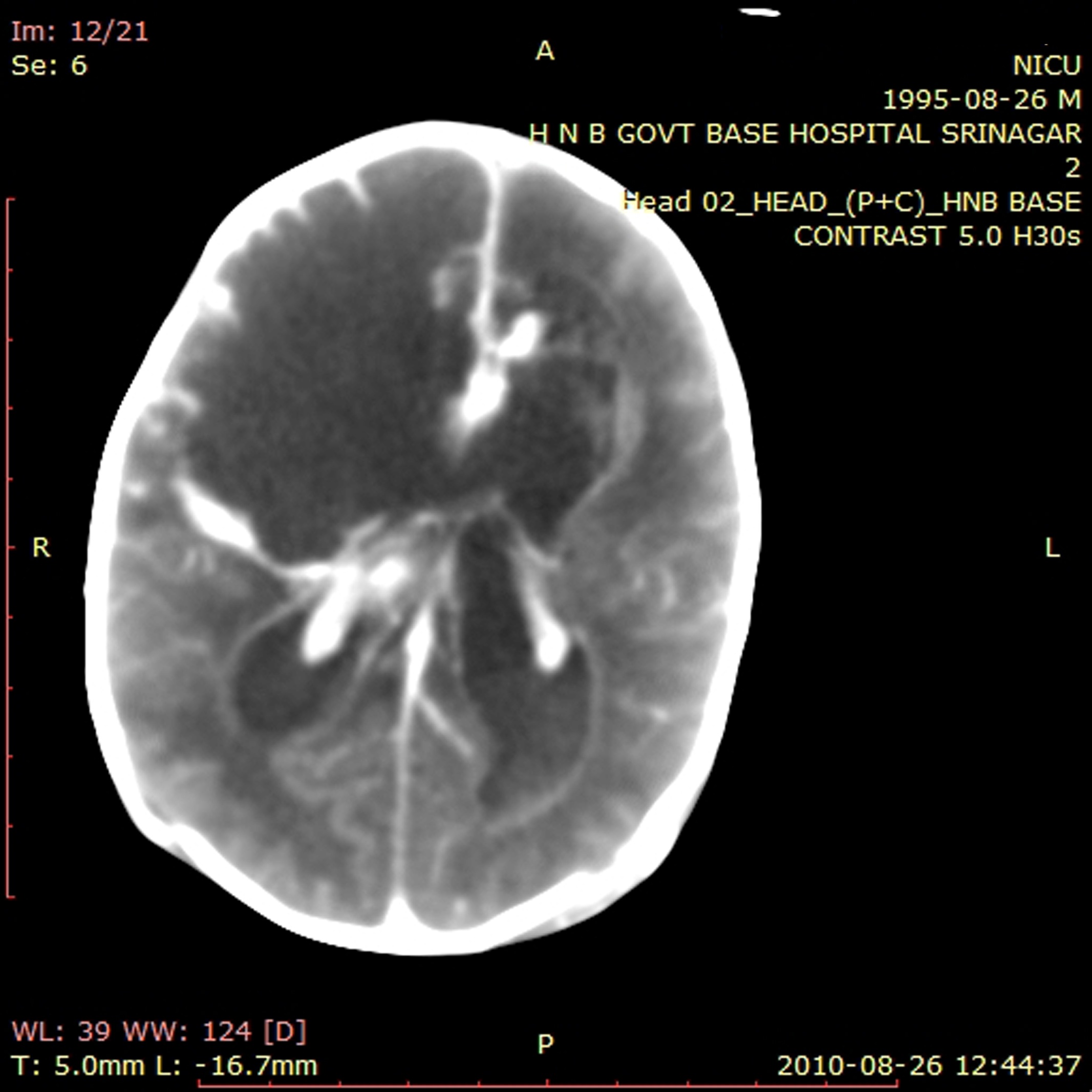
These findings associated with laboratory reports pointed towards early right frontal lobe abscess with meningoventriculitis and subependymal abscess. The parents were informed of the severe brain damage and poor prognosis. On day 15th of admission patient died following irreversible multiple organ failure.
DISCUSSION
P. mirabilis is a ubiquitous saprophytic bacillus and is part of the normal flora of human gastro intestinal tract (GIT). Several cases of bacteremia, meningitis, meningoencephalitis, and cerebral abscess due to P.mirabilis have been reported [2,3,4,5,6].
P. mirabilis was responsible for 4% of gram negative bacterial meningitis seen in one American center over a 21 year period [7]. It was reported to be a infective agent in 7.1% cases of neonatal bacterial meningitis in a teaching hospital in Taiwan over a 13 year period [8]. In an unusual outbreak in a hospital nursery, P.mirabilis was responsible for bacteremia and meningitis in newborns [5]. This organism is also an uncommon cause of brain abscess in infants and children [9,10].
Neonatal sepsis and meningoventriculitis even though initially has nonspecific mild clinical symptoms, it may turn life threatening and delay in treatment result in poor prognosis and higher mortality. Higher case fatality rates have been reported for gram negative organisms than for gram positive organisms [11,12]. Third generation cephalosporins and aminoglycosides have been used in treating gram negative neonatal sepsis and meningitis [13].
Brain abscess and ventriculitis in neonates is rare and usually occur as complication of bacterial meningitis or bacteremia. Maternal factors can be an important source. Symptoms of seizures, signs of sepsis and bulging fontanelles are frequently seen in neonatal brain abscess [14]. Route of infection in our patient was probably maternal as she gave history of premature rupture of the membrane and the clinical features appeared on second day of life. Sepsis and meningoventriculitis due to P.mirabilis in this case was further complicated by brain abscess which unfortunately had a poor outcome. CT findings represented brain abscess on the right frontal lobe and subependymal abscess along both the ventricles that has caused tissue destruction and necrosis. Though the antimicrobials were administered early but the patient could not recover which may have been due to the severity of the infection. Early CT scan was not possible due to the unstable condition of the patient.
CONCLUSION
P. mirabilis should be considered as a cause of sepsis, meningitis and meningoventriculitis among neonates. Brain CT is warranted for early diagnosis, proper management and good prognosis of the patient. Prompt, aggressive and prolonged antibiotic therapy should be considered.
[1]. Champs C. de, Bonnet R, Sirot D, Chanal C, Sirot J, Clinical relevance of Proteus mirabilisin hospital patients: a two year surveyJournal of Antimicrobial Chemotherapy 2000 45:537-539. [Google Scholar]
[2]. Zainab K, Azian AA, Quazi MH, Humairah ASC, Isolation of Proteus mirabilis from sever neonatal sepsis and central nervous system infection with extensive PneumocephalusEur J Pediatr 2003 162:644-45. [Google Scholar]
[3]. Watanakunakorn, C, Perni S. C., Proteus mirabilis bacteremia: a review of 176 cases during 1980–1992Scand. J. Infect. Dis. 1994 26:361-67. [Google Scholar]
[4]. Grahnquist L, Lundberg B, Tullus K, Neonatal Proteus meningoencephalitis; Case reportActa Pathol. Microbiol. Immunol. Scand 1992 100:734-36. [Google Scholar]
[5]. Burke J. P., Ingall D., Klein J. O., Gezon H. M., Finland M, Proteus mirabilis infections in a hospital nursery traced to a human carrierN. Engl. J. Med. 1971 284:115-21. [Google Scholar]
[6]. Ceccareili M., Balestri M, Fontani C, Lupetti L, Ughi C, Recurrent meningitis: a case reportEur J Pediatr 1989 148:646-47. [Google Scholar]
[7]. Unhanand M, Mustafa MM, McCracken GH Jr, Nelson JD, Gram negative enteric bacillary meningitis; a 21 year experienceJ Pediatr 1993 122:15-21. [Google Scholar]
[8]. Chang Chien HY, Chiu NC, Li WC, Huang FY, Characteristics of neonatal meningitis in a teaching hospital in Taiwan from 1984-1997J Microbiol Immunol Infect. 2000 33:100-04. [Google Scholar]
[9]. Ersahin Y, Murluer S, Guzelbag E, Brain abscess in infants and childrenChilds Nerv Syst. 1994 10:185-89. [Google Scholar]
[10]. Smith ML, Mellor D, Proteus mirabilis meningitis and cerebral abscess in the newborn periodArch Dis Child 1980 55:308-10. [Google Scholar]
[11]. Mulder CJ, Zanen HC, A study of 280 cases of neonatal meningitis in the NetherlandsJ Infect 1984 9:177-84. [Google Scholar]
[12]. Franco SM, Cornelius VE, Andrews BF, Long-term outcome of neonatal meningitisAm J Dis Child 1992 146:567-71. [Google Scholar]
[13]. Yurdakok M, Antibiotic use in neonatal sepsisTurk J Pediatr 1998 40:17-33. [Google Scholar]
[14]. Lardhi Amer A, Neonatal group A streptococcal meningitis: a case report and review of literatureCases Journal 2008 1:108 [Google Scholar]