Organophosphate insecticides are the potent inhibitors of the acetylcholinesterase enzyme which lead to an increased acetylcholine activity, which are responsible for symptoms such as abdominal pain, diarrhoea, vomiting and hypersalivation. We are reporting on a young male with acute organophosphate poisoning, who presented with unusual complications like toxic pancreatitis with an intraabdominal abscess.
INTRODUCTION
Organophosphorous poisoning is a major clinical problem in the developing countries like India. Neurologic, cardiac and respiratory complications are the main causes of the morbidity and the mortality in these patients. The involvement of other systems can also occur, but it is very uncommon.
In the recent years, a number of case reports of acute pancreatitis which were associated with acute organophosphorous poisoning had been described [1–6]. The cause and the effect relationship of this disease entity have been demonstrated in animal studies. However, this association may still have not been widely recognized.
Acute pancreatitis usually follows a subclinical course and it therefore remains unrecognized and leads to increased morbidity and mortality in the patients who are affected by it.
CASE REPORT
A 25 year male patient presented to the emergency department with a history of the ingestion of a pesticide 5 hours ago. At the time of presentation, the patient had abdominal pain, vomiting, nausea and copious oral secretions. The patient denied having any history of alcohol consumption or alcohol abuse. His past history was unremarkable.
On physical examination, the patient was drowsy, heart rate was 88/min, regular and blood pressure was 100/60 mmHg and his respiratory rate was 26/min. The patient was hypoxic, with an SPO2 level of 80-85%. His chest examination showed bilateral, diffuse, coarse crepitations. Bilateral pinpoint pupils and diffuse fasciculations were found on his nervous system examination. His other system examinations were unremarkable. Based on the clinical picture, a provisional diagnosis of organophosphorous poisoning was made.
The treatment was initiated with gastric lavage. A bolus dose of 8 mg atropine and 1.5 gms PAM was given. The atropine infusion was continued with 4 mg /hr and it was titrated to maintain the pulse rate between 100-140 beats per minute. Bolus doses of 1.5 gms of PAM were also continued every 8th hourly for 3 days.
At the time of his admission, his serum pseudocholinesterase was 412U/L (5000-13000 U/L) and his total count showed mild leucocytosis . His routine blood examination, liver function tests, renal function tests, ECG and chest radiography were within normal limits. The subsequent laboratory changes are shown in [Table/Fig-1].
Laboratory values at admission and follow up
| Investigations | 1st week | 2ndweek | 3rd week | 4th week |
|---|
| PH | 7.41 | 7.44 | 7.38 | |
| PaO2 | 72 | 82 | 76 | |
| PaCO2 | 39 | 40 | 37 | |
| HCO3 | 24.2 | 23.1 | 22.4 | |
| Hb% | 10.6 | 10 | 8.8 | 11.2 |
| Total count | 24,200 | 15,000 | 16000 | 15,000 |
| Differential count N/L/M/B | 73/06/01/ | 85/15/4 | 95/15/4 | 64/22/5 |
| RBS (mg/dl) | 120 | 140 | 124 | 118 |
| Blood urea (mg/dl) | 24 | 26 | 20 | 30 |
| Serum creatinine (mg/dl) | 0.8 | 0.8 | 1.0 | 0.9 |
| ALT (U) | 35 | 29 | 18 | 24 |
| AST (U) | 68 | 25 | 41 | 32 |
| ALP (U) | 216 | 177 | 283 | 155 |
| Albumin (mg/dl) | 0.6 | 1.8 | 2.0 | 2.3 |
| LDH (U/L) | - | 254 | - | - |
| Serum amylase (IU/L) | 2879 | 153 | 147 | - |
| Ascitic fluid amylase (IU/L) | 46 780 | - | - | - |
| Serum lipase (U/L) | 114 | - | - | - |
| Serum calcium (mg/dl) | 6 | 7 | 8.2 | 8.0 |
| Serum pseudoch olinesterase (5000-13000 U/L) | 412 | 497 | 502 | 850 |
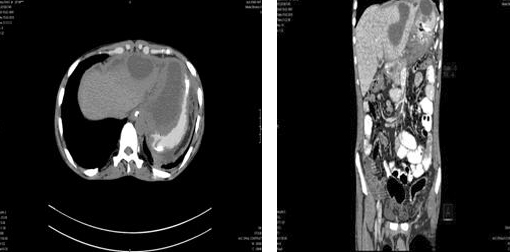
The patient responded to the initial treatment. His oral secretions and bronchial secretions decreased but the patient was still hypoxic. The saturation was maintained with O2 administration, but on 3rd day, it deteriorated further, with poor respiratory efforts and he developed type I respiratory failure and worsening of the abdominal pain, with a localized swelling. Therefore, the patient was put on ventilatory support. Due to the persistent abdominal pain and the appearance of the localized swelling, an ultrasound (USG) of the abdomen was done, which revealed a biloculated collection of pus in the subcapsular region (the left lobe of the liver), an oedematous pancreas which involved the body and the tail and ascites. An ultrasound guided drainage of the liver abscess was attempted, but no pus was aspirated. The findings of the ultrasound were later confirmed by CT of the abdomen [Table/Fig-2a & b]. The patient was kept nil per orally. Amikacin, metronidazole, 3rd generation cephalosporins and octreotide were started.
CT scan showing left subcapsular abscess extending into the lesser sac (A & B)
The abdominal pain and the localized swelling gradually increased in intensity and size respectively, over the next 5 days.
On day 8, an ultrasound guided drainage of the abscess was done and the collected sample was sent for culture and antibiotic sensitivity tests, which showed the growth of Klebsiella species which were sensitive to Imipenem [Table/Fig-3]. Subsequently, the ceftriaxone was substituted with imipenem.
| Culture and sensitivity | Blood | Urine | Subphrenic abscess fluid | E T Secretion |
|---|
| First | Negative | Enterococcus spp sensitive to Imipenem, Amoxyclav | Klebsiella spp sensitive to Imipenem | Staph. aureus sensitive to Netilmycin, Tazobactum. Follow up culture-Klebsiella sensitive to Imipenem, Gentamycin and Netilmycin |
| Second | Negative | Negative | - | Negative |
| Third | Negative | Negative | - | Negative |
The patient started improving symptomatically over the next few days and a repeat USG which was done, showed disappearance of the liver abcess and resolution of the pancreatic abscess. The patient was discharged after one month of the hospital stay. At one month of follow up, the patient was found to be absolutely normal and he was able to take up his routine activities.
DISCUSSION
Acute pancreatitis (toxic pancreatitis) is a rare complication of organophosphorus poisoning. It generally shows a subclinical course [1]. It is mainly caused by acetylcholine release from the pancreatic nerves and the prolonged hyper stimulation of the acinar cells [2]. Some patients may also develop serious complications like abscess formations [2,3,6].
In 1979, Dressel had described the first case report of acute pancreatitis with organophosphrous poisoning [7]. The patient was a healthy young woman who was brought in a comatosed state. At admission, the serum amylase was found to be 20 times elevated, which had returned to normal by the 4th day. In our patient, acute pancreatitis was suspected on the third day of his admission, with his serum amylase being 20 times elevated and his ascitic fluid amylase also being very high ( 46,780 U), which returned to normal in the second week of his admission [8]. In 1981, Moore and James had described another case of acute pancreatitis which had presented to the hospital in a comatosed state, with signs of organophosphorous poisoning [9]. It was later confirmed by the low pseudocholinesterase levels.
In 1981, Dagli had reported a case of diazinon poisioning who had developed acute pancreatits. Following this, Dagli and Sheikh studied 75 cases who had been admitted to a general hospital with a definitive history of malathion ingestion [10,11]. Hyperamylasaemia was found in 47 cases (63%) and in 10 cases (21%), the levels were more than twice the upper limit of the normal levels. The higher level was more than four times the upper limit of the normal level. In 42 cases (89%), the levels had returned to normal within 48 hours of the admission of the patients.
Isoenzyme studies or pancreatitic biopsies were not done in these cases and therefore, it was not clear whether the hyperamylasaemia which was observed was due to pancreatitis. However, experiments which were done on dogs showed quite convincingly that pancreatitis could be produced by the intra venous infusion of secretin and diazinon. Significant increases of serum amylase and lipase were found at 1, 2 and 3 hours.
In our patient, acute pancreatitis was diagnosed, based on the laboratory and the ultrasound abdomen findings on the 3rd day of his admission to the hospital. The other possible aetiological factors for acute pancreatitis like alcohol, biliary disease and medications were excluded. A repeat ultrasound of the abdomen and CT of the abdomen showed regression of the oedema in the pancreas and the size of the abscess cavity, with the subsequent follow up showing disappearance of the abscess cavity.
Liver involvement in the organophosphorus poisoning is very rare. A post-mortem study of the deaths which had been caused by organophosphorus poisoning had shown the involvement of the liver in only 14 % of the cases [5]. It had mainly revealed microscopic findings as fatty changes in 4(36.36%) patients; congestion in 5(45.45%) patients; alcoholic hepatitis in 1 patient and sinusoidal dilatation in 1(9.09%) patient. In our patient, the liver abscess had developed secondary to the acute pancreatitis.
Hence, in the patients with organophosphorous poisoning, who complain of persistent abdominal pain, not only acute pancreatitis, but also complications like liver abscesses should also be searched for, so that an early diagnosis can be made, to prevent further complications.
CONCLUSION
The diagnosis of acute pancreatitis may be masked by the systemic effects of the OP poisoning like abdominal pain, nausea and vomiting, which are also the common features of acute pancreatitis. Hence, one should consider the possibility of acute pancreatitis in the patients of organophosphorous poisoning, who have persistent abdominal pain. In such patients, an early diagnosis which is made on the basis of ultrasound and CT scan will help in preventing the morbidity and the mortality.
[1]. Kandalaft K, Liu S, Manivel C, Organophosphate increases the sensitivity of the human exocrine pancreas to acetylcholinePancreas 1991 6:398-403. [Google Scholar]
[2]. Krupesh N, Chandrashekar TR, Organophosphorus poisoning - still a challenging propositionIndian J. Anaesth 2002 46(1):40-43. [Google Scholar]
[3]. Kumar SV, Fareedullah MD, Sudhakar Y, A current review on organophosphorus poisoningArchives of Applied Science Research 2010 2(4):199-215. [Google Scholar]
[4]. Dresse TD, Goodale RL, Pancreatitis as a complication of anticholinesterase insecticide intoxicationAnn Surg. 1979 189(2):199-204. [Google Scholar]
[5]. Sutay SS, Tirpude BH, The pattern of the histopathological changes in liver poisoningJ Indian Acad Forensic Med. 2008 30(2):63-68. [Google Scholar]
[6]. Sahin IC, The prevalence of pancreatitis in organophosphorous poisoningHum Exp Toxocol. April 2002 21(4):175-77. [Google Scholar]
[7]. Dressel TD, Goodale RL Zweber, Borner JW, The effect of atropine and duct decompression on the evolution of diazinon: Induced acute canine pancreatitisAnn Surg. 1982 195:424-34. [Google Scholar]
[8]. Singh. S, Hyperamylasemia and acute pancreatitis following anticholinesterase poisoningHuman and Experimental Toxicology 2007 26:467-71. [Google Scholar]
[9]. Moore PG, James OF, Is acute pancreatitis induced by organophospate poisoning?Postgrad Med J. 1981 57:660-62. [Google Scholar]
[10]. Dagli AJ, Moos JS, Shaik WA, Acute pancreatitis as a complication of diazion poisoningL Assoc Phy Ind 1981 29:794 [Google Scholar]
[11]. Dagli AJ, Shaik WA, Pancreatic involvement in Malthion. Anticholinesterase insecticide intoxicationA study of 75 cases Br J Clin Prac. 1983 :270-72. [Google Scholar]