Tuberculosis is a disease with protean manifestations. We present a case which was initially suspected as bronchogenic carcinoma with lymphangitic carcinomatosis, based on radiological appearance but later diagnosed as pulmonary tuberculoma with military tuberculosis and silicosis after thoracotomy and open lung biopsy. The patient was treated successfully with Antituberculosis Therapy (ATT). Rarity of presentation in form of pulmonary tuberculoma co-existing with histological features of miliary tuberculosis and silicosis, led us to report this case.
INTRODUCTION
A pulmonary tuberculoma is a well circumscribed nodule or mass in the lungs, caused by Mycobacterium tuberculosis. It is encapsulated by multiple concentric layers of connective tissue.
Miliary tuberculosis is the result of diffuse dissemination of tubercle bacilli via blood stream, causing numerous foci in multiple organs.
Silicosis is an occupational lung disease which is caused by the inhalation of crystalline silica dust, and it is marked by inflammation and scarring in form of nodular lesions in the lungs.
Pulmonary tuberculosis coexists in 25% patients of acute or chronic silicosis, and as compared to normal population, silicosis patients have 2.8 times higher relative risk of tuberculosis. Pulmonary tuberculoma coexisting with military tuberculosis and silicosis has never been reported till now, to the best of our knowledge. We did an extensive search of the PUBMED indexing system and the internet, but came across no instance of a pulmonary tuberculoma which co-existed with miliary tuberculosis in a silicosis patient. That is why we are reporting this case.
Diagnosis was obtained after thoracotomy and open lung biopsy. A histopathological examination of the excised tissue revealed the coexistence of these 2 pathologies. Our case report highlights the need to opt for invasive investigations when faced with multiple radiological differential diagnoses.
CASE REPORT
A 48 years old male, stone cutter-engraver was admitted with the chief complaint of a progressively increasing breathlessness which was there since 1 year , of grade IV MMRC which was there since 3 days, of a right sided chest pain which was there since 3 months and of high grade fever which was there for the past 1 week. The pain was dull aching and non radiating in nature and it was localized to the right chest, below the clavicle. There was no history of any trauma or a prior procedure. There was no significant history of any past illness .The patient was an ex-smoker, having smoked around half a bundle of bidis for 30 years, till a year back. He had started out with the stone cutting-engraving profession in adolescence and since then, was continuously exposed to stone dust during his workday.
He had BP 128/70, pulse rate 96/minute, respiratory rate 32/minute and O2 saturation 86% at room air. The patient had a toxic appearance. Respiratory system examination revealed an impaired percussion note and reduced air entry on infraclavicular region and fine pan inspiratory crepitations bilaterally. The patient was non diabetic and immunocomptetant.
We started the patient on a supportive management – low flow inhaled oxygen to maintain the O2 saturation above 92% and antibiotics. His forearm showed an induration of 18 mm with PPD after 72 hours. His sputum smear was negative for AFB.
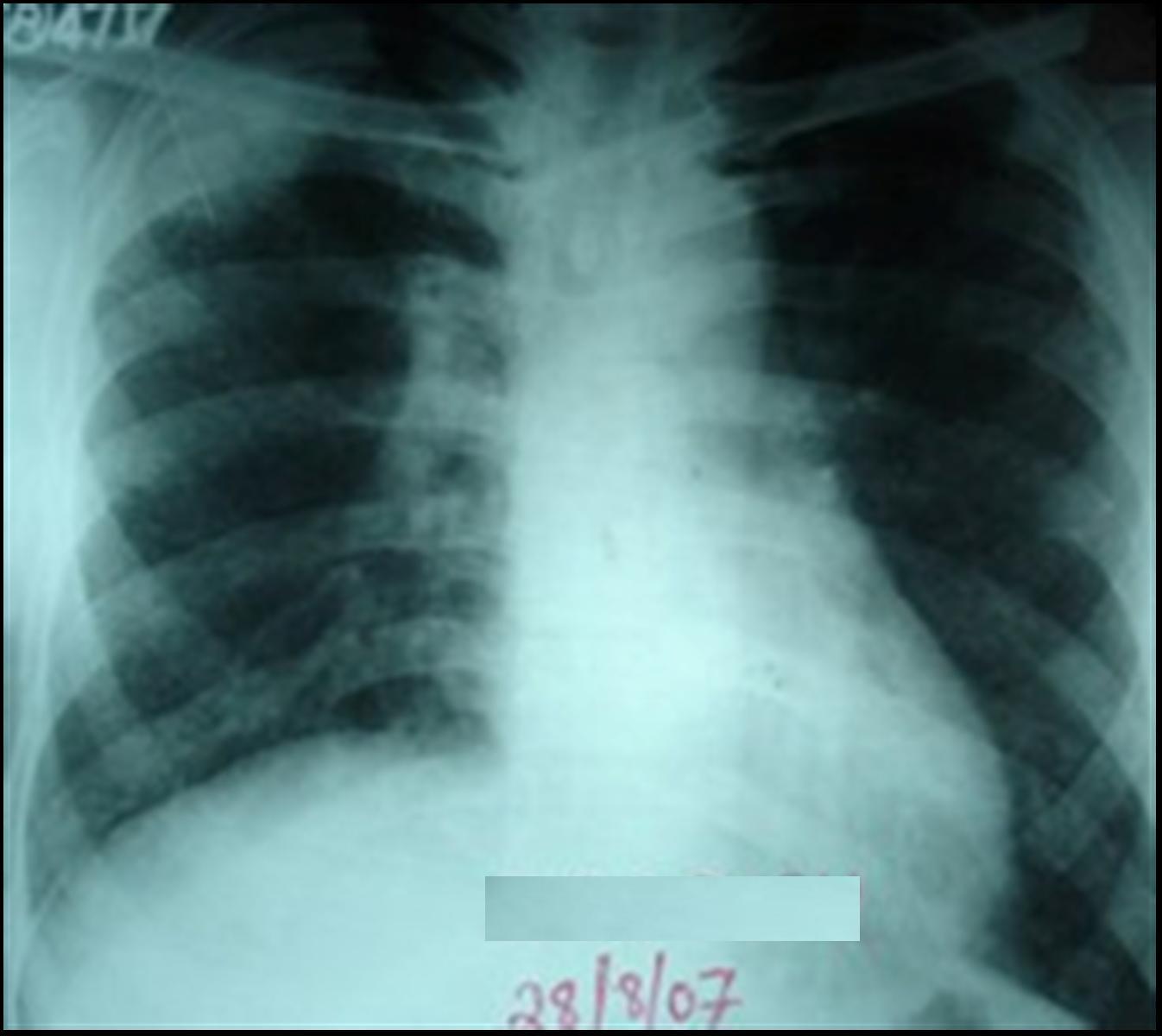
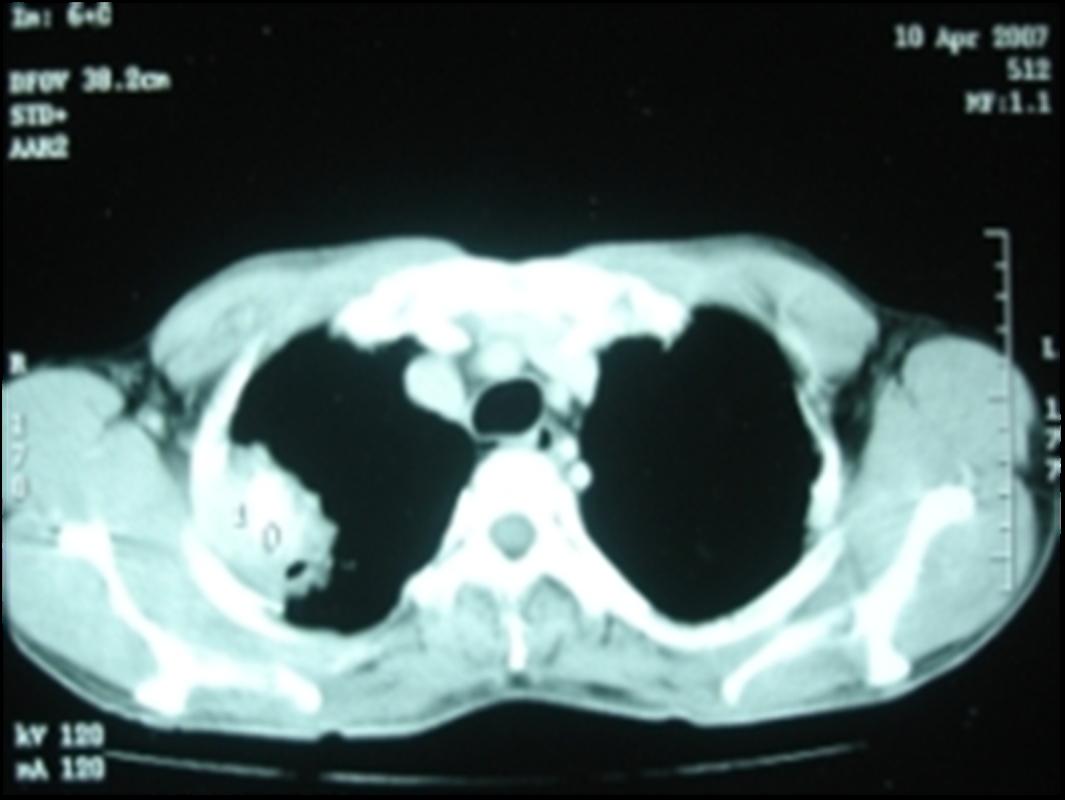
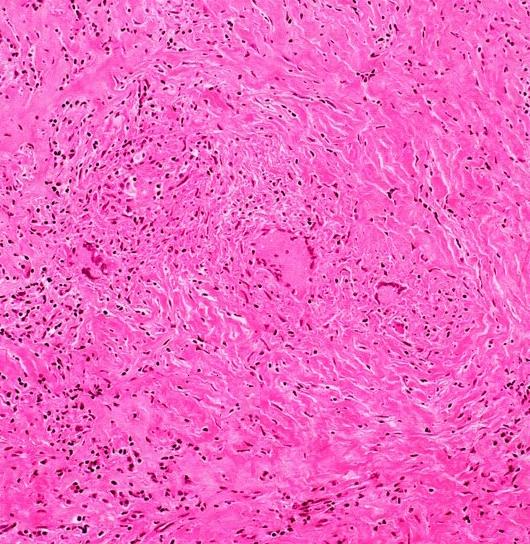
We did a CECT of the thorax, which showed a right sided intrathoracic mass with an evidence of calcifications in the apical and the posterior segments of the right upper lobe [Table/Fig-1] and a micro nodular appearance in the bilateral lung fields on chest X-ray, PA [Table/Fig-2]. CT guided FNAC and biopsy of the intrathoracic mass was done twice but revealed fibrocollagenous tissue. The patient then underwent a thoracotomy and an open lung biopsy. At thoracotomy, numerous miliary nodules were seen on the pleural surface. The biopsy from accessible area of lung revealed caseous necrosis with epitheloid cells, Langerhan’s giant cells and pneumonitis, separated by dense fibroblastic tissue. The necrotic areas consisted of dense hyalinized connective tissue and deposits of small crystalline material. Based on his histological and radiological presentations, we diagnosed it as a case of pulmonary tuberculoma with miliary tuberculosis and silicosis.
Chest X ray PA showing right upper zone mass lesion
CECT thorax at presentation, showing mass with calcifications and cavity
We started the patient on four drug ATTs which comprised of rifampicin, isoniazid, ethambutol and pyrazinamide. The patient gradually became afebrile, his breathlessness reduced after one month and his oxygen saturation improved on room air.
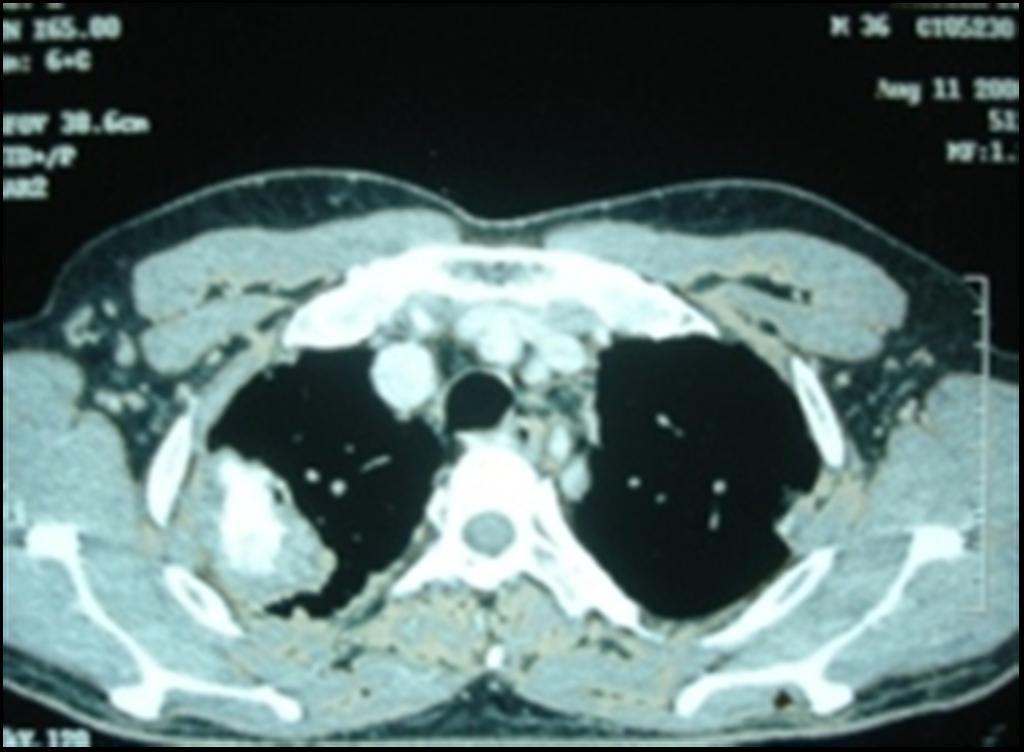
A CT thorax [Table/Fig-3] was done after 5 months, which revealed that the previous mass had calcified and reduced in size, persistence of the miliary nodules and calcification of the pretracheal and the paratracheal lymph nodes, with a bilateral pleural thickening. We again performed a CT guided FNAC and a biopsy of the mass, which revealed only necrosis [Table/Fig-4]. The patient did not consent for a repeat thoracotomy. At present, the patient is on follow up after completing nine months of ATT. He is healthy and he has only bearable chest pain.
CECT thorax repeated after ATT, showing evidence of healing
DISCUSSION
Pulmonary tuberculoma and miliary tuberculosis are rare, even in immunocompetent adults. Pulmonary tuberculomas develops in 6–9% of the post-primary TB patients. Tuberculomas are usually found as single nodules and they may include a cavity or a calcification with sharp margins. They are usually found in the upper lobes [2].
Miliary tuberculosis is found in 1.3% of all the pulmonary tuberculosis cases [3]. Approximately two-thirds of all the miliary TB cases are Acid-Fast Bacilli (AFB) smear-negative, and even a transbronchial biopsy frequently fails to reveal the AFB or the caseating granulomas [4–6]. In a study, 32% were positive (≥ 10 mm of induration) to 5TU of PPD [6].
The other option for the rapid diagnosis of miliary TB includes invasive procedures such as an open lung biopsy or an empirical ATT which is based on radiology. A random distribution of micronodules are most commonly seen in the metastatic disease, in silicosis and in miliary tuberculosis [7]. The predisposing factors for the development of miliary tuberculosis include advanced age, the Human Immunodeficiency Virus (HIV) infection, malnutrition, diabetes mellitus, chronic renal failure, organ transplantation, corticosteroid therapy, silicosis, immunosuppressive therapy, and pregnancy [8].
India has 3 million workers who are exposed to silicosis every year and it was the predisposing factor to tuberculosis in our patient [9].
Free crystalline silica, SiO2, is the most common mineral in the earth’s crust. It is found in sand and in rocks such as granite, sandstone, flint and slate, and in some coal and metallic ores. In the respiratory tract, the silica particles are quickly ingested by the macrophages into phagosomes, which then interact with the lysosomes and release proteolytic enzymes, cytokines (mostly IL-1, IGF-1,PDGF and TNF-alpha) and oxygen radicals. This massive release of lysosomal contents results in the death of the cells and inflammation in the form of lymphocyte and granulocyte recruitment and T-helper cell proliferation. Local fibrosis occurs with the elaboration of collagen and fibrinonectin and collagen fibres are continually laid down in a concentric fashion to form the characteristic lesion of the silicosis, the well circumscribed silicotic nodule in the later stages [8]. The later stages of the silicosis may involve infection with Mycobacterium tuberculosis, atypical mycobacteria, fungi and Acinetobacter spp. , thus complicating the diagnosis and management and accelerating the fibrotic process [10].
Our patient had a tuberculoma with a cavity, which was diagnosed on radiology, but after taking an ATT for 9 months, it calcified and shrunk in size, with the cavity still persisting.
A possible radiological differential diagnosis could be multiple silicotic nodules with coalescing of the nodules in the upper zone to mimic a ‘mass’. But in contrast to such a possibility, our patient clinically and radiologically improved with the ATT. We also advised the patient to change his occupation.
This case highlights the need of keeping judicious balance between invasive investigations and starting empiric treatment, when faced with “synchronous double pathology” and diagnosing in retrospect.
[1]. Cowie RL, The epidemiology of tuberculosis in gold miners with silicosisAm J Respir Crit Care Med. 1994 150:1460-62. [Google Scholar]
[2]. Lee HS, Oh JY, Lee JH, Yoo CG, Lee CT, Kim YW, Response of pulmonary tuberculomas to anti-tuberculous treatmentEur Respir J. 2004 23:452-55. [Google Scholar]
[3]. Hussey G, Chisholm T, Kibel M, Miliary tuberculosis in children: a review of 94 casesPediatr Infect Dis J. 1991 10:832-36. [Google Scholar]
[4]. Maartens G, Willcox PA, Benatar SR, Miliary tuberculosis: rapid diagnosis, hematologic abnormalities and outcome in 109 treated adultsAm J Med. 1990 89:291-96. [Google Scholar]
[5]. Al-Jahdali H, Al-Zahrani K, Amene P, Memish Z, Al-Shimemeri A, Moamary M, Alduhaim A, Clinical aspects of miliary tuberculosis in Saudi adultsInt J Tuberc Lung Dis. 2000 4:252-55. [Google Scholar]
[6]. Mert A, Bilir M, Tabak F, Ozaras R, Ozturk R, Senturk H, Miliary tuberculosis: clinical manifestations, diagnosis and outcome in 38 adultsRespirology 2001 6:217-24. [Google Scholar]
[7]. McGuinness G, Naidich DP, Jagirdar J, Leitman B, McCauley DI, High resolution CT findings in miliary lung diseaseJ Comput Assist Tomogr 1992 16:384-90. [Google Scholar]
[8]. Mossman BT, Churg A, Mechanisms in the pathogenesis of asbestosis and silicosisAm J Respir Crit Care Med 1998 157:1666-80. [Google Scholar]
[9]. Cowie RL, Silicotuberculosis: Long-term outcome after short-course chemotherapyTubercle and Lung Disease 1995 76:39-42. [Google Scholar]
[10]. Rees D, Murray J, Silica, silicosis and tuberculosisInt J Tuberc Lung Dis. 2007 11:474-84. [Google Scholar]