Cervical cancer, one of the most dreaded form of genital cancers in females, tends to originate in the uterine cervix (transformational zone). Ironically, it is one of the most frequently and easily screened organ system of the female genital tract, yet contributing to a major chunk of cancers amongst females.
A lack of basic understanding of the importance of the routine screening has been a major contributor to the high incidence of cancer of the cervix amongst the female population in the developing nations.
In India, over the past 5 decades, there has been a definitive change or shift in the trend of the cancer development amongst females, thus making cervical cancers slip down to the second position, being second only to breast cancer.
Nevertheless, the nuisance which is posed by cervical malignancies is much more than ever. The year 2005 had a total global estimate which was put to 520,000 cases of cervical cancer, of which little more than 100,000 belonged to the developed nations and the rest which were found had their origins in the developing world [1].
The projected rise of the cervical cancer cases in India in the last decade, 2000- 2010, has been alarming, from 0.11 million cases to 0.16 million cases.1 Over 80% of the cervical cancers present at a fairly advanced stage and around 80,000 deaths have been reported to be caused by cervical cancer in India [1,2]. The Human Papilloma Virus (HPV) infection has been at the forefront in the development of cancer of the cervix all over the globe.
The predominant subtypes which cause cervical malignancies include HPV 16 or 18, though other strains have been implicated. Besides HPV as an obvious infective risk factor, the associated factors which propagate cervical malignancies include, age, multiparity, sexual partners, an early age of marriage, oral contraceptives, tobacco and immunosupression [3].
The field of cytopathology,off late, has seen advancements, with various types of special staining techniques,cell proliferation markers, morphometric analyses and flow cytometric analyses. amongst the simple, inexpensive cell proliferative methods, one such technique is silver staining of the nucleolar organizer regions of the nucleus – once stained, these regions behave as cell proliferation markers, enormously aiding in giving the indications of the cell ploidy and the proliferation status.
However, despite various visual tests coming up,it seems that the PAP smear still remains a gold standard for cervical screening. This study has emphasized on the visualization of AgNORs on microscopy with the aid of a special silver staining technique.
The method which was used in the present study was based on the viewing of the nucleoli in the nucleus of a cell by using silver stains i.e. AgNOR, thereby assessing the measure of the cell proliferation on the basis of the nucleolar counts. It is known as the one step, simplified, Silver Nitrate Staining(AgNOR) technique and it has been widely employed, both in the cytological and the histopathological studies of various organs. However, there is a relative scarcity of the application of the AgNOR technique in cytopathology, especially in cervical smears.
MATERIALS AND METHODS
The present study was carried out at Jawaharlal Nehru Medical College (JNMC), Sawangi (Meghe), Wardha India, a rural hospital, with the intention of testing a hypothesis with respect to the applicability of the AgNOR technique in cervical pathological smears, thereby utilizing the AgNOR score, for it to act as an adjunct with the cervical PAP stained smears for the evaluation of the cervical cytopathological diagnosis.
This was a prospective study which was applied on the patients who attended the gynaecological OPD and ward at JNMC, Wardha. The study was carried out in a span of 2 years. An ethical clearance from the institution and an informed consent from the study subjects were duly obtained.
INCLUSION CRITERIA
All the women who were above 60 years of age, irrespective of their parities.
All the women who were above 35 years of age, who had three or more children.
All the women who revealed pathological lesions on the cervix during the clinical examination, which included malignancy.
All the patients who presented with gynaecological symptoms.
The relevant clinical data and the history regarding the age, parity, marital status and multiple sexual partners and a detailed menstrual history were obtained from the patients. The presenting symptoms, the history of contraception and the clinical findings were recorded on the cytology form which was specially designed for this purpose.
Two cervical smears from the squamocolumnar junction were carefully collected from the clinically significant, high risk women. One smear was PAP stained and evaluated, when it was diagnosed with a significant cervical lesion under the following mentioned categories i.e. normal, chronic cervicitis, a low squamous intra epithelial lesion, a high squamous intra epithelial lesion, carcinoma cervix only then the other smear collected from the same patients was subsequently stained with silver nitrate one step staining technique for AgNOR counts.
This particular study comprised of a total of 50 cases [Table/Fig-1].
Lesion Wise Distribution Of 50 Cases
| Sr. No. | Cytopathological Diagnosis | Total no. of cases |
|---|
| 1 | Normal Cervix | 10 |
| 2 | Chronic Cervicitis | 15 |
| 3 | Low squamous Intraepithelial Lesion | 15 |
| 4 | High squamous Intraepithelial Lesion | 06 |
| 5 | Carcinoma Cervix | 04 |
| Total | 50 |
THE MATERIALS WHICH WERE USED FOR THE SILVER COLLOID STAINING
The smears were stained by the simple one step silver colloid technique which was devised by Crocker [4].
EVALUATION OF THE SMEARS
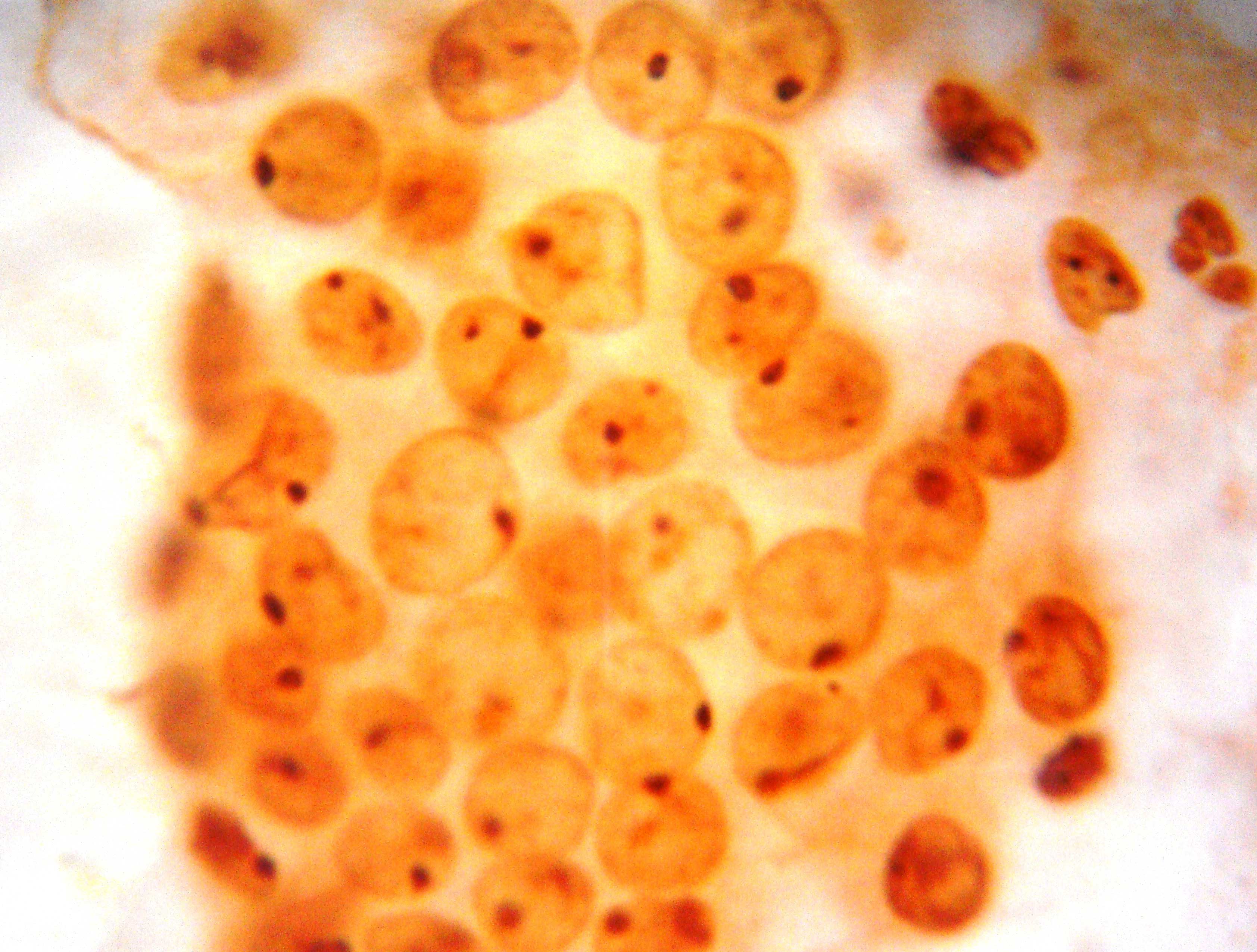
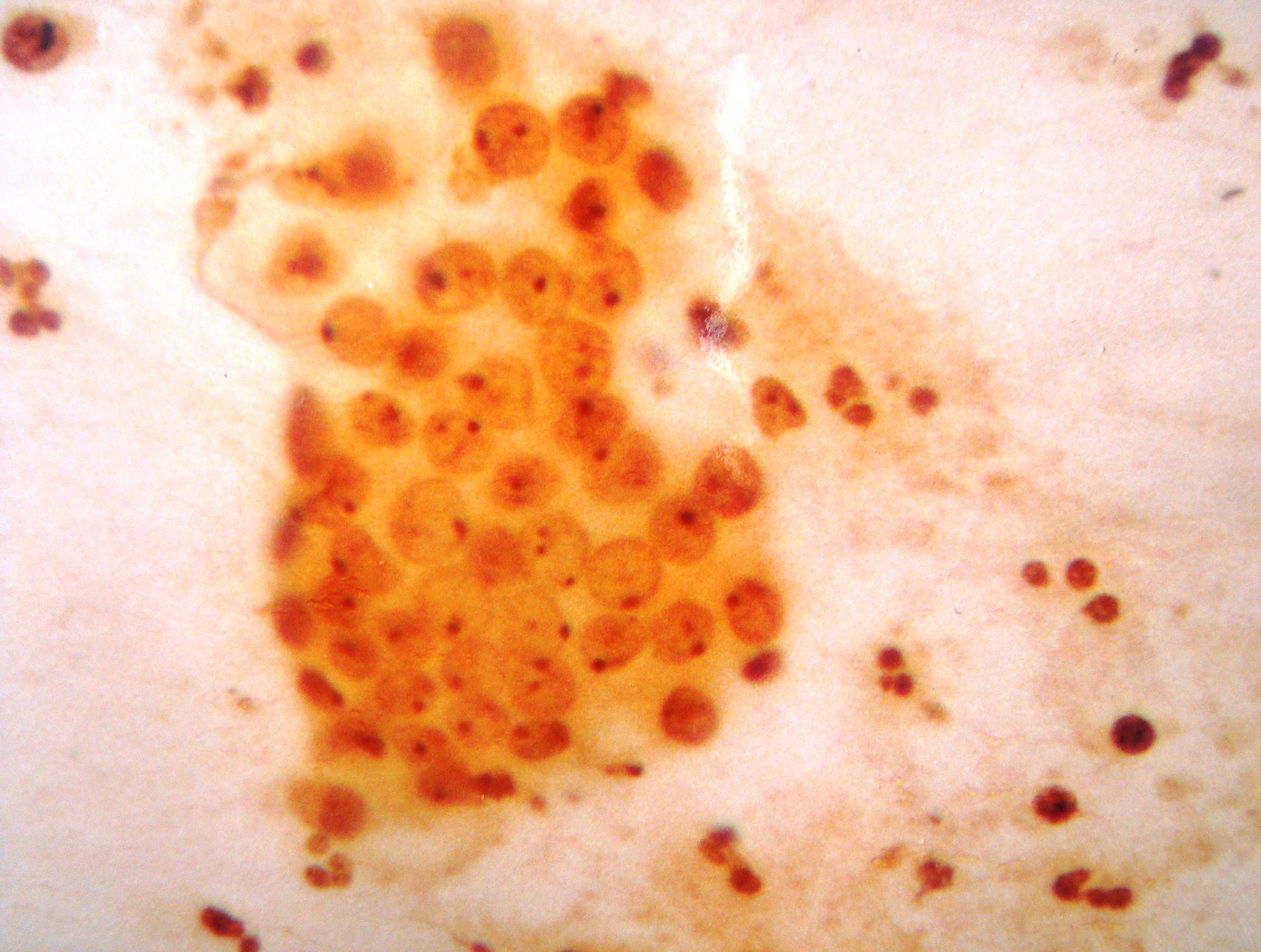
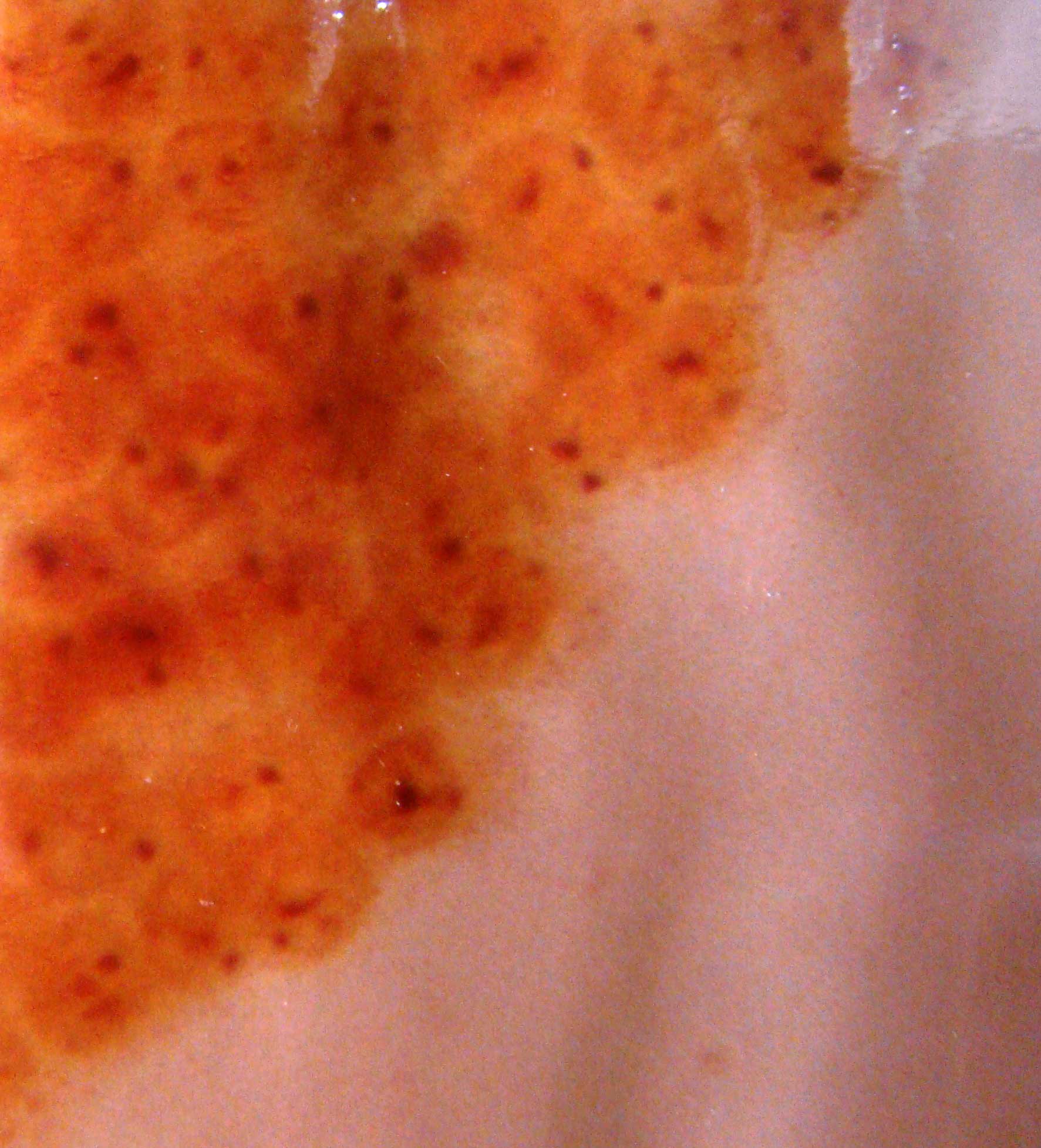
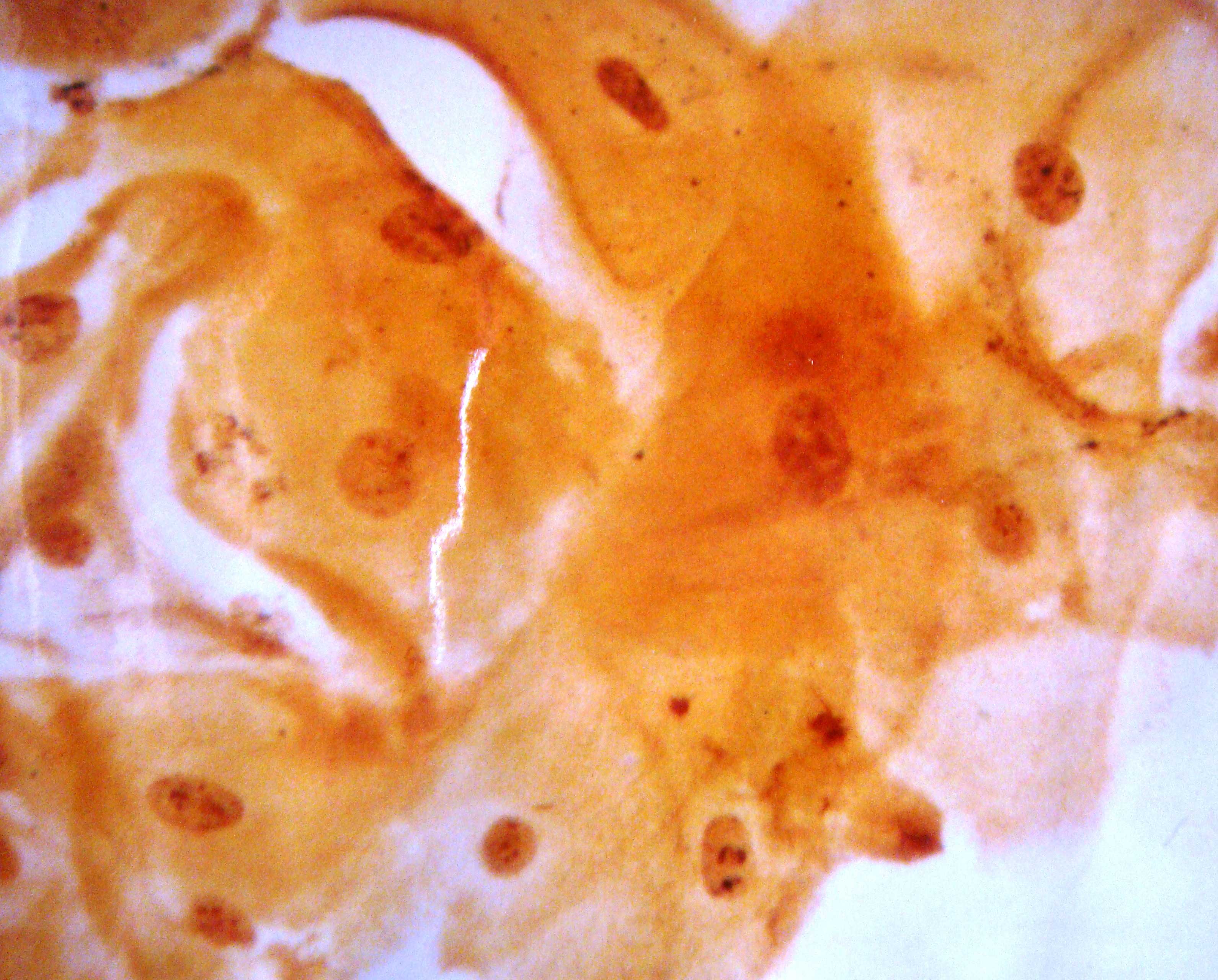
The AgNOR sites appear as intranuclear black dots and the background appears pale yellow. The controls which were used were normal superficial squamous epithelial cells of the cervix, that on an average, had 1 AgNOR per cell nucleus. It was observed that the AgNOR dots were single larger and compact in the normal cervix and in chronic cervicitis. They appeared small and loosely arranged in the dysplastic and malignant lesions of the cervix.
THE METHOD FOR COUNTING THE AGNORS
For the AgNOR counts:
A slide was considered as a single unit in which 100 nuclei were counted for the presence of black appearing AgNORs by using an oil immersion lens.
The AgNOR dots from each nuclei (a total of 100 nuclei) were then summed up and the mean AgNOR count for each slide was then calculated4
The AgNOR scores were then compared with the corresponding slide of the same patient, which was stained with PAP smears. The evaluation of the AgNOR counts with the corresponding cytopathological diagnosis (on the PAP smears) was then done.
The cytopathological diagnosis on the PAP smear was used as an adjunct for the correct evaluation of the significant AgNOR values.
The AgNOR counts were divided and distributed within five categories, based on the cytopathological PAP stained diagnosis (as per the Bethesda system) [Table/Fig-2 & 3].
Table showing Lesion based AgNOR counts.
| Sr. No. | Normal Cervix | Chronic Cervicitis | LSIL | HSIL | Carcinoma Cervix |
|---|
| 1 | 1.80 | 2.08 | 2.54 | 3.90 | 6.24 |
| 2 | 2.30 | 2.20 | 2.66 | 4.50 | 6.09 |
| 3 | 2.00 | 1.90 | 3.00 | 3.80 | 5.55 |
| 4 | 1.50 | 2.26 | 2.76 | 4.10 | 6.04 |
| 5 | 1.80 | 2.05 | 3.30 | 4.94 | |
| 6 | 1.52 | 2.20 | 1.84 | 3.90 | |
| 7 | 1.32 | 2.05 | 2.15 | | |
| 8 | 1.92 | 2.22 | 3.16 | | |
| 9 | 2.00 | 2.03 | 3.24 | | |
| 10 | 1.40 | 1.96 | 3.05 | | |
| 11 | | 2.04 | 2.96 | | |
| 12 | | 2.40 | 2.75 | | |
| 13 | | 2.01 | 3.00 | | |
| 14 | | 1.90 | 2.70 | | |
| 15 | | 2.10 | 3.16 | | |
AgNOR counts/cells in various categories of cytopathological diagnosis
| Cytopathological Diagnosis | Mean | SD | 95 % Confidence Interval Meanα2SE |
|---|
| Normal Cervix (Fig 8) | 1.75 | 0.31 | 1.75α0.19 |
| Chronic Cervicitis (Fig 9) | 2.09 | 0.13 | 2.09α0.07 |
| LSIL (Fig 10) | 2.81 | 0.40 | 2.81α0.20 |
| HSIL (Fig 11) | 4.17 | 0.45 | 4.17α0.37 |
| Carcinoma Cervix (Fig 12) | 5.98 | 0.29 | 5.98α0.29 |
THE STATISTICAL METHODOLOGY
The Student’s unpaired ‘t’ test was applied in this technique to evaluate the significance of the AgNOR scores.
With ‘t’ test comparisons between AgNOR counts of
Normal Cervix with Chronic Cervicitis, LSIL, HSIL and Carcinoma Cervix.
Chronic cervicitis with Normal Cervix, LSIL,HSIL and Carcinoma Cervix.
LSIL with Normal Cervix, Chronic Cervicitis, HSIL and Carcinoma Cervix.
HSIL with Normal Cervix, Chronic Cervicitis, LSIL, and Carcinoma Cervix.
Carcinoma Cervix with Normal Cervix, Chronic Cervicitis, LSIL and HSIL.
OBSERVATIONS
This study comprised of a total of 50 cases.
The total number of cases against the cytopathological diagnoses were as follows.
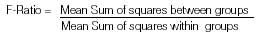
Inference: The ‘between the group’ variability was greater than the ‘within the group’ variability. From the F-test, we found that the difference between these 2 variations was significant (F=167.83,p<0.05) [Table/Fig-4]. There was a significant variation in all the 5 groups. There was an evidence to show that all the five groups were not from populations which had identical means.
| Source of Variation | Sum of Squares | Degrees of Freedom | Mean Sum of Squares | F-Ratio |
|---|
| Between Groups | 70.43 | 4 | 17.609 | 167.83 p<0.05 Significant |
| Within Groups | 4.72 | 45 | 0.105 |
| Total | 75.15 | 49 | |
Note: * = Significant at 5% level of significance
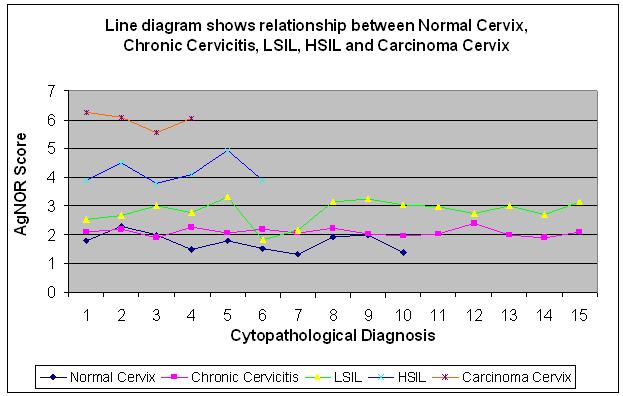
[Table/Fig-5] shows that all the 5 comparisons which were made with the use of the ‘t’ test, came out to be significant, that is the above derived values were equal to or greater than the tabulated values.
Inter comparative chart of various categories bases on Student’s unpaired t-test.
| Variables | N | CC | LSIL | HSIL | Ca Cx |
|---|
| N | - | 3.78* | 12.93* | 13.12* | 23.11* |
| CC | 3.78* | - | 6.5* | 16.9* | 5.46* |
| LSIL | 12.93* | 6.5* | - | 6.86* | 14.46* |
| HSIL | 13.12* | 16.9* | 6.68* | - | 7.01* |
| Carcinoma Cervix | 23.11* | 5.46* | 14.46* | 7.01* | - |
The ‘t’ test being significant, pointed strongly towards a –
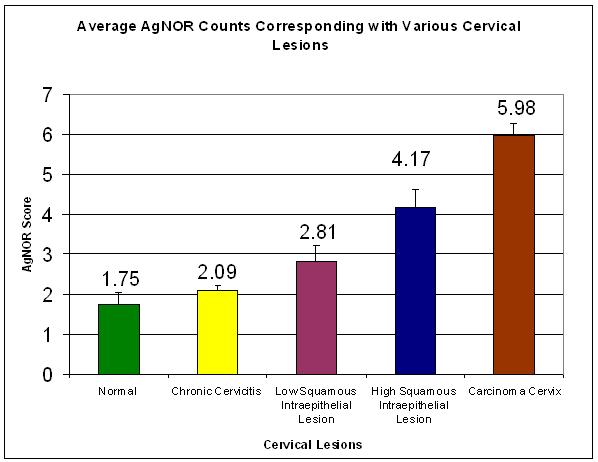
Definite correlation between the increasing AgNOR counts and the severity of the lesions [Table/Fig-6].
Average AgNOR Counts Corresponding with Various Cervical Lesions
Definite difference in the AgNOR counts between all the 5 comparisons which were made by using different cervical lesions [Table/Fig-7].
Inter comparative chart of various categories bases on Student’s unpaired t-test.
DISCUSSION
Cervical cancer is a major menace to the world. It is a serious impediment in the fight against cancer. The anatomy of the cervix makes it an ideal site for screening the premalignant changes in that organ. Cervical cancer goes through a series of preneoplastic changes or premalignant stages, which if identified on time, tend to help in intervening and preventing the cancer.
PAP smears, at times, can result in intra and inter observer errors and can be underdiagnosed or overdiagnosed. The cytopathologists can differ in their opinions, especially between the low and the high squamous epithelial lesions, while they go through the PAP stained cervical smears. To prevent a misdiagnosis with the present utilized AgNOR stain, the specific Nucleolar Organizer Regions (NORs) are highlighted on staining with the silver stains and they can actually aid in specifically knowing the cervical neoplastic status. The NOR counts keep on increasing with the frequency of severity of the lesions.
The present study was carried out purely to enhance the extensive utility of the AgNOR technique, especially its application, in cervicopathological smears. We utilized the NOR counts of the silver stained cervical scrap smears for a better understanding of the premalignant lesions and their transitions into low and high cervical intraepithelial lesions, before they got transformed into cervical cancer.
A NOR, by definition, is a part of a chromosome and the nucleolus is a structure which contains this chromosomal part. In addition, the materials which accumulate around the NOR are most notably the rRNAs, and their precursors (rDNA), as well as specific ribosomal proteins [5].
The NORs can be located by staining with silver nitrate under prescribed conditions; the structures which are thus demonstrated are termed as AgNORs. A sub cellular parameter such as a NOR, can be useful in the evaluation of the evolution of neoplastic lesions. In view of the close relationship between the NORs and the cellular activity, their size and number might reflect or predict the cell proliferation, transformation or even an overt malignancy. A correlation is thus observed between the value of the NOR and the tumour evolution.
In the present study, the total number of cases was 50
| Normal Cervix | - | 10 cases |
| Chronic Cervicitis | - | 15 cases |
| LSIL | - | 15 cases |
| HSIL | - | 06 cases |
| Carcinoma Cervix | - | 04 cases |
AgNORs are viewed as black dots within the nucleus. Most of these structures are actually nucleoli which consist of clustered AgNORs, together with dispersed AgNORs. The benign cells tend to have a regular nucleolus with tightly clustered AgNORs and the malignant cells often show dispersal of the AgNORs throughout the nucleus, as well as multiple nucleoli which contain clustered AgNORs. The quantification of the actual AgNORs, especially the intranucleolar ones, is subjective and non reproducible.
The present study, which was carried out on cervical smears, has drawn the following observations based discussion.
The AgNOR counts definitely workup as a cell proliferative marker.
The AgNOR counts increase as the cervical lesions increase in severity (cervical lesions- inflammatory, LSIL, HSIL and cervical carcinoma)
The AgNOR counts follow a definitive range of the NOR counts in correlation with the individual lesions.
Assessing a NOR count gives a substantial idea about the kind of cervical intraepithelial lesion or malignancy, thereby immensely aiding in the PAP based cervical smear diagnosis.
Significant differences in the AgNOR counts were observed in the cervical lesions. In the present study, it was observed that the AgNOR counts in the cervical lesions gradually tended to increase with the severity of the lesions i.e. from a normal cervix to chronic cervicitis to LSIL to HSIL and finally, carcinoma of the cervix had the highest score. However, the present study found a narrow margin of difference in the AgNOR counts between a normal cervix and chronic cervicitis and between chronic cervicitis and LSIL. An obvious difference in the counts was found between chronic cervicitis and HSIL, between LSIL, HSIL and carcinoma of the cervix and between HSIL and carcinoma of the cervix. (as has been depicted in [Table/Fig-8,9,10,11,12].
Normal Cervix Stained With Silver Stain Showing Predominantly 1 Dot (Nor)/ Cell
Chronic Cervicitis Stained With Silver Stain Showing Predominantly 2 Dots (Nor)/ Cell
Low Squamous Intraepithelial Lesion Stained With Silver Stain Showing 2- 3 Dots (Nor)/ Cell
High Squamous Intraepithelial Lesion Stained With Silver Stain Showing 3-4 Dots (Nor)/ Cell
[Table/Fig-12]: Cervical Carcinoma Lesion Stained With Silver Stain Showing 4-5 Dots (Nor)/ Cell
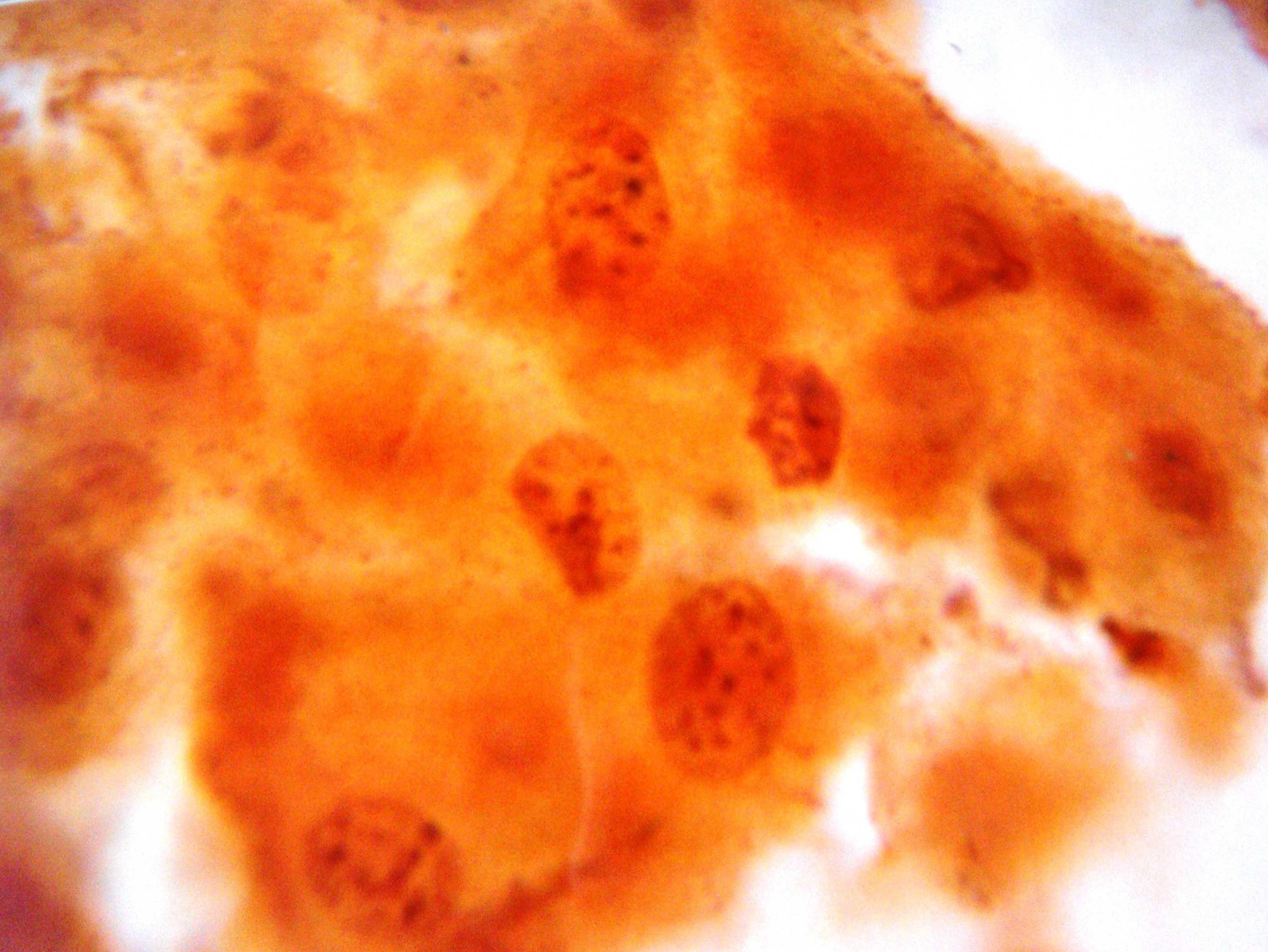
As the lesion progressed towards severity i.e. from cervicitis to LSIL to HSIL and finally to carcinoma of the cervix, the NOR dots also increased, thereby raising the average AgNOR count of that case. It thus indicated that NOR had the property of ploidy and that the proliferation of NOR was related to the increase in severity of the lesion. So NOR ultimately behaved as a tumour proliferative marker. (as has been depicted in [Table/Fig-3 & 6].
The factors that can alter the AgNOR counts (diminished AgNOR results) are - improper collection of the smears, not collecting them from the proper sites/ lesions, inadequate cellularity, inter and intra observer errors, etc. Besides this, the cervical smear results are directly related to the staining reagent. The staining reagent should be freshly prepared [6].The following are the major significant AgNOR studies of similar interest which have been carried out in the cervix.
Parallels have been drawn between them and the present study:
The study which was carried out by Kaushik R et al., in 2003 included 100 cases of cervical biopsies and categorized them as cervicitis, CIN I, CIN II, CIN III and Ca Cx. All of the categories in this study showed significant variations in the AgNOR counts (p<0.001). Our study showed the AgNOR dot counts as normal (1.75) , chronic cervicitis (2.09), LSIL(2,81), HSIL(4.17) and CaCx (5.48). The only parameters which had a very narrow range of demarcation in the AgNOR ratio was cervicitis and LSIL [7].
The study of Sławomir Terlikowski et al., (2004), sought a correlation between the number of AgNOR granules and the degree of the Cervical Intraepithelial Neoplasia (CIN). Thirty-five sections (5 normal,10 CIN1, 10 CIN2 and 10 CIN3) were subjected to a retrospective analysis. The number of granules per 100 cells was also found to be increased with the degree of CIN. It can be thus concluded that the number of cells with 4 and more AgNOR granules can serve as a CIN differentiation exponent. The findings of these studies correlate strongly with those of our study, i.e the number of cells with 1 dot decreased with the increasing grade of the intraepithelial lesion (LSIL/HSIL). Also, the number of cells with 4 dots or more, increased with the increasing grade of LSIL/ HSIL [8].
Misra JS et al., in 2005, studied 50 cervical smears of cytologically diagnosed normal inflammatory low grade SIL, LSIL and squamous cell carcinoma. In the normal and the inflammatory smears, the AgNOR dots ranged from 1 to 2. The LSIL dots ranged from 2 to 4 and the HSIL dots ranged from 6 to 8. The frank squamous cell carcinoma had 10 dots. The above values which are mentioned, correlated with those of the present study [9]. Singh U et al., in 2006, found significant AgNOR scores in cervical biopsies. They found a definitive increase in the AgNOR dot score with the progression of the lesions I.e. the AgNOR count in CIN I was 1.64, that in CIN II 2.68 and that in CIN III 4.3.
The differences in the AgNOR counts between CIN I and CIN II, between CIN II and III, and between CIN I and CIN III were statistically significant. Our study which was done on cervical smears which were stained with silver colloid stains, deduced similar findings, i.e there was a progressive rise in the AgNOR counts with the severity of the lesions (normal cervix< chronic cervicitis< LSIL<HSIL<carcinoma of the cervix i.e. 1.75 < 2.09 < 2.81 < 4.17< 5.98 respectively) [10].
Alarcón-Romero LC et al., in 2009, worked extensively on the AgNOR counts in cervical intraepithelial lesions and carcinoma of the cervix.
The polymorphism of the AgNORs rises progressively according to the grade of the histological lesions. This can be useful as a prognosis for the progression of squamous cell carcinoma. The present study which was done on precancerous and cancerous lesions of the cervix, similarly showed that the AgNOR was valuable as a cellular activity marker and as well as a marker of malignancy [11].
CONCLUSION
The present study found a significant correlation between the NORs and the cervical lesions. The NORs within the nucleus of the squamous cells have a definitive proliferative activity with the severity of the cervical pathology. The AgNOR granules or dots tend to increase as the severity of the cervical lesion progresses. Ultimately, the highest number of NORs was reported in the cytological sampling of patients of carcinoma of the cervix. Though the cervical pathology of inflammatory origin as well as the early dysplastic changes in the squamous lining epithelial had a low discriminatory index or score as compared to that of the normal cervix cytology, the NOR served tremendously in differentiating the cytological smears of HSIL from those of LSIL, as well as those of carcinoma of the cervix amongst one another.
The AgNORs in cervical cytology can act as an important adjunct with their counterpart, the PAP stained smears and help in bringing about a final diagnosis, thus making an immense difference in the patient’s premalignant management and prognosis. This entire study put forward a strong emphasis on the fact that the AgNORs can be declared a definite index for assessing the cell proliferation. However, on the context of AgNORs being declared as a tumour marker, a further, extensive, long term research would be recommended.