The introduction of modern diagnostic imaging techniques, mainly ultrasonography (USG), has enabled the detection and location of lesions in sites which are not easily accessible to surgical biopsies, besides offering vast opportunities for fine needle aspiration of the deeper structures. Samples may be obtained from the deeper structures as the first step in the laboratory investigation, thereby, quickly satisfying the avidity of clinicians for a rapid diagnosis. USG- guided fine needle aspiration is a readily accepted, rapidly growing and an important diagnostic technique which is an accurate, safe, simple, rapid, and an efficacious method which can be used for rendering a cyto-histologic diagnosis in space occupying lesions of the abdomen and also for the confirmation of the suspected malignant masses in various intra-abdominal and pelvic locations. The basic principle of an ultrasound guided FNAC is that, the rather complicated three-dimensional problem of hitting a small target is converted to a much simpler two dimensional imaging technique.
Ultrasonography offers several advantages as a biopsy guidance system. It is readily available, relatively inexpensive and portable; it uses no ionizining radiation and it can provide guidance in multiple planes such as transverse, longitudinal and oblique. The greatest advantage however, is that, it allows real time visualization of the needle tip as it passes through the tissue planes into the target area. It has been demonstrated that ultrasound can precisely guide needle biopsies in lesions which are as small as 1cm, in critical anatomical areas. This precision is necessary for a successful procedure and it often makes sonography the first choice in guiding interventional procedures. An intra-abdominal mass is an enigma in the surgical practice. Fine needle aspiration of abdominal masses has gained tremendous popularity, since it can have a major impact on the management of the patients and in many cases, it may obviate the diagnostic surgical procedures or expedite the planning for the therapy. Ultrasound guided fine needle aspiration can be utilized for practically any mass in the abdomen, pelvis, mediastinum, lung/ pleura, thyroid, parathyroid, and the cervical nodes.
Aspiration cytology helps in differentiating the cystic versus the solid lesions, the benign versus the malignant neoplasms, or an abscess versus a neoplasm. Occasionally, FNAC does not yield information which is sufficient for making a precise diagnosis. The presence of a pathologist during the aspiration procedure provides a combined consultation between the pathologist and the radiologist. This leads, not only to a better clinical correlation, but it can also lead to a suggestion of additional biopsy sites and samplings for special procedures such as culture or gram staining in abscesses and immunophenotyping or PAP staining in malignancies or any other means of confirmation. The present study was undertaken to critically analyze the usefulness of ultrasound guided fine needle aspiration cytology in the diagnosis of intra-abdominal and pelvic masses and to evaluate the accuracy of aspiration cytology in comparison to a histologic diagnosis.
MATERIALS AND METHODS
This study involved 90 cases with clinically or ultrasonographically diagnosed abdomino-pelvic masses, who were referred for FNAC to the Department of Pathology, Mysore Medical College and Research Institute Hospital, Mysore, Karnataka, India during the period from 2008-2011. A majority of the patients presented with a mass per abdomen and/or pain in the abdomen. Detailed clinical data which included the patients’ history, physical examination findings and reports of relevant investigations which were conducted (routine and special), were recorded. The coagulation profile was routinely done in all the patients with abdomino-pelvic masses. Only those patients with normal coagulation profiles were selected for the study.
Before posting the patients for the procedure, the absolute indications and contraindications for FNAC of the abdominal masses were kept in mind, the absolute indications being right hypochondrial masses without definite clinical diagnoses, suspected focal hepatic lesions and specific liver conditions like primary and secondary liver malignancies, hepatic abscesses and deep seated hepatic vascular and cystic tumours. The contraindications which were considered were patients with haemorrhagic tendencies and prolonged PT, suspected extra-hepatic obstructive jaundice, hepatic surface hemangioma and echinococcosis and unco-operative patients. The patients were subjected to a ultrasonographic evaluation to assess the origin of the mass and its relationship with the adjacent organs. A percutaneous FNAC of the mass was done under real-time USG guidance, in the Department of Radiology, while taking absolute aseptic precautions, by the shortest route to the site, as was suggested by the sonologist. A 10ml disposable plastic syringe and a 22 gauge needle were used. For deep-seated lesions, a 20-22 gauge spinal needle of 9cm length was used. A trans-abdominal approach, by using the most direct route was made and the standard FNAC procedure was followed. Each aspirate was smeared on an average of four to five slides, all of which were immediately wet-fixed in 95% alcohol fixative. The MGG and Papaincolaou stains and special stains like Periodic Acid Schiff were employed wherever necessary. Only those cases with adequate material for a cytodiagnosis were taken up for the study and those with histopathological correlations were considered for statistical analyses.
OBSERVATIONS
The applicability of USG guided FNAC for the pre-operative diagnoses of abdomino-pelvic masses, was assessed in 90 patients . A majority of the patients were females and most of the patients were between 21-30 years and 51-60 years of age. The site of origin of most of the abdomino-pelvic masses was the uterus and the ovary (40%), followed by the intestine (23%) and the liver(15%). A majority of the lesions were malignant (64.5%), followed by nonneoplastic (20%) and benign (5.5%) lesions [Table/Fig-1].
Distribution pattern of non neoplastic, benign and malignant lesions
| Lesions | Number | Percentage(%) |
|---|
| Benign | 14 | 15.5 |
| Malignant | 58 | 64.5 |
| Non-neoplastic | 18 | 20.0 |
| Total | 90 | 100 |
Among the non-neoplastic lesions, a majority were appendicular abscesses and non-specific inflammatory lesions (22.3% each), followed by 16.7% ileocaecal tuberculosis lesions, 11.2% liver abscesses and 5.5% each of tubo-ovarian abscesses and empyema, hydatid cyst [Table/Fig-2], hydatidiform mole and haematoma. Most of the benign neoplasms were ovarian surface epithelial tumours. A majority of the malignant neoplasms were pelvic in origin (32.7%), followed by intestinal (31%) and hepatic (18.9%) lesions [Table/Fig-3].
Hydatid cyst of liver showing laminated membrane x40X(MGG)
Site of distribution of malignant neoplasms
| Site | Number | Percentage(%) |
|---|
| Uterus and ovary | 19 | 32.8 |
| Intestine | 18 | 31.0 |
| Liver | 11 | 19.0 |
| Retroperitoneum | 3 | 5.3 |
| Stomach | 2 | 3.4 |
| Gall bladder | 2 | 3.4 |
| Abdominal Lymphnode | 2 | 3.4 |
| Bile duct | 1 | 1.7 |
| Total | 58 | 100 |
Among the malignant neoplasms, a majority were malignant, surface epithelial tumours of the ovary. A histopathological correlation was available in 69 cases, by using which the statistical data was calculated [Table/Fig-4].
Histopathological correlation and diagnostic accuracy
| Lesion | Number of cases diagnosed on FNAC | Histopathological | Other means of confirmation* | Dignostic accuracy (%) |
|---|
| Available | Consistent |
|---|
| Benign | 14 | 13 | 13 | 100 |
| Malignant | 58 | 50 | 48 | 96 |
| Nonneoplastic | 18 | 18 | 17 | 94.4 |
| Total | 90 | 81 | 78 | 96.3 |
The diagnostic accuracy rates of USG guided FNAC for benign, malignant and non-neoplastic lesions were 100%, 96%, and 94.4% respectively. The overall accuracy rate was 96.3%. The sensitivity and the specificity of this study were 94.1% and 100% respectively [Table/Fig-5]. In the present study, no false positive diagnosis was encountered.
Overall results of the study
| Indices | Percentage (%) |
|---|
| Sensitivity | 94.1 |
| Specificity | 100 |
| Overall accuracy | 96.3 |
| Positive predictive value | 100 |
| Negative predictive value | 90.9 |
DISCUSSION
Ultrasound guided FNAC is a rapid, accurate, economical and a safe diagnostic procedure that can be used in various neoplastic and non-neoplastic diseases. As a diagnosis is rapidly available on FNAC, the appropriate medical or surgical therapies can be started earlier, thus avoiding unnecessary, expensive and often invasive diagnostic procdures [1]. The aforesaid factors reduce or eliminate the surgical morbidity and mortality as well as the hospitalization, thereby benefitting the patients as well as the healthcare system. In the present study, it was observed that a majority were malignant lesions which comprised 64.5% lesions and the remaining 35.5% were benign and non-neoplastic lesions. This was almost similar to the study of Smith et al., [2] in which 66% were malignant lesions and 34% were benign/ non-neoplastic lesions. Though the technique of obtaining material by aspiration in a case of hydatid cyst is simple, the procedure is hazardous due to a risk of anaphylaxis, leakage of fluid, secondary cyst formation and bacterial infection [3]. No such complication was encountered in the present study.
Abdominal tuberculosis continues to pose a diagnostic challenge for the clinicians [4]. In patients with abdominal tuberculosis whose presentations are insidious, an abdominal mass is cited the most common finding. It is in this group of patients that fine needle aspiration can be performed as an ambulatory procedure, to obtain a tissue diagnosis, thereby obviating a surgery. In the present study, three cases of intestinal tuberculosis, with AFB (Acid Fast Bacilli) positivity, were diagnosed on cytology alone and they responded to a therapeutic trial of the Anti-Tuberculosis Chemotherapy (ATT).
Among the benign neoplasms in the present study, a majority comprised of surface epithelial tumours and teratomas of the ovary [Table/Fig-6 & 7], followed by a uterine leiomyoma, a luteoma, a neurofibroma, a desmoid tumour and a retroperitoneal teratoma. Ganjei P et al., [5] observed in their study, that serous cystadenomas exhibited great variations in the colour and volume of the aspirated cyst fluids. They also observed that the epithelial cells which were aspirated from the serous cystadenomas showed some non-specific features which were in contrast to those of the mucinous cystadenomas. The observations of the present study were similar to these findings. Two cases of ovarian surface epithelial neoplasms posed a diagnostic confusion in the present study, since the cytological features favoured borderline malignant features and the report was signed off as “suspicious of malignancy”. They were subsequently diagnosed as “invasive cystadenocarcinomas” on histopathology. As was observed in the present study, ovarian tumours with a borderline malignant potential may present diagnostic dilemmas on cytology and histopathology seems to remain the gold standard in the definitive diagnoses of these grey zone lesions. Uterine leiomyoma, in the present study, yielded scant material on repeated aspirations as in any other study and it showed only few clusters of benign spindle cells with blunted nuclei.
Serous cystadenoma showing sheets and papillary aggregates of small bland epithelial cells x10X(H&E)
Benign cystic teratoma showing nucleated and anucleated squamous cells x10X(H&E)

FNAC has been widely used in the diagnoses of recurrent and metastatic gynaecological malignancies. In our experience also, FNAC which was done in ovarian tumours was found to be a relatively safe procedure and an accurate, pre-operative identi- fication of the nature of the tumour was possible in a majority of the cases [Table/Fig-8]. The diagnostic accuracies for benign and malignant neoplasms of the ovary and the pelvis were 100% and 88.2% respectively.
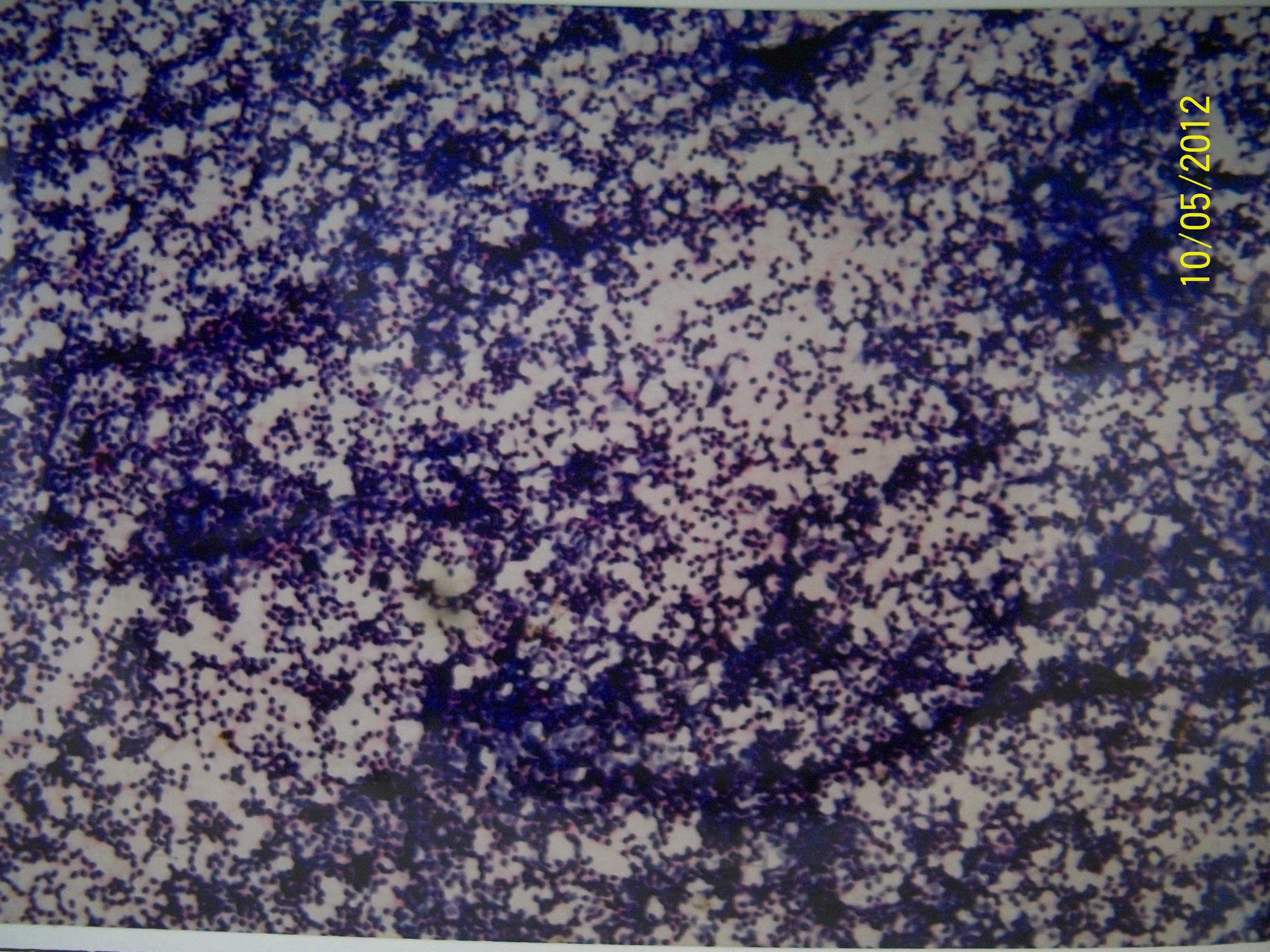
Dysgerminoma showing cellular smears with dispersed population of round-oval cells with interspersed lymphocytes against tigroid background. x10X(H&E)
Punctation of the cystic ovarian tumours could be hazardous, which can cause leakage and a potential tumour-cell implantation in the case of malignant tumours. Kjellgren has suggested that this risk can be reduced significantly by doing a trans-vaginal or a trans-rectal aspiration [6]. In the present study, though the approach was trans-abdominal in all the cases, no such complications were encountered. Besides this, the FNAC diagnosis was helpful, especially in young patients with unilateral ovarian masses, for the prospect of a conservative surgery, in order to preserve the fertility.
Among the gastro-intestinal lesions, tuberculosis and adenocarcinomas posed no problem on the cytodiagnosis [Table/Fig-9]. But, as was expressed by other investigators, cytology alone definitely posed difficulties in the diagnosis of Non Hodgkin’s Lymphomas (NHLs).This was due to the close resemblance of the tumour cells of NHL to those of any other small round cell tumour [Table/Fig-10]. But on correlation with a complete history, physical examination, radiological findings and cytologic features, like a lack of cellular cohesion and a monotonous population of tumour cells and nuclei with peppered chromatin, a cytological diagnosis of NHL was offered, which was subsequently confirmed by histopathology. The cytomorphological diagnosis of NHL helped in initiating the therapy at the earliest, as a live-saving measure. FNAC, coupled with USG guidance, yielded a high diagnostic accuracy rate in gastro-intestinal lesions, which was in contrast to the accuracy rate which was noted in the study which was undertaken without a radiological guidance by Khanna et al., [7].
Gastric adenocarcinoma showing cells with large hyperchromatic nuclei ,abundant vacuolated cytoplasm and occasional signet-ring cellsx40X(H&E)
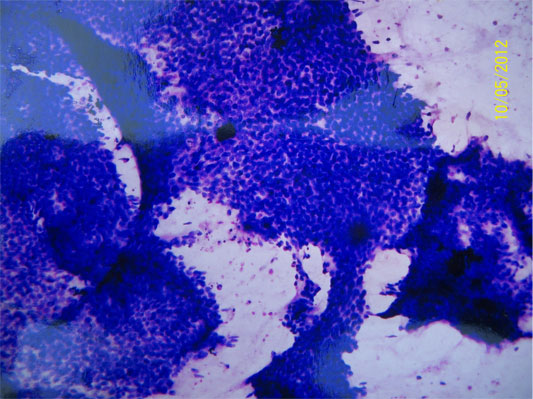
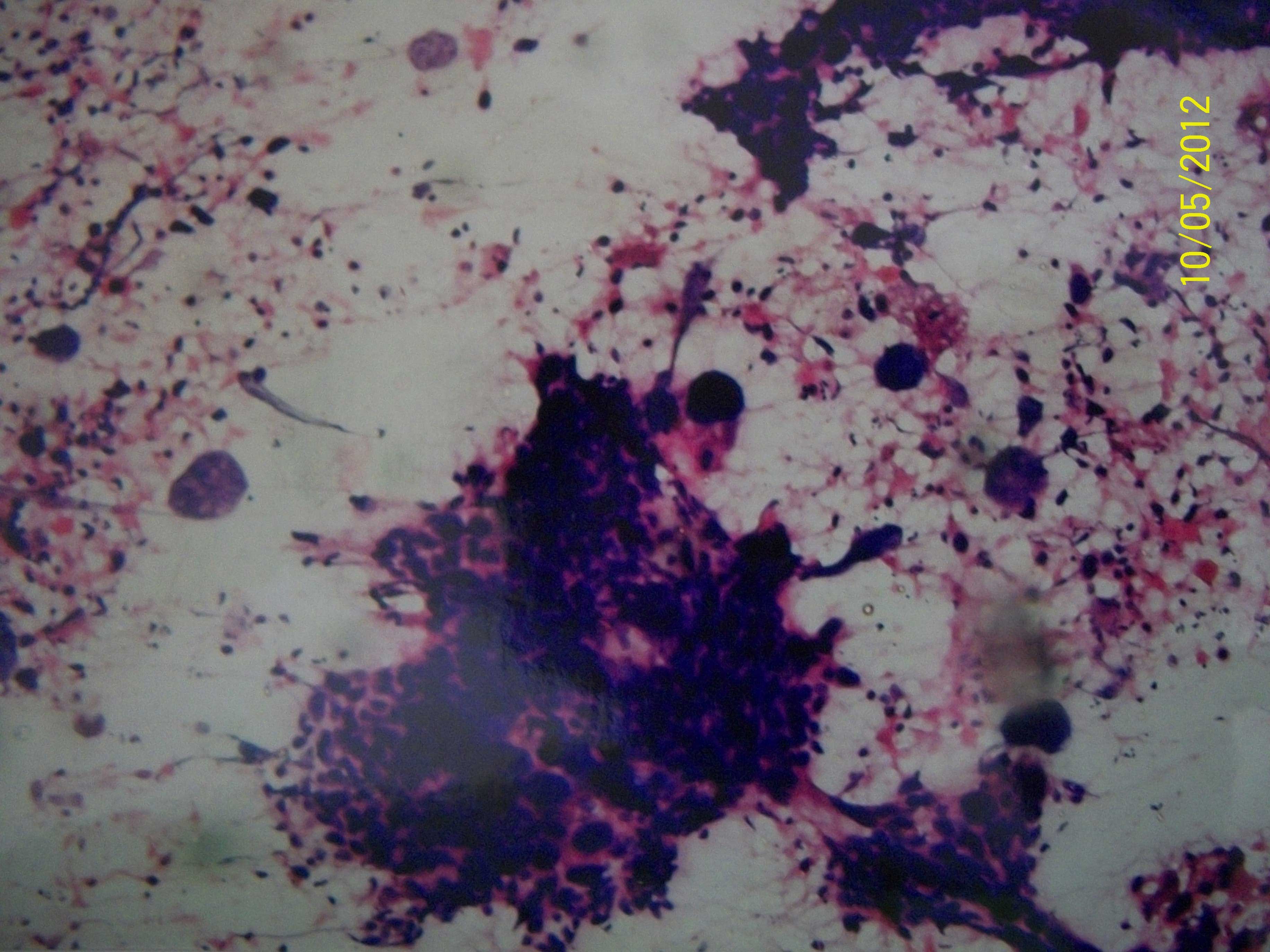
Non Hodgkin’s lymphoma showing cleaved and noncleaved with peppered chromatin x40X(MGG)
Among the hepatic lesions, a majority were hepatocellular carcinomas (40%) [Table/Fig-11 & 12], which was comparable with the results of the study of Tatsuta et al., [8]. But in the studies of Montali et al., and Pinto et al., [9] a majority of the cases were metastatic deposits in the liver. As was stated by Pilotti et al. the most common diagnostic problem which had to be solved by using an FNAC procedure in the liver, was to distinguish a primary from a secondary tumour. This was a reflection of the limitations of the non-invasive radiologic methods such as USG and CT scan, which are usually employed for the preliminary workup of these lesions. Though hepatocellular carcinoma is a very vascular tumour and is prone for a spontaneous rupture causing haemoperitoneum, no such complication was encountered in the present study. The present study showed high rates of sensitivity by Montali et al., and Tastuta et al. FNAC of hepatic masses has proved to be a safe and an accurate method for diagnosing tumours in this site. The present study also showed that use of USG for guiding the needle, increases the sampling accuracy of the aspirates.
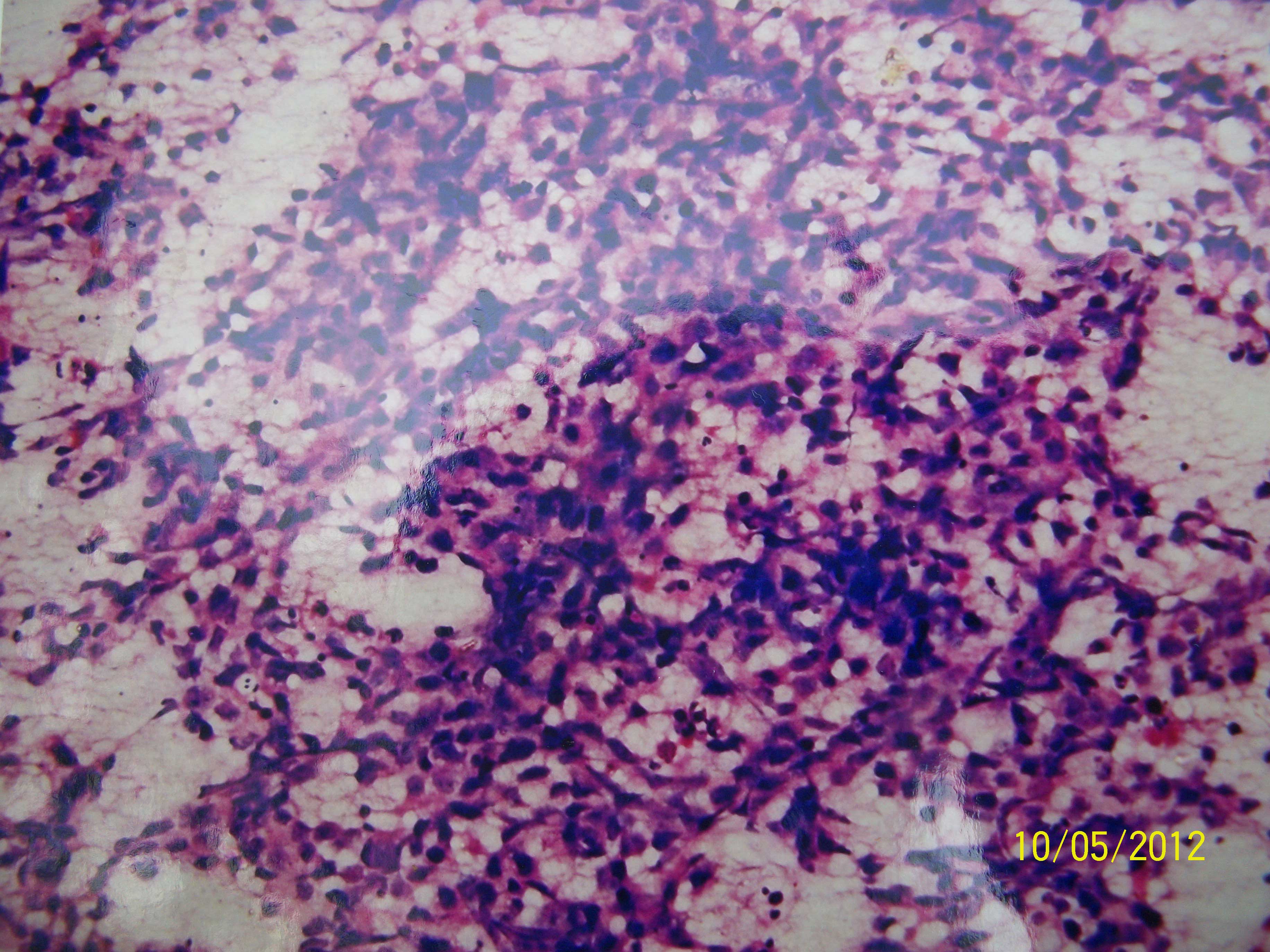
Moderately differentiated hepatocellular carcinoma showing moderately pleomorphic tumor cells,tumor giant cells and endothelial strands traversing cell groups x10X(H&E)
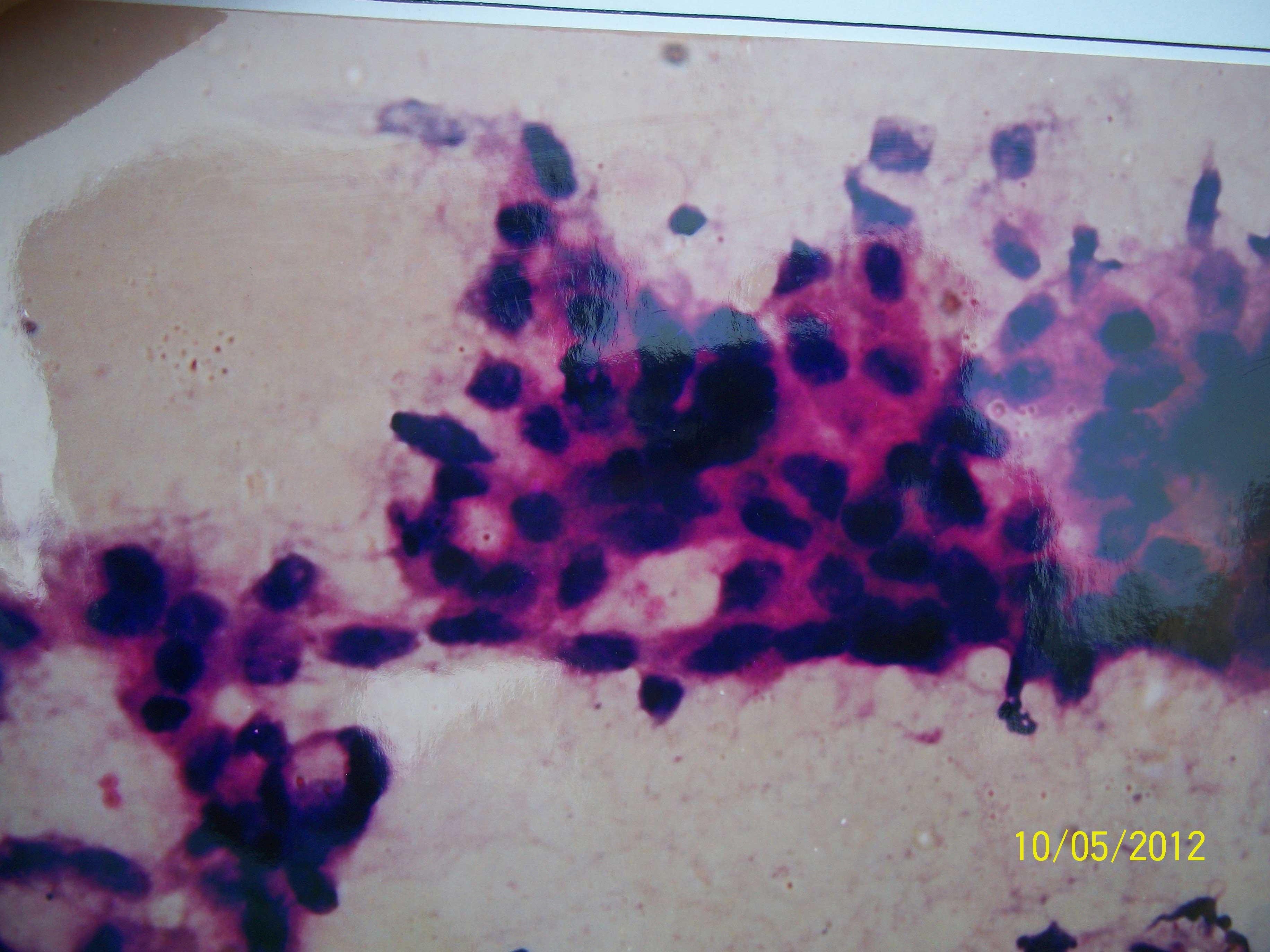
Well-differentiated HCC showing sheets of malignant hepatocytes with round nuclei and prominent nucleoli x 40X (H&E)
Among the gall bladder lesions, a cytologically diagnosed case of a non-specific inflammatory lesion, proved to be a papillary adenocarcinoma of the gall bladder on histopathology. The false negative diagnosis in this case could be attributed to a sampling error, wherein the needle might have missed the target lesion, as it was surrounded by an extensive inflammatory infiltrate. Akosa AB et al., [10] found that FNAC of the gall bladder had a sensitivity of 88% and a diagnostic accuracy of 69% in their series, and they suggested that FNAC which was performed under USG or fluoroscopic guidance during a per-cutaneous trans-hepatic cholangiography would ensure an earlier diagnosis of gall bladder carcinoma and the planning of the appropriate surgery. The diagnostic accuracy (66.6%) of the present study in biliary lesions was comparable with the findings of the study of Desa et al.,(67%).
Regarding the retroperitoneal lesions, Gupta RK et al., [11] stated that FNAC was not only useful in the diagnosis of the space-occupying lesions of the retroperitoneum, but that it could also help in choosing the appropriate management. In concurrence with the findings of the present study and as was observed by many authors, the main drawback of FNAC in these lesions was that the sampling could be performed only on parts of the tumour, the structure of which was different in different fields. This has been specially true in the retroperitoneal tumours, which often attain huge dimensions.
Two cases of para-aortic lymph nodes were encountered in the present study and both the cases showed metastatic deposits. One of the cases showed poorly differentiated adenocarcinomatous deposits and the other showed secondary deposits from a mixed germ cell tumour of the testis [Table/Fig-13]. But a histopathological confirmation was not possible due to the non-availability of biopsies, as the patients were referred to a higher centre for further management. Krishna et al., [12] in their study of these lesions, noted that, the high false positive rates could be reduced if the FNAC was done under USG guidance. The present study also showed a high sensitivity rate and a diagnostic accuracy rate which were in close comparison to those of the studies of Civardi et al. and Stewart CJR et al.
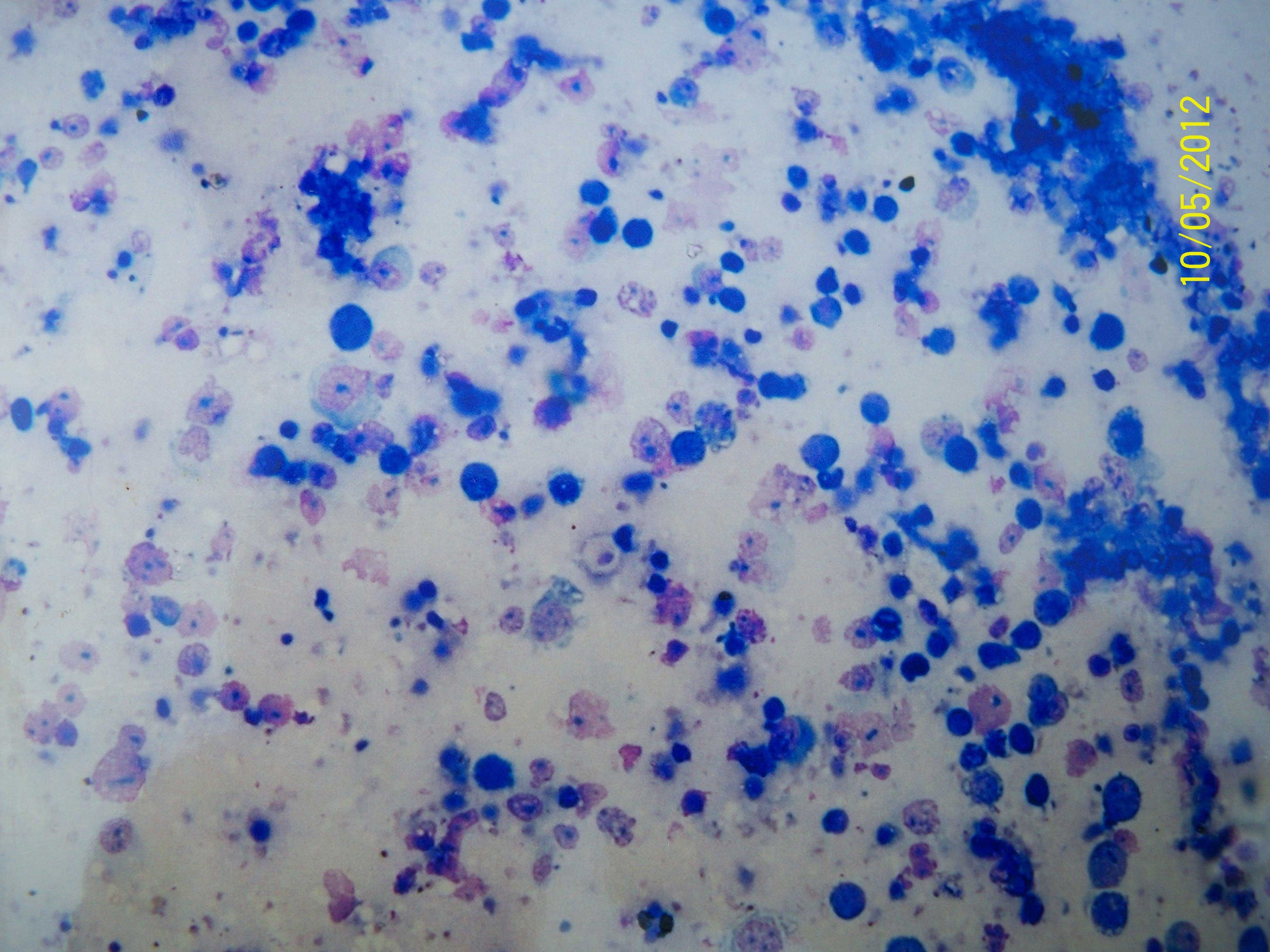
Seminoma showing dispersed population of round-oval cells having prominent nucleoli and indistinct cytoplasm with interspersed lymphocytesx10x(MGG)
CONCLUSION
USG guided FNAC is a rapid, cost effective , accurate, non-invasive and a safe diagnostic procedure which can be conveniently used in various abdomino-pelvic masses, thereby avoiding unnecessary, expensive and often invasive diagnostic procedures. It is a highly accurate procedure which can be done on an outpatient basis. It can be pre-empt a lengthy and an expensive workup in the search for a primary tumour. It has emerged as a reliable method which involves minimal/ no risks and complications. USG guided FNAC, as the first line investigation, is not only useful in the diagnosis of deep seated, inaccessible and spaceoccupying lesions, but it also helps in choosing the appropriate management.