LRTIs are a persistent and a pervasive health problem which impose an enormous burden on the society. They being common reasons for consultation and hospitalization [1,2], the patients present with a wide spectrum of diseases which range from minor self limiting illnesses to potentially life threatening infections [2,3]. The outcome depends on the virulence of the organism and the host defense mechanism. The bacteriological profiles of the LRTIs are different in different countries, which vary with time within the same country. The aetiologies of respiratory infections play a significant role in the decision making, as they concern the choice of empirical antibiotics, isolation and hospitalization measures. A variety of organisms are usually implicated in their aetiologies, the most common ones being gram negative bacteria [4–7], followed by gram positive organisms.Specific microbiological investigations are essential for minimizing the consequent development of complications and for improving the outcomes. The dramatic rise in the antimicrobial resistance among the respiratory pathogens [3,4], presumably due to the prophylactic administration of anti bacterial therapy even before the availability of the culture results, is a matter of potential concern worldwide. This study has reviewed our current understanding on lower respiratory tract infections and it has emphasized the changing trends in their occurrence and the anti microbial susceptibility pattern of the respiratory pathogens which were isolated in a tertiary care setting, thus enabling the clinicians to appropriately formulate and endorse a competent and rational anti bacterial policy, to further curb the incidence of the disease.
MATERIALS AND METHODS
A prospective analysis was carried out at a Medical College Hospital In North Kerala, India from April 2011 to March 2012, after getting a clearance from the ethical committee. The respiratory samples which were collected were sputum and broncho alveolar lavage fluid. The early morning sputum samples were collected after giving proper instructions to the patients, in a sterile container and the broncho alveolar lavage fluid was collected aseptically in a sterile container by aspirating the saline which was injected through a fi- beroptic bronchoscope, from the patients which were on mechanical ventilation for at least three days in the medical intensive care units, which were transported promptly within two hours to the microbiology lab. These clinical samples which were received from the patients of all the age and sex groups, with symptomatologies which were suggestive of LRTIs, were processed by the standard laboratory methods. The samples which were received from new patients who were enrolled for the first time, were included in the study. The sputum samples were assessed for their quality by using Barlett’s grading system. The specimens with an average Q score of zero or less were rejected and bronchial secretions with less than 103CFU/ml were regarded as commensals or contaminants [8]. The isolates which were identified as contaminants or commensals were excluded from the study. The respiratory pathogens were identified by their morphologies and their cultural and biochemical characteristics. The susceptibility profiles of the positive bacterial isolates were determined by the modified Kirby-Bauer disk diffusion method on Mueller-Hinton agar, as per the CLSI guidelines [9]. Their sensitivities to amoxicillin/clavulanic acid (30μg), cipro- floxacin (5μg), ofloxacin (5μg), levofloxacin (5μg), amikacin (30μg), cefepime (30μg), cefuroxime (30μg), ceftazidime (30μg), ceftriaxone (30μg), cotrimoxazole (1.25/23.75μg), aztreonam (30μg), imipenem (10μg), cefoperazone/sulbactum (75/10μg), and piperacillin/ tazobactum (100/10μg) were determined. Klebsiella pneumoniae ATCC 700603, Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as the control strains for the identification and the anti microbial susceptibility testing of the isolates. The data was analyzed and interpreted by using the WHO Net Antibiotic Susceptibility Surveillance Software.
RESULTS
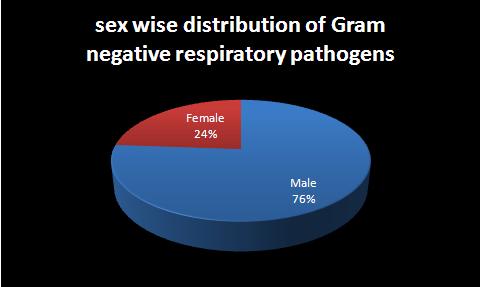
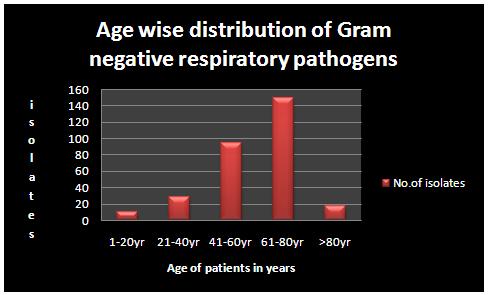
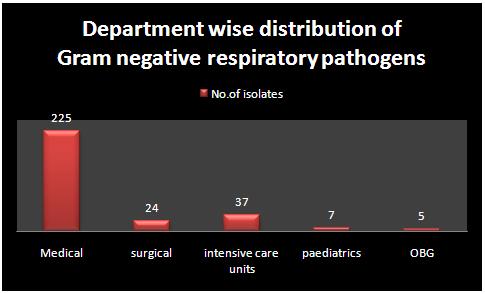
Among the 1750 respiratory samples, 298(17.03%) were found to be positive for bacterial isolates. 227 samples (76.17%) from among males and 71 samples (23.83%) from among females were culture positive, thus showing a male sex predilection [Table/Fig-1]. The highest isolation rate was observed in the 61-80 years (50%) age group [Table/Fig-2]. This age group showed an increased vulnerability to LRTIs in the geriatric population, presumably, due to the various age related physiological changes. Irrespective of the age group, Klebsiella pneumonia (41.95%) was found to be the predominant organism which was isolated, followed by Pseudomonas aeruginosa (26.84%) [Table/Fig-3]. A majority of the culture positive isolates were obtained from the medical departments (75.50%), followed by the intensive care units (12.42%) and the surgical departments (8.05%). The resistance among the respiratory pathogens to the agents that have traditionally been recommended as the first line therapy, is on the rise. The gram negative bacteria which were isolated, displayed higher resistance patterns towards most of the widely used Cephalosporins [Table/Fig-4]. Klebsiella pneumonia exhibited a higher sensitivity towards imipenem (90%), followed by piperacillin/tazobactum (72.7%). Pseudomonas aeruginosa showed a relatively lesser resistance towards the flouroquinolones than Escherichia coli and Klebsiella pneumoniae. A monotherapy with imipenem demonstrated significant susceptibility patterns and it was found to be effective against a majority of the isolates; especially Pseudomonas aeruginosa and Escherichia coli showed nil resistance to it.
Sex-wise distribution of Gram negative respiratory pathogens isolated
Age-wise distribution of Gram negative respiratory pathogens isolated
Gram negative respiratory pathogens isolated
| Organism | No. of isolates | Percentage isolation |
|---|
| Klebsiella pneumonia | 125 | 41.95 |
| Pseudomonas aeruginosa | 80 | 26.84 |
| Escherichia coli | 46 | 15.44 |
| Acinetobacter baumanii | 24 | 8.05 |
| Citrobacter koseri | 20 | 6.71 |
| Moraxella catarrhalis | 2 | 0.67 |
| Citrobacter freundii | 1 | 0.34 |
Resistance pattern of gram negative respiratory pathogen isolated
| Antibiotics | K.pneumonia | P.aeruginosa | E. coli | A.baumanii | C.koseri | M.catarrhalis | C.freundii |
|---|
| Amoxyclav | 91.7 | 100 | 68.8 | 100 | 75 | 50 | 100 |
| Cotrimoxazole | 67.9 | ND | 91.3 | 87 | 52.9 | 100 | 100 |
| Cefepime | 80.9 | ND | 72.2 | ND | ND | ND | ND |
| Cefuroxime | 83.3 | ND | 91.7 | 100 | 78.9 | 0 | 100 |
| Ceftriaxone | 76.5 | ND | 74.1 | 94.4 | 64.7 | 0 | 100 |
| Ceftazidime | 84.1 | 40.4 | 57.1 | 100 | ND | ND | ND |
| Ciprofloxacin | 59.1 | 23.9 | 81.8 | 87.5 | 57.1 | ND | 100 |
| Ofloxacin | 70.8 | 40 | 76.9 | 84.2 | 50 | 50 | ND |
| Levofloxacin | 52.3 | 31.4 | 68 | 42.9 | 47.4 | 50 | ND |
| Amikacin | 34.3 | 13.5 | 7.2 | 61.9 | 10 | 0 | 0 |
| Aztreonam | 88.9 | 0 | 80 | 90.9 | 66.7 | ND | ND |
| Imipenem | 7.8 | 0 | 0 | 4.8 | 6.7 | ND | 0 |
| Cefoperazone/Sulbactum | 23.6 | 14 | 6.9 | ND | ND | ND | 0 |
| Piperacillin/Tazobactum | 18.2 | 1.9 | 3.6 | 16.7 | 8.3 | ND | 0 |
DISCUSSION
Respiratory tract infections are the second most common cause of hospital acquired infections. A detailed evaluation of the patients, which starts with a history taking, along with underlying co morbidities, and a comprehensive rapid clinical examination, is a fundamental part of the medical management. Potentially, a more rapid and a more frequent aggravation can be anticipated in elderly patients with cardiac or respiratory co-morbidities, chronic alcoholics, immunocompromised hosts, HIV patients, in those with cystic fibrosis, and Diabetes mellitus, etc. Most of the cases result from bacterial infections which warrant an antibiotic therapy as the mainstay of the treatment. The microbiological diagnosis of LRTIs is often challenging, as the specimen collection for the investigation entails the hazard of contamination by the microbes which reside in the upper respiratory tract, thus raising the need for sophisticated invasive procedures.
An appropriate application of the clinical and laboratory findings can point towards an accurate diagnosis. The emerging resistance to the anti microbial agents despite the advances in therapeutic and preventive measures, is a growing concern which is faced by the clinicians worldwide, thus raising significant concerns. The indiscriminate and the irrational usage of antimicrobials has further contributed to the emergence of resistance, which may turn out to be a leading cause for morbidity and mortality in the developing countries. Tackling this issue has become a major quest.
The present study provides an insight on the prevalence and the antibiogram of the respiratory pathogens which were isolated in this part of North Kerala, India. Klebsiella pneumoniae (41.95%) was the predominant organism which was isolated, followed by Pseudomonas aeruginosa (26.84%), as is shown in [Table/Fig-3], which was in concordance with the findings of similar studies which were done by V.Olugue et al.,[3], Kaul et al.[10] and Akingbade OA [6].
The rate of isolation was higher in males (76.17%), which revealed an increased susceptibility to the LRTIs in the male sex than in females (23.83%), as has been shown in [Table/Fig-1], which was in comprehension with the findings of similar studies which were done by Shah, et al. [2], V Olugbue et al. [3] and Akingbade O [6].
The analysis of the age wise data portrayed an increased prevalence in the 61-80 years age group (50%), as shown in [Table/ Fig-2], which was at par with the findings of the studies which were done by Shah, et al., [2] and Mandell et al., [11]. The increased vulnerability in the geriatric population maybe due to their age related physiological and immunological changes and other co-morbidities.
The department wise isolation rate was higher in the medical wing (general medicine, respiratory medicine, dermatology, etc) (75.50%), followed by that in the intensive care units (12.42%), as has been shown in [Table/Fig-5] .This may mostly be due to the patients with respiratory tract infections who presented to the general medicine or the respiratory medicine departments.
Department-wise distribution of Gram negative respiratory pathogens isolated
The antimicrobial resistance among the respiratory pathogens is a major barrier that might interfere with an effective treatment. This study depicts the anti microbial susceptibility patterns among the gram negative, respiratory pathogens which were isolated during the study, as has been shown in [Table/Fig-5].
Quinolones: Among the quinolones which were tested, cipro- floxacin showed the highest resistance towards a majority of the isolates, except for Pseudomonas aeruginosa (23.9%). This was in correlation with the findings of Nidhi Goel et al., [4].
Levofloxacin demonstrated a lesser resistance rate in comparison to ciprofloxacin and ofloxacin among all the isolates, except for Pseudomonas aeruginosa, where ciprofloxacin was found to have a comparatively lesser resistance rate (as shown in [Table/Fig-2], which was in contrast to that which was reported by V. Olugbue, et al., in which the least sensitivity was shown by Pseudomonas aeruginosa (36.4%) as compared to other isolates [3].
Cephalosporins:Klebsiella pneumoniae showed high resistance to all the drugs, with the highest resistance to ceftazidime (84.1%), which was similar to that which was reported by V.OLugbue, et al., which showed 100% resistance [3] and the least resistance to ceftriaxone (76.5%). Pseudomonas aeruginosa showed the highest resistance to cefuroxime (97.1%) and the least to ceftazidime (57.1%), as was also reported by Kaul et al.,[10].
Acinetobacter baumanii showed the highest resistance to cefuroxime and ceftazidime (100%) and the least to ceftriaxone (94.4%). Citrobacter koseri showed the highest resistance to cefuroxime (78.9%) and the least to ceftriaxone (64.7%). On the whole, ceftazidime was the better choice of treatment in the Pseudomonas aeruginosa and Escherichia coli infections, whereas ceftriaxone was found to be a better choice against Klebsiella pneumoniae, Acinetobacter baumanii and Citrobacter koseri.
Aminoglycosides: Amikacin showed a relatively higher resistance in Acinetobacter baumanii (61.9%),in contrast to that which was reported by Nidhi Goel et al.,[4], followed by Klebsiella pneumonia (34.3%) and the least resistance to Citrobacter koseri (10%) and Escherichia coli (7.2%), followed by Pseudomonas aeruginosa (13.5%). This was a far lesser resistance than that which was reported by Nidhi Goel et al.,[4].
Monobactums: Aztreonam: the resistance rate which was shown by aztreonam with respect to Klebsiella pneumonia, E.coli, Acinetobacter baumanii and Citrobacter koseri was as follows: 88.9%, 80%, 90.9% and 66.7% respectively, whereas Pseudomonas aeruginosa showed nil resistance.
Carbapenems: Imipenem showed high resistance in Klebsiella pneumoniae (7.8%), Citrobacter koseri (6.7%) and in Acinetobacter baumanii (4.8%) and no resistance in Pseudomonas aeruginosa and Escherichia coli (0%). This was very less than that which was reported by Nidhi Goel et al.,[4].
Betalactum/Betalactum inhibitors:Pseudomonas aeruginosa, Acinetobacter baumanii, Klebsiella pneumoniae, Citrobacter koseri, Escherichia coli and Moraxella catarrhalis showed the highest resistance to amoxyclav (100%, 100%, 91.7%, 75%, 68.8%, and 50% respectively) and the least resistance to piperacillin/tazobactum, as shown in [Table/Fig-5]. This shows that piperacillin/tazobactum is the best combination for treating LRTIs which are induced by gram negative bacilli, as was also reported by Manjari Joshia et al., [12] in contrast to the higher resistance which was reported by Nidhi Goel [4].
CONCLUSION
The emergence of resistant strains poses a major threat to the patients globally. Inappropriate and irrational drug usage should be avoided. Owing to the increased concern which surrounds antibiotic resistance and the changing patterns of both viral and bacterial pathogens, the ongoing surveillance of disease and a regular review of the management guidelines are critical. Educational campaigns have quite sensibly tried to convince both the doctors and the general public about the need to use an appropriate, evidence based, antibiotic treatment policy which is based on the infective organism. Ongoing community based studies are needed to identify the best management for individual patients. The therapy should be based on the identification of the at risk patients, an aggressive diagnostic work up and the broad spectrum antimicrobial treatment which is guided by microbiological support.