The supra scapular notch is situated in the lateral part of the superior border of the scapula, adjacent to the base of the coracoid process. The notch is converted into a foramen by the transverse scapular ligament and it serves as a passage for the suprascapular nerve. Suprascapular nerve entrapment is an acquired neuropathy which is secondary to the compression of the nerve, in the bony suprascapular notch [1, 2]. The suprascapular notch is an important landmark of the suprascapular nerve during arthroscopic shoulder operations [3, 4]. The distance between the suprascapular notch and the margin of the glenoid cavity is critical during open surgical procedures which require dissection of the posterior aspect of the shoulder joint [5, 6]. Knowing the anatomical variations in detail, along the course of the suprascapular nerve, is important for a better understanding of the location and the source of the entrapment syndrome.
The present study was taken up as the literature revealed that only very little data was available on the morphology of the suprascapular notch, particularly in the south Indian population. This study also provided data on the association of the safe zone distance of the suprascapular notch from the margin of the glenoid cavity.
MATERIAL AND METHODS
The present study was carried out on 104 dried scapulae of unknown sex, which were obtained from the Department of Anatomy, NRI Medical College, AP, India and from other nearby medical colleges. The broken scapulae were excluded from the study. The suprascapular notches in the scapulae were classified, based on the descriptions of Rengachary et al., [1] Natsis et al., [7] and Ticker et al. [8] The suprascapular notch of each scapula was measured to check for the following details [Table/Fig-1].
Showing the dimentions suprascapular notch
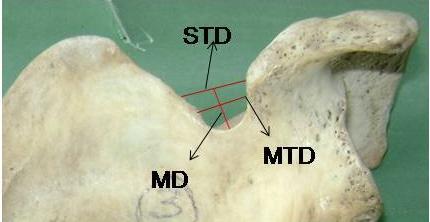
The Superior transverse diameter (STD): The maximum horizontal distance between the superior corners of the notch.
The Middle transverse diameter (MTD): The maximum horizontal distance between the margins of the notch.
Maximum depth (MD): The maximum vertical distance between the deepest point of the notch to the imaginary plane between the superior corners of the notch.
In the scapulae where the notch was absent and in those with a suprascapular foramen, these measurements were not recorded.
The distance between the deepest point of the suprascapular notch and the supra glenoid tubercle [Table/Fig-2], and the distance between the medial wall of the spinoglenoid notch at the base of scapular spine and the posterior rim of the glenoid cavity [Table/Fig-3] were measured.
Showing the distance between suprascapular notch and margin of glenoid cavity

Showing the distance between spinoglenoid notch and the margin of glenoid cavity

The measurements were taken by using slide vernier calipers and they were recorded in millimetres. The data was analyzed statistically.
RESULTS
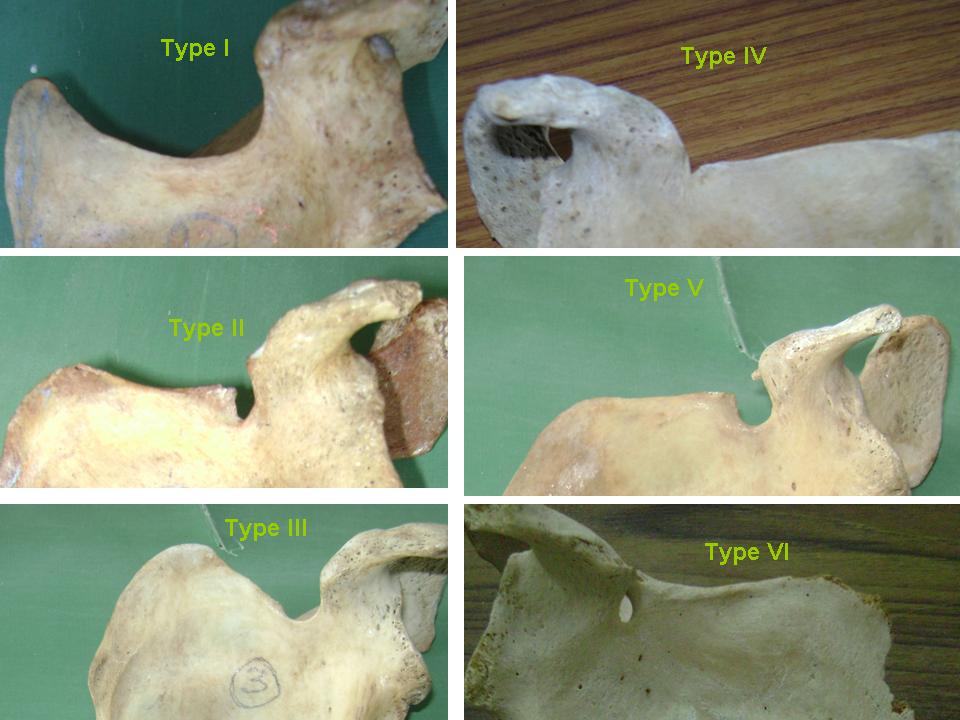
Based on the Rengachary classification, the frequencies of the various types of suprascapular notches which were observed in the present study were as follows: type I – 22/104 (21.15%), type II – 9/104 (8.65%), type III – 62/104 (59.61%), type IV – 3/104 (2.88%), type V – 6/104 (5.76%) and type VI – 2/104 (1.92%). U - type notches were observed in 76 (73.07%) scapulae and V – type notches were observed in 28 (26.92%) scapulae [Table/ Fig-4]. A partial ossification of the ligament was observed in 6 (5.76%) scapulae and a complete ossification of the ligament ie. a suprascapular foramen was observed in 2 (1.93%) scapulae.
Showing types of Suprascapular notches based on Rengachary classification
[Table/Fig-5] shows the dimensions of various types of suprascapular notches. In 59 (56.73%) scapulae, the STD was more than the MD, in 15 (14.42%), the STD was less than the MD and in 6 (5.76%) scapulae, the STD was equal to the MD.
Dimensions of various types suprascapular notches
| Type of notch (Rengachary Classification) | Superior transverse diameter (STD) Mean ± SD | Middle transverse diameter (MTD) Mean ± SD | Maximum depth (MD) Mean ± SD |
|---|
| I | - | - | - |
| II | 8.58 ±1.82 | 4.73 ± 1.45 | 6.5 ± 1.57 |
| III | 10.63 ± 3.06 | 8.65 ± 2.57 | 7.11 ± 2.41 |
| IV | 2.64 ± 0.68 | 1.75 ± 0.63 | 2.06 ± 0.33 |
| V | 5.65 ± 0.9 | 7.6 ± 1.92 | 9.09 ± 2.69 |
| VI | - | - | - |
The distance between the suprascapular notch and the supraglenoid tubercle varied with the type of notch, but the difference was not statistically significant. The mean distance was 29.06 ± 2.9 mm. Minimum distances were observed in the scapulae with the types III and II notches. The least mean distances were observed in the types II and IV scapulae. [Table/Fig-6] shows the details of the distance between the suprascapular notch and the supraglenoid tubercle in various types of notches.
Distance between suprascapular notch and supraglenoid tubercle in various types of notches.
| Type of notch (Rengachary Classification) | Mean ± SD | Range |
|---|
| I | 28.9±2.37 | 24.62 – 32.34 |
| II | 27.12±4.2 | 20.16 – 33.3 |
| III | 29.53±2.4 | 19.86 – 36.4 |
| IV | 27.77±3.7 | 23.57 – 32.64 |
| V | 28.57±2.5 | 25.1 – 32.11 |
| VI | 28.17 ±0.57 | 27.6 – 28.74 |
The mean distance between the posterior rim of the glenoid cavity and the medial wall of the spinoglenoid notch was 16.31 ± 1.84 mm. Minimum distances were observed in the scapulae with the types I, III and V notches. The least mean distance was observed in the type IV scapulae. [Table/Fig-7] shows the details of the distance between the posterior rim of the glenoid cavity and the medial wall of the spinoglenoid notch in various types of notches.
Distance between posterior rim of glenoid cavity and medial wall of spinoglenoid notch in various types of notches.
| Type of notch (Rengachary Classification) | Mean ± SD | Range |
|---|
| I | 16.4 ±2.08 | 12.59 – 21.19 |
| II | 17.66 ±1.6 | 14.86 – 19.64 |
| III | 16.03 ± 1.55 | 12.42 – 21.09 |
| IV | 14.81 ± 0.42 | 14.21 – 15.12 |
| V | 16.44 ± 1.89 | 13.92 – 19.05 |
| VI | 20.2 ± 0.7 | 19.5 – 20.91 |
DISCUSSION
Several descriptions of the suprascapular notch variations have been studied in different populations - Hrdicka [9], Olivier [10], Rengachary et al., [1, 2] Ticker et al., [8] Bayramoglu et al., [11] Natsis et al., [7] Sinkeet [12], Wang [13] and Polguj [14]. A difference in the classification of the notches had been mentioned by earlier authors. Rengachary et al., [1, 2] classified the suprascapular notch into six types, based on its shape. Type I – the entire superior border of the scapula shows a wide depression from the medial superior angle to the base of the coracoid process, type II – a wide, blunt, v-shaped notch, type III – a symmetrical, u-shaped notch with parallel margins, type IV – a small, v-shaped notch, type V – similar to type III with the medial part of the ligament ossified and type VI – with the ligament completely ossified and forming a foramen [Table/Fig-4]. In the present study, the type III notch was more common and this observation was similar to that of other studies. The second common type was type I, which was similar to the observation of Sinkeet et al., [12] but it differed from the findings of Rengachary et al., [1, 2] and Natsis et al., [7] who described type II as the second common type of notch. Type VI is the least common type and this finding was similar to that of Rengachary et al., [1, 2] and Sinkeet et al., [12]. [Table/Fig-8] shows the comparison of the frequencies of various types of suprascapular notches in different populations, based on the Rengachary classification.
Comparison of frequency of various types of suprascapular notches in different populations based on Rengachary classification.
| Type of notch | Rengachary et al (America) [1, 2] | Natsis et al (Greek) [7] | Sinkeet et al (Kenya) [12] | Present study (India) |
|---|
| I | 6% | 8% | 22% | 21.15% |
| II | 24% | 31% | 21% | 8.65% |
| III | 40% | 48% | 29% | 59.61% |
| IV | 13% | 3% | 5% | 2.88% |
| V | 11% | 6% | 18% | 5.76% |
| VI | 6% | 4% | 4% | 1.93% |
Natsis et al., [7] proposed a classification which was based on a study which was done on 423 scapulae. Type I – without a discrete notch, type II – a notch with the longest transverse diameter, type III – a notch with the longest vertical diameter, type IV – a bony foramen and type V – a notch and a foramen. In the present study, the presence of both the notch and the foramen was not observed. [Table/Fig-9] shows the comparison of the frequencies of various types of suprascapular notches in different populations, based on Natsis et al’s classification.
Comparison of frequency of various types of suprascapular notches in different populations based on Natsis et al classification.
| Type of notch | Natsis et al (Greek) [7] | Wang (Chinese) [13] | Present study (India) |
|---|
| I | 8.3% | 28% | 21.25% |
| II | 41.85% | 58.16% | 56.73% |
| III | 41.85% | 28.23% | 14.42% |
| IV | 7.3% | 3% | 1.92% |
| V | 0.7% | - | - |
In the present study, the STD of the notch was more than the MD in 56.73% scapulae, the STD was less than the MD in 14.42% and the STD was equal to the MD in 5.76% scapulae. In 23.06% scapulae, the dimensions could not be determined. [Table/Fig-10] shows the comparison of the dimensions of the suprascapular notch in different populations.
Comparison of dimensions of suprascapular notch in different populations.
| Study | STD>MD | STD<MD | STD=MD |
|---|
| Rengachary (America) [1,2] | 31% | 48% | - |
| Natsis (Greek) [7] | 41.85% | 41.85% | - |
| Ticker (America) [8] | 33% | 31% | - |
| Urguden (Turkish) [16] | 24% | 40% | - |
| Polguj (Poland) [14] | 57.7% | 24.4% | 2.3% |
| Present study (India) | 56.73% | 14.42% | 5.76% |
Dunkelgrun et al., [15] stated that the U-shaped notch had a large area than the V-shaped notch, leading to an assumption that the V-shaped notch was more likely to be connected with the nerve entrapment. In the present study, the U-shaped notch was more common (69.23%) than the V-shaped notch (26.92%). This finding was similar to those of various other studies, as has been shown in [Table/Fig-11].
Comparitive distribution U and V type of notches in different studies
| Study | U-type | V-type |
|---|
| Ticker et al [8] | 77% | 23% |
| Bayramoglu [11] | 62.5% | 25% |
| Duparc [17] | 63.3% | 36.7% |
| Present study | 69.23% | 26.92% |
A complete ossification of the superior transverse scapular ligament, which converted the notch into a foramen, was observed in 2/104 (1.93%) scapulae in the present study. The literature revealed that the incidence of the suprascapular foramen was different in different populations. [Table/Fig-12] shows the comparative distribution of the suprascapular foramen in different populations.
Comparative distribution of suprascapular foramen in different populations.
| Population | Author | Presence of notch |
|---|
| French | Olivier [10] | 5 – 6.5% |
| Italian | Vallois [18] | 6.1% |
| Greek | Natsis [7] | 7.3% |
| Turkish | Urguden [16] Bayramoglu [11] | 6 – 12.5% |
| America | Edelson [19] Tubbs [20] Rengachary [1, 2] | 3.7% 3.7% 4% |
| Alaskan Eskimos | Hrdicka [9] | 0.3% |
| Native America | Hrdicka [9] | 2.1 – 2.9% |
| India | Present study | 1.93% |
The distance between the suprascapular notch and the margin of the glenoid cavity is critical during open surgical procedures which require dissection of the posterior shoulder joint, as has been described by De Mulder et al., [5] and Warner et al. [6] In order to avoid injuries to the suprascapular nerve during these procedures, a safe zone has been described, based on the critical distance within which they can be done safely [3]. It has been reported that 2.3 cm. from the glenoid rim, at the level of the superior rim of the glenoid and 1.4 cm. from the posterior rim of the glenoid, at the level of the base of the scapular spine are safe. In the present study, the mean distances were 2.9 cm. and 1.6 cm. respectively. But 3/104 (2.88%) and 9/104 (8.65%) scapulae fell short of the respective critical distances which have been mentioned for the safe zones. A similar study was carried out by Sinkeet et al., [12] in the Kenyan population, which described that 5.9% and 12% scapulae fell short of the critical distances respectively. Urguden et al., [16] described that the type IV scapular notches had the lowest distance between the notch and supraglenoid tubercle. This implies that the defined safe zone may be inadequate for avoiding suprascapular nerve injuries during shoulder procedures. Hence, there is a need to take extra care during shoulder procedures, to avoid nerve injuries.
CONCLUSION
A study on the morphology of the suprascapular notch is useful, as the notch is the common site of nerve compression. The type of notch may be the cause of a nerve entrapment. The determination of the notch type, particularly in rotator cuff tears, is helpful in avoiding iatrogenic nerve lesions. A study on the safe zone distances is of surgical importance in avoiding injuries to the suprascapular nerve during shoulder procedures.