Acute Myeloid Leukaemia (AML) Presenting as a Bilateral Pleural Effusion
Ranjan Agrawal1
1 Associate Professor, Department of Pathology,
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjan Agrawal, Associate Professor, Department of Pathology, Rohilkhand Medical College Hospital, Pilibhit Byepass Road, Bareilly, India. Mobile: 9412291009; Email: drranjan68@gmail.com
Haematologic malignancies, especially leukaemias, rarely present with or develop pleural effusions during the clinical course of the disease. We are reporting a patient with acute myeloid leukaemia, who presented with a bilateral pleural effusion. There was no symptom which was related to leukaemia at the time of presentation [1,2].
A 45 year old, non-smoker male was admitted with a history of dyspnoea of 2 months duration, which was insidious in onset and gradually progressive in nature. Lately, he had started having orthopnoea. There was a history of fever but he had no chest pain, cough or wheezing. He had loss of appetite with mild weight loss. The patient stated that his family physician had put him on antitubercular therapy for bilateral pleural effusion since past 1 month and that his symptoms had not been relieved. On examination, the patient was found to have tachypnoea and tachycardia. There was no sternal tenderness, gum hypertrophy, purpuric spots or organomegaly. His chest examination showed a bilateral pleural effusion, which was further confirmed by X-ray.
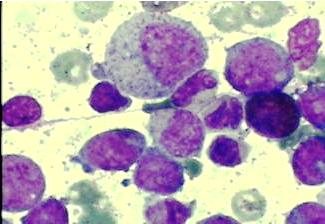
On investigation, his Hb was found to be 8.6 g%, TLC 86000/ mm3, and platelet count 37000/mm3. The peripheral smear showed 92% myeloblasts that were myeloperoxidase positive and PAS negative. His biochemical investigations were within normal limits. Pleural tapping showed a haemorrhagic fluid with a protein content of 4.2 gm%, and his cytology showed predominantly small mature lymphocytes, few mesothelial cells and RBCs. The myeloblasts were lying discretely and in small clusters in the pleural fluid [Table/Fig-1]. The patient was subjected to bone marrow aspiration from the posterior superior iliac spine. It showed a markedly increased cellularity with an M:E ratio of 11:1. The myelopoiesis was markedly increased with myeloblasts, few of which showed the presence of “Auer Rods”. A diagnosis of acute myeloid leukaemia (M2- FAB classification) was made. The cause of the pleural effusion was thus established. An induction chemotherapy was started, but the patient expired a week later.
Pleural fluid cytology showing myeloblasts (Leishman-Giemsa, 400 X).
Granulocytic sarcoma occurs in 3-7% cases of AML and it can present before, during, or even after the diagnosis of AML. Different organs can be involved individually or simultaneously, which include the skin, lymph nodes, bone, breast, the CNS and the lungs. Pleural effusions may be the first presentation of the haematological malignancies or they may develop during the course of the disease. The acute and chronic leukaemias are rarely accompanied by pleural effusions. Besides the direct infiltration of leukaemic cells into the pleura, the pleural effusions can be secondarily caused by drug toxicity, underlying infections or by metastatic or rarely autoimmune causes in haematologic malignancies. In most of the cases, the pleural fluid responds to the treatment of the primary disease, whereas the resistant or the relapsing cases may necessitate a pleurodesis [1].
An extramedullary relapse is a recurrence of the leukaemia in sites other than the bone marrow. It is known to recur ‘isolated’ without any recurrence in the bone marrow [2].
[1]. Raina S, Kaul R, Mahesh DM, Kaushal SS, Gupta D, Sharma. J, Pleural effusions in acute myeloid leukaemiaJAPI 2008 56:194 [Google Scholar]
[2]. Alexandrakis MG, Passam FH, Kyriakou DS, Bouros D, Pleural effusions in hematologic malignanciesChest 2004 125:1546-55. [Google Scholar]