Squamous Cell Carcinoma Arising in Warthin’s Tumour: A Case Report
P J Yaranal1, Umashankar T2
1 Associate Professor, Department of Pathology, Yenepoya Medical College, Mangalore - 575018, India.
2 Associate Professor, Department of Pathology, Yenepoya Medical College, Mangalore - 575018, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Umashankar T, Associate Professor, Department of Pathology, Yenepoya Medical College, Mangalore - 575018, India.
Phone: 9880568839
E-mail: tumashankar@hotmail.com
Warthin’s tumour (adenolymphoma) is a well defined salivary gland tumour which consists of epithelial and lymphoid components. However, the malignant transformation of adenolymphoma is extremely rare. We are reporting a case of squamous cell carcinoma which arose in a Warthin’s tumour of the right parotid gland, to highlight its varied cytolomorphological features which can cause diagnostic problems on cytological examination. The review of the literature has been discussed.
Squamous cell carcinoma, Warthin’s tumour, Parotid gland
INTRODUCTION
Warthin described Warthin’s tumour (adenolymphoma) in 1929 [1]. Warthin’s tumour is the second most common benign neoplasm of the salivary glands and it accounts for 5% - 10% of all the parotid tumours. Warthin’s tumour is more common in men, with a peak incidence in the seventh decade and it is associated with cigarette smoking. The tumour is usually an asymptomatic and a slow growing painless mass and it is bilateral in about 10% of the cases [1–5].
Sudden increase in its size is attributable to a malignant change or inflammation [1,2,4]. The malignant transformation of Warthin’s tumour is extremely rare (0.3%). The malignant transformation of its lymphoid component into malignant lymphoma is relatively common, whereas, an epithelial malignancy in Warthin’s tumour is extremely rare [3,4]. Till date, only 32 cases of epidermoid carcinoma have been reported to arise in Warthin’s tumour [3]. We are reporting one such case of squamous cell carcinoma which arose in a Warthin’s tumour in the parotid gland and also to highlight the diagnostic problems which are faced on its cytological examination.
CASE REPORT
Clinical findings: A 65-year-old male presented with a painless mass in the right preauricular region. It had been present for the past one year, but it had increased in size over the past three months. On examination, a non-tender well defined lump which measured 4x3cm in size was seen in the right parotid region and it was partly fixed to the underlying structures. Clinically, there was no evidence of facial nerve involvement or regional lymphadenopathy. The haematological and biochemical investigations were within normal limits. The patient was referred for Fine Needle Aspiration Cytology (FNAC) with the clinical impression of a secondary tumour in the right cervical lymph node. FNA was performed and a few drops of thin watery to mucoid material was obtained. Smears were prepared from it and they were fixed in alcohol and stained with Papanicolaou’s stain.
Cytological findings: The smears showed scattered epithelial cells which were arranged in clusters or nests in a diffuse inflammatory and necrotic background. Some epithelial cells had a squamoid appearance which showed variable sized bizarre shaped nuclei. They had a moderate amount of dense eosinophilic keratinized cytoplasm. A cytological diagnosis of metastatic squamous cell carcinoma was suggested and the patient was advised excision biopsy.
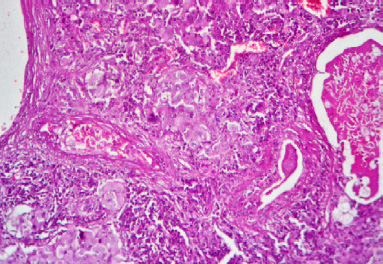
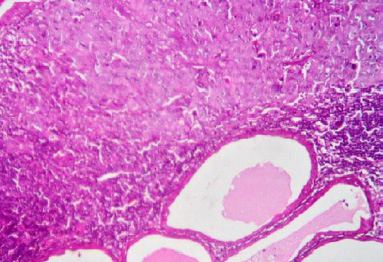
Histopathology findings: Subsequently, the mass was excised and it was submitted for histopathological studies. Grossly, the specimen consisted of a globular grey-white mass which measured 2x1x1cm. The cut surface showed both solid and cystic areas. The haematoxylin and eosin (H and E) stained sections showed the classical features of Warthin’s tumour with islands of malignant squamous epithelial cells which were found to invade the lymphoid stroma and the cells showed atypical features with a high nucleocytoplasmic ratio, prominent nucleoli and keratinization of the cytoplasm [Table/Fig-1] and [Table/Fig-2]. A histological diagnosis of Warthin’s tumour with squamous cell carcinoma was made.
Section shows Warthin tumor with infiltration of stroma by malignant squamous cells. (H&E, X400)
Section shows Warthin tumour with infiltration of lymphoid stroma by malignant squamous cells. (H&E, X400)
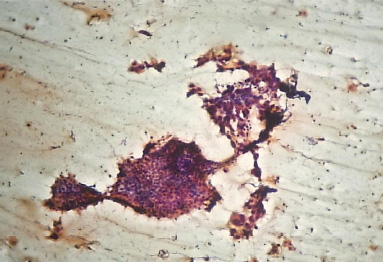
In view of this histological report, the FNAC smears were reviewed thoroughly, that showed occasional flat, irregular sheets of polyhedral and finely granular oncocytic cells with well defined cell borders, in addition to malignant squamous epithelial cells. These cells were arranged in honeycomb patterns in a lymphatic background. A final diagnosis of squamous cell carcinoma which arose in a Warthin’s tumour was made [Table/Fig-3].
Cytology smear shows pleomorphic malignant squamous cells with honey- comb pattern of oncocytes in a lymphoid background. (H&E, X400)
DISCUSSION
Warthin’s tumour occurs frequently in the inferior pole of the parotid glands and the periparotid lymph nodes [3]. The histopathology of Warthin’s tumour is highly distinctive; yet FNAC fails to detect the lesion in up to 20% of the cases. Most often, this relates to a sampling error i.e. failure of FNAC to yield diagnostic oncocytes. In some cases, its detection is precluded by extensive necrosis of the oncocytic epithelium or by replacement of the oncocytic epithelium by a metaplastic mucinous or a squamous epithelium [4].
The cytological appearance of Warthin’s tumour is characterized by cellular debris which is mixed with lymphocytes and oncocytes [6]. This is not a consistent finding. In their review of 16 fine-needle aspiration biopsies of histologically confirmed Warthin’s tumours, Ballo et al. found that 13(81%) had typical features and that three cases showed a predominance of the lymphoid component, squamous cells and necrotic/mucoid debris. This creates a significant diagnostic challenge because the squamous element in particular, is common to squamous cell carcinoma and mucoepidermoid carcinoma [7]. The sensitivity, specificity and the diagnostic accuracy of FNAC in diagnosing Warthin’s tumour ranges from 74% to 100% [6].
In our case, a diagnosis of squamous cell carcinoma was made histologically, due to the invasive nature of the squamous cells with nuclear atypia, which had the classical features of Warthin’s tumour. A histopathologic examination alone could not fully characterize the pre-existing tumour to be a Warthin’s tumour. This possibility can be confirmed by immunohistochemical stains like EMA, CEA and the secretory component of IgA, which were positive for epithelial cells and the lymphocyte- rich stroma which were positive for CD45, which were used to establish the diagnosis [8].
The pathogenesis of the development of malignant tumours in preexisting Warthin’s tumours is uncertain, but Damjanov et al [9] reported a case and demonstrated on an ultrastructural level, a gradual transition from the cylindrical cells with keratin cytoskeleton which were rich in mitochondria, to flattened squamous cells with few cytoplasmic organelles. They postulated that squamous carcinomas arose from a focus of squamous metaplasia [9]. The presence of keratin in the cytoplasm of the Warthin’s tumour cells may provide a clue to the case with which these cells undergo squamous metaplasia [10]. The transition from cylindrical cells to squamous cells may be due to infection or ischaemia and necrosis in a large tumour. Ischaemia was thought to be the most probable aetiology for squamous metaplasia [8].
A malignant change in a Warthin’s tumour is suggested clinically by a recent history of a rapid enlargement of a longstanding mass [4] This was noted in the present case as well as in the patients which were described by Damjanov et al [9].
The presence of transitional zones right from the benign oncocytic component to the frank malignant epithelium is important to be distinguished from the metastasis of primary carcinoma at another site [9]. In most of the reported cases, a distant metastasis is rare, however, a regional lymph node metastasis is common [3,8]. We did not discover any distant or lymph node metastasis in the present case and the patient was found to be disease free at the 12- month follow-up, following complete surgical excision.
CONCLUSION
This case highlights the pitfalls in the clinical and the cytologic recognition of malignant changes in Warthin’s tumours. The cytopathologists should have adequate awareness to make an FNAC diagnosis of the malignant transformation of Warthin’s tumour. They can be confuse it with a secondary tumour from a squamoid carcinoma in a lymph node. It is therefore important for the clinician to make appropriate decisions.
[1]. Auclair PL, Ellis GL, Gnepp DR, Other benign epithelial neoplasmsSurgical Pathology of the Salivary Gland Edited by: Ellis GL, Auclair PL, Gnepp DR 1991 PhiladelphiaWB Saunders Company:252-68. [Google Scholar]
[2]. Siefert G, Carcinoma in pre-existing Warthin’s tumors (cystadenolymphoma) of the parotid gland. Classification, pathogenesis and differential diagnosisPathologies 1997 18:359-67. [Google Scholar]
[3]. Sharama M, Saxena Chintamani S, Agrawal S, Squamous cell carcinoma arising in unilateral Warthin’s tumour of the parotid glandJournal of Oral and Maxillofacial Pathology 2008 12:82-4. [Google Scholar]
[4]. Cob CJ, Greaves TS, Raza AS, Fine needle aspiration cytology and the diagnostic pitfalls in Warthin’s tumour with necrotizing granulomatous inflammation and facial nerve paralysisActa Cytol. 2009 53:431-4. [Google Scholar]
[5]. Mukunyadzi P, Review of the fine needle aspiration cytology of salivary gland neoplasms, with emphasis on differential diagnosesAm J Clin Pahtol. 2002 118(suppl 1):S100-S115. [Google Scholar]
[6]. Thangarajah T, Reddy VM, Castellanos-Arango F, Panarese A, Current controversies in the management of Warthin’s tumourPostgrad Med J. 2009 85:3-8. [Google Scholar]
[7]. Ballo MS, Shin HJ, Sneige N, Sources of diagnostic error in the fineneedle aspiration diagnosis of Warthin’s tumour and the clues to a correct diagnosisDiagn Cytopathol. 1997 17:230-4. [Google Scholar]
[8]. Gunduz M, Yamanaka N, Hotomi M, Kuki K, Yokoyama M, Nakamine H, Squamous cell carcinoma arising in Warthin’s tumourAuris Nasus Larynx 1999 26:355-60. [Google Scholar]
[9]. Damjanov I, Sneff EM, Delerme AN, Squamous cell carcinoma arising in unilateral Warthin’s tumour of the parotid gland; A light electron microscopic and immunohistochemical studyOral Surg Oral Med Oral Pathol 1983 55:286-90. [Google Scholar]
[10]. Therkildsen MH, Christensen N, Andersen LJ, Larsen S, Katholm M, Malignant Warthin’s tumour: A case studyHistopathology 1992 21:167-71. [Google Scholar]