An interstitial ectopic pregnancy is a rare and a dangerous form of an ectopic pregnancy. It presents late clinically and it is difficult to be imaged radiographically. We are presenting a case of an interstitial pregnancy which was a surprise intra operative finding.
As Assisted Reproductive Technology (ART) procedures are becoming popular, the incidence of ectopic pregnancies is likely to increase. The clinicians should be well equipped to diagnose and to treat this unusual form of ectopic pregnancies at the earliest.
Interstitial pregnancy, Cornual ectopic pregnancy
INTRODUCTION
An ectopic pregnancy is one of the most common gynaecological emergencies. Ectopic pregnancies comprise 2% of all the pregnancies. The myriad of locations have a hierarchy on the prevalence as well as the associated mortality and morbidity [1].The most common location of the ectopic pregnancies continues to be fallopian tubes (accounting for roughly 95% of all the ectopic pregnancies), followed by the far less common interstitial ectopic pregnancies which comprise 2-4% of all the extrauterine cavity pregnancies [2]. This condition occurs once in every 2500-5000 live births [2]. The interstitial part of the fallopian tube is the proximal portion that lies within the muscle wall of the uterus. It is 0.7 mm wide and 1-2 cm long, with a slightly tortuous course upwards and outwards from the uterine cavity.
Although the term ‘interstitial’ and ‘cornual’ ectopic pregnancies are used interchangeably, there is a specific difference. An interstitial pregnancy refers to an ectopic location of the gestational sac in the intramyometrial segment of the fallopian tube in a normally configured uterus, while a cornual pregnancy pertains to an ectopic location of the gestational sac in the cornu of a bicornuate uterus. An interstitial pregnancy should also be differentiated from an angular pregnancy. An angular pregnancy occurs when an embryo gets implanted in the lateral angle of the uterine cavity, medial to the internal ostium of the fallopian tube [2].
CASE REPORT
A 26 year old lady presented to the emergency department with the complaint of a sudden onset, severe pain in the abdomen, of 2 hours duration. She was known to be 2 months pregnant, but was unsure of the dates of her last menstrual period. She was gravid 2 and parity 1, with the history of a spontaneous vaginal delivery 1 year back. She was breastfeeding her one year old child. She was haemodynamically unstable. There was tachycardia and hypotension. Lower abdomen tenderness, rigidity and guarding were present. The speculum examination was normal. The vaginal examination revealed tenderness in the bilateral fornices. Her urinary human chorionic gonadotropin value was positive.
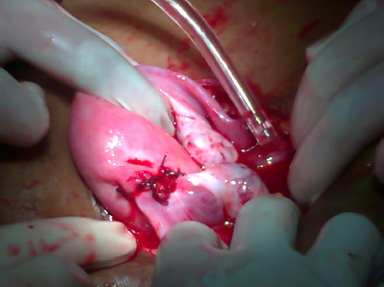
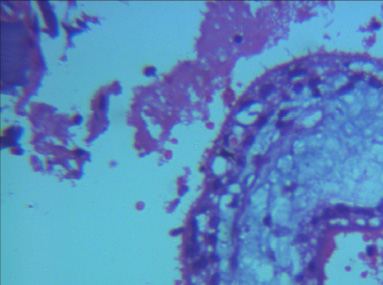
Pelvic ultrasonography revealed an empty uterine cavity and haemoperitoneum. A pelvic CT scan which was done, did not reveal the location of the pregnancy. An emergency laparotomy was done. A ruptured left interstitial tubal ectopic was found [Table/Fig-1]. The abdomen was filled with 1500 ml of fresh blood clots. Left uterine artery ligation was done and the interstitial tube defect was repaired in two layers [Table/Fig-2]. The haemostasis was secured. The patient had an uneventful post operative course. The histopathological study of the excised specimen showed chorionic villi [Table/Fig-3]. She was discharged after the normalization of her serum hCG levels. The patient was advised barrier contraception for two years to maintain the inter pregnancy interval.
Intra operative photograph of ruptured left uterine cornu

Intra operative photograph of repaired left uterine cornu
Microscopic histopathology of chorionic villi in the shelled out gestational sac from the tubal interstitium
DISCUSSION
There is often a delay in the diagnosis of an interstitial pregnancy, as this segment has increased distensibility, leading to less pain. In our patient, the diagnosis of an interstitial ectopic pregnancy was missed on ultrasonography and pelvic CT scan. It was a surprise intra operative finding. It poses a significant diagnostic and s therapeutic challenge and it carries a greater maternal mortality risk than an ampullary ectopic pregnancy. After 2-3 months of amenorrhoea, the vaginal spotting commonly begins. The developing chorionic villi may eventually erode into the blood vessels of the cornu, causing a severe haemorrhage. An interstitial pregnancy occurs at the most richly vascularized site of the female pelvis, the junction of the branches of the uterine and the ovarian arteries. The significant maternal haemorrhage which leads to hypovolaemia and shock, can rapidly result from an interstitial pregnancy rupture [2]. The Maternal And Child Health Report for 2000-02 in Black pool, Victoria Hospital, UK, stated that 4 out of 11 deaths from ruptured ectopic pregnancies were due to interstitial pregnancies [3]. The haemorrhage can be severe because an interstitial tubal pregnancy is often more developed than an extra uterine tubal pregnancy. It presents late and the blood supply is large. The clinicians should be aware of the difficulties which are faced in both the clinical and the radiological diagnoses.
The aetiological factors of an interstitial pregnancy are pelvic in- flammatory diseases, fibroids, a previous pelvic surgery and the use of ART procedures [2]. A high number of transferred embroyos, a transfer near the uterine horn, excessive pressure on the syringe during the transfer or the difficulties which are encountered during the embryo transfer procedure increase the risk [4]. Bilateral salpingectomy is likely to be another risk factor [5]. For the nonsalpingectomized patients, the peri and the intra tubal adhesions which are related or not related to endometriosis, are an additional risk factor. Certain authors also consider the quality of the embryos and the hormonal milieu at the moment of the transfer as a possible cause [6]. With the increasing use of ART procedures, the clinicians should be equipped with skills to diagnose this evasive form of ectopic pregnancies as early as possible. The present maternal mortality rate is 2-2.5 % for all the interstitial ectopic pregnancies.
The diagnosis of an interstitial pregnancy is made by a critical evaluation of all the criteria which are used for other types of tubal pregnancies. The symptoms are acute abdominal pain, intraperitoneal bleeding, a low hematocrit value and a positive serum or urine pregnancy test. The diagnostic tests include the sensitive beta-HCG radioimmunoassay, culdocentesis and ultrasonography. An interstitial pregnancy is diagnosed with the ultrasonographic criteria in the presence of a positive HCG level, which indicates a pregnancy [7].
Timor Trisch and colleagues established the transvaginal ultrasound criteria for interstitial pregnancies [8]. These criteria include a) an empty uterine cavity b) a chorionic sac which is seen separately and which is less than 1 cm from the most lateral edge of the uterine cavity and c) a thick myometrial layer which surrounds the chorionic sac. All these parameters are relatively specific (88%- 93%), but they lack the sensitivity (only about 40%) which is required for the diagnosis of an interstitial pregnancy [2]. Ackerman et al have described the “interstitial line sign” [9]. A thin echogenic line extends directly upto the centre of the interstitial gestational sac. This represents either the endometrial cavity or the interstitial portion of the fallopian tube, depending upon the size of the interstitial chorionic sac. A transvaginal, three dimensional ultrasound scanning can reproduce the coronal plane of the uterus and it can facilitate the exact localization of the gestational sac which is relative to the uterine cornu.
The features that are helped with the use of the 3-dimensional Trans Vaginal Ultrasonography (TVS) include a live embryo in a gestational sac which is surrounded by the myometrium. It lies below the cornu and outside the endometrium [10]. Another diagnostic aid is laparoscopy, which has the advantage of allowing both the diagnosis and the treatment. One study has shown that an early diagnosis of an interstitial pregnancy with TVS allows a first trimester conservative management with methotrexate. However, if the diagnosis is made later in the gestation, as in our patient, a surgical treatment with cornual repair, resection or even hysterectomy may be required [11].
The Royal College of Obstetricians and Gynaecologists recommends that the women with tubal pregnancies who are most suitable for the methotrexate therapy are those who have serum beta HCG levels of 3000IU/ml and minimum symptoms. There is some evidence which suggests that the women who present with interstitial pregnancies and beta HCG levels of <5000IU/mL can be treated successfully with a single dose of methotrexate [12].
CONCLUSION
The interstitial tubal pregnancies are rare and they can be missed radiologically. The obstetricians may encounter them as surprise intra-operative findings.
LEARNING POINTS
• The interstitial tubal pregnancies are rare and they can be missed radiologically. The obstetricians may encounter them as surprise intra-operative findings.
• Historically, the difficulties which are associated with an early diagnosis of an interstitial pregnancy can be attributed to its location. The eccentric position of the gestational sac and the thinning of the myometrium make the differentiation between the eccentric intrauterine and the interstitial pregnancy difficult. The three dimensional ultrasound has a role in improving the detection rates.
• Assisted reproductive procedures are on the rise. The clinicians should be well aware about diagnosing an interstitial ectopic pregnancy at the earliest.
• In our patient, the interstitial gestation had ruptured and the only option was a cornual repair with a uterine artery ligation.
• Counseling regarding the risk of a rupture of an upper segment uterine scar and the need for a prolonged interpregnancy interval need to be appropriately conveyed to the patients, to help them in making an informed choice about future pregnancies.
CONSENT
We have obtained the patient’s consent for the case report.
COMPETING INTERESTS
We do not have any commercial association that might pose a con- flict of interest in connection with the manuscript. We certify that neither this manuscript nor one with a substantially similar content under our authorship has been published or is being considered for publication elsewhere.
AUTHORS CONTRIBUTION
Dr. Nidhi Sharma carried out the surgery and participated in the sequence alignment and she drafted the manuscript. Dr. G. Rohini also actively participated in the sequence alignment and drafted the manuscript. Dr. Upasana carried out the radiological study for the patient. All the authors read and approved the final manuscript.
[1]. Tulandi T, Al-Jaroudi D, The interstitial pregnancy :results which were generated from the Society of Reproductive Surgeons RegistryObstet Gynaecol. 2004 103:47-50. [Google Scholar]
[2]. Te Linde’s Operative GynaecologyNinthEctopic pregnancy [Google Scholar]
[3]. Faraj R, Steel M, The management of a cornual (interstitial) pregnancyObstetrian Gynaecologist9:245-55. [Google Scholar]
[4]. Chang Y, Lee JN, Yang CH, An unexpected quadruplet hetrotopic pregnancy after a bilateral salpingectomy and the replacement of three embryosFertil Steril. 2003 80:218-20. [Google Scholar]
[5]. Agarwal SK, Wiscot AL, Garzo G, Meldrum DR, Cornual pregnancies in patients with prior salpingectomies who were undergoing in vitro fertilization and embryo transferFertil Steril 1996 65:659-60. [Google Scholar]
[6]. Pan HS, Chuang J, Chiu SF, Hsieh BC, Lin YH, Tsai YL, Huang SC, A hetrotopic triplet pregnancy: the report of a case with a bilateral tubal pregnancy and an intrauterine pregnancyHum Reprod. 2002 17:1363-66. [Google Scholar]
[7]. Graham M, Cooperberg PL, The ultrasound diagnosis of an interstitial pregnancy: the findings and the pitfallsJ. Clin Ultrasound. 1979 7:433-37. [Google Scholar]
[8]. Timor-Tritsch IE, Monteagudo A, Lerner JP, A “potentially safer” route for the puncture and the injection of cornual ectopic pregnanciesUltrasound Obstet Gynaecol. 1997 7:353-55. [Google Scholar]
[9]. Ackerman TE, Levi CS, Dashefsky SM, Holt SC, Lindsay DJ, An interstitial line :sonographic finding in an interstitial (cornual) ectopic pregnancyRadiology 1993 189(1):83-87. [Google Scholar]
[10]. Lee GS, Hur SY, Kown I, The diagnosis of early intramural ectopic pregnancyJ Clin Ultrasound 2005 33:190-92. [Google Scholar]
[11]. Khawajan N, Walsh T, Gill B, A uterine artery ligation for the management of a ruptured cornual ectopic pregnancyEur J Obstet Gynaecol Reprod Biol. 2005 118:269 [Google Scholar]
[12]. The Royal College of Obstetricians and Gynaecologists. The management of a tubal pregnancyGreen Top Guidelines No 21. 2004 London,UKThe Royal college of Obstetricians and Gynaecologists [Google Scholar]